Back to Journals » Research and Reports in Urology » Volume 14
Willingness to Pay and Preferences Among Patients Undergoing Cystoscopies: Results from a Large Survey-Based Study in Spain
Authors Borja Brugés CN , Rindorf DK , Cepeda M, Schultz Hansen K
Received 13 June 2022
Accepted for publication 14 September 2022
Published 18 October 2022 Volume 2022:14 Pages 359—367
DOI https://doi.org/10.2147/RRU.S375582
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Panagiotis J Vlachostergios
Cindy N Borja Brugés,1 Dinah K Rindorf,2 Marcos Cepeda,3 Kristian Schultz Hansen4
1Copenhagen Business School, Frederiksberg, Denmark; 2Ambu A/S, Market Access, Ballerup, Denmark; 3Department of Urology, Hospital Río Hortega de Valladolid, Valladolid, Spain; 4Department of Public Health, University of Copenhagen, Copenhagen, Denmark
Correspondence: Cindy N Borja Brugés, Copenhagen Business School, Solbjerg Pl. 3, 2000, Frederiksberg, Denmark, Tel +45 81710059, Fax +45 72252050, Email [email protected]
Purpose: Cystoscopy procedures can cause distress among patients. Patient perspectives on health services are essential inputs in decision-making. This study investigated the patient preferences in Spain regarding single-use cystoscopes (SUC) compared to reusable cystoscopes and their willingness to pay (WTP) for cystoscopy procedures.
Patients and Methods: Between May and June 2021, an anonymous survey was distributed to Spanish patients who had previously undergone a cystoscopy. The survey included patient preference measures on reusable cystoscopes compared to SUCs and a discrete choice experiment. The survey was distributed through a human data science company (IQVIA), collected using an online survey tool (QuestionPro®), and analyzed using Stata/MP, StataCorp.
Results: Of 300 respondents, 148 (49.33%) were female and 150 (50%) were male, and mainly between 18– 49 years (247, 82.33%). Most (265, 88%) preferred to have their procedure performed with a SUC rather than a reusable cystoscope. Among these patients, 215 (80%) could imagine asking their doctor to use a SUC. A total of 231 (77%) respondents indicated an increased level of concern about the risk of exposure to contamination related to their cystoscopy following the COVID-19 pandemic. Patients would pay 62 EUR to have their initial consultation and cystoscopy procedure on the same day (p < 0.001), 59 EUR to reduce the environmental impact, and 57 EUR to reduce the risk of contamination (p < 0.001).
Conclusion: Patients prefer to undergo cystoscopy using an SUC on the same day as their initial consultation. The increased contamination concerns due to the COVID-19 pandemic and WTP to reduce the risk of cystoscope contamination may explain patients’ preferences for SUCs. The most important attributes related to their cystoscopy procedure are the ability to have their procedure performed on the same day as their initial consultation, the reduction of the environmental impact, and the reduction of the contamination risk.
Keywords: cystoscopy, single-use endoscope, patient preferences, discrete choice experiment, willingness to pay
Introduction
Cystoscopy is a procedure completed by urologist surgeons to identify, screen and treat different conditions that can affect the bladder and urethra. It allows visualization of the urethra, the urethral sphincter, prostate, bladder, and ureteral orifices and can diagnose bladder tumor, stones, benign prostatic hyperplasia, and stenosis among other diseases. For the procedure, a cystoscope is required, and both flexible and rigid device options are available.1 Importantly, the cystoscopy procedure can trigger distress in patients,2 and the level of discomfort and preferences of patients may vary according to their gender and the device used.3 There is an increasing push to involve patients in decision-making4 as their perspectives about experiences, attitudes, preferences, value, and expectations towards health services and treatments are unique and valuable inputs for a health technology assessment.5 Hence, it is important to uncover patients’ preferences in cystoscopy.
In recent years, single-use cystoscopes (SUCs) have entered the market, offering benefits in terms of work-flow efficiency, costs, portability, and elimination of the cross-contamination risk compared to reusable cystoscopes.6–9 Several studies demonstrated less complications after using a disposable device like less UTIs and lower rate of cystoscopy recurrence.10 Some other studies confirmed that quality of the cystoscopies performed is comparable among SUCs and reusable devices.11 Nevertheless, it can be a bit of discussion in terms of image quality.12,13 However, data on patient preferences related to this new technology is limited,8 as well as information about the environmental impact of single-use cystoscopes compared to reusable cystoscopes. Although pain levels have been compared between the use of reusable flexible cystoscopes and SUCs with a relative equivalence of results,14–18 other aspects remain understudied. Therefore, this study sought to explore attributes related to the willingness to pay (WTP) of patients through assessing patients’ preferences regarding cystoscopy procedures in Spain. The main objective of this investigation was to validate patients’ opinions through a robust statistical method to be able to raise patients’ voices within cystoscopy practice.
Materials and Methods
Data Collection and Instrument Design
The study included 300 Spanish patients aged >18 years who had previously undergone ≥1 cystoscopy procedure(s). An electronic survey was conducted in Spanish between May and June 2021. Respondents were recruited by IQVIA (Durham, NC, USA), who shared the online study survey using a software platform tool (QuestionPro®; Survey Analytics LLC, San Francisco, CA, USA), which was compliant with General Data Protection Regulation guidelines. Patients provided informed consent before replying to the survey, and their anonymity was assured. The survey was divided into the following 4 sections: (1) introduction and informed consent; (2) part I (descriptive Information), which included demographic questions; (3) part II (cystoscopy procedures and devices), which included general questions and preferences regarding cystoscopies and devices; and (4) part III (a discrete choice experiment [DCE]), which included an introduction to the task and attributes described. The average estimated time to complete the questionnaire was 8–10 min (See Questionnaire in Appendix 1).
Discrete Choice Experiment
The DCE is a stated preference quantitative technique that allows for individual preferences to be elicited and uncovers the value a respondent places on a specific attribute of a product/intervention plus the trade-offs they would be willing to make.19 During a DCE, the respondents are exposed to several choice sets showing hypothetical alternatives that include several attributes with a variety of levels and are asked to choose the best choice for them. The DCE assumes utility maximization by each respondent. More details on the model can be find in Appendix 2.
Attributes, Levels, and Tasks
Following a patient perspective, the attributes and levels were chosen based on a structured electronic literature search performed in Embase and PubMed using search words related to “cystoscopy”, “contamination”, “patients”, “preferences”, “organizational impact”, and “cost.” The decisions made regarding the choices of attributes and levels were transparent and verified through pilot testing. Five attributes with their respective levels were chosen (Table 1), as follows: (1) direct to cystoscopy,20 (2) risk of cancellation,6,7 (%) (3) contamination risk21–23 (%)(4) negative environmental impact,24 and (5) cost per procedure (in euros [EUR]).10 Range values were avoided in the categories of level selection, as this could allow respondents to interpret the levels subjectively, which might result in ambiguity and affect the results.25
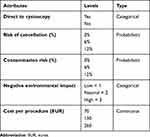 |
Table 1 Attributes and Levels |
A full choice alternative, including all the attributes in 6 choice sets, was presented to the patients (Table 2). The pilot test did not indicate any cognitive fatigue or misunderstanding on the part of the respondents. A forced-choice elicitation format between the 2 alternatives was used. An option for “no preference” was not included.
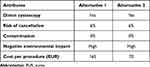 |
Table 2 Example of a Choice Set |
Each attribute was represented as an independent variable. All alternatives were exposed in a factorial, D-optimal design. The cognitive capacity of the respondents was assumed to be healthy. No specific product names/labels were used during the DCE.
Statistical Analysis
The data were imported from QuestionPro® to a dataset-analysis software package (Stata/SE version 16.0; StataCorp LLC, College Station, TX, USA). Twelve tasks were generated by each respondent, for a total of 3600 observations. A chi-squared test was used to estimate the significant difference between the observed and expected values. For the DCE, a conditional logit model was used to estimate the coefficients representing the strength of the preference of the level for each attribute; then, the WTP for each attribute was calculated. A dummy-variable coding method was used. Fourteen variables were considered for the DCE (Appendix A3). The statistical significance was assessed at a 95% confidence interval (CI) with a statistical significance value of p < 0.05.
Ethics
In the legislation presented under §14, stk. 2. regarding research projects using questionnaires, it is stated that research should only be submitted for ethical approval if the project involves human biological material. This study did not involve any data from human subjects; thus, no international review board assessment or approval was required. The study was performed in accordance with the Declaration of Helsinki, and written informed consent was obtained from all participants.26,27
Results
Among the 300 respondents, 148 (49%) were female, 150 (50%) were male, and 2 individuals (0.7%) preferred not to disclose their gender (Table 3). A total of 67 (22%) of the respondents were residents of Madrid, followed in descending order by 59 living in Andalucía (20%), 51 living in Catalunya (17%), 25 living in Comunidad Valenciana (8%), and 15 living in Galicia (5%), respectively.
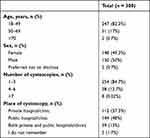 |
Table 3 Descriptive Demographic Data |
A total of 99 (33%) respondents were aged 30–39 years, 79 (26%) were aged 40–49 years, and 69 (23%) were aged 18–29 years, respectively. A total of 144 (48%) of the cystoscopies were performed in public hospitals/clinics compared to 112 (37%) cystoscopies that were performed in private institutions. Patient counts according to the number of cystoscopy procedures and age category can be observed in Figure 1.
 |
Figure 1 Distribution by cystoscopy procedures and age. |
Patients’ Reported Preferences and Concerns
A significantly greater number of respondents (265, 88%) preferred a SUC compared to 35 (12%) who preferred a reusable cystoscope (p < 0.001) (Table 4). A total of 225 (75%) respondents indicated that they would be willing to pay a small additional amount of money for a reusable cystoscope. A total of 215 (72%) respondents reported that they would dare to ask the doctor to use a SUC, and, among these individuals, 154 (51%) indicated that they would be willing to find another hospital/clinic to undergo the cystoscopy with a SUC. In general, out of the 300 respondents 242 individuals (80.67%) would rather have the cystoscopy procedure in the same day instead of in two different days. A total of 246 (82%) respondents are concerned about the risk of a cystoscope being contaminated when receiving a cystoscopy procedure while 54 (18%) respondents are not. 250 (83.33%) of all the respondents believe that receiving a picture or video of the findings of their own cystoscopy is valuable. In contrast, 50 (16.67%) respondents do not believe is valuable. Lastly, 231 (77%) of all respondents showed a high level of concern about exposure to contamination by the cystoscope following the start of the coronavirus disease 2019 (COVID-19) pandemic (p < 0.001). These results are independent of the type of cystoscope to be used.
 |
Table 4 Preferences for Device Type by the Number of Cystoscopies and Type of Cystoscope |
The most common concern regarding reusable cystoscopes was the risk of urinary tract infection (UTI), with 175 (58%) respondents citing this as a concern; a concern about the contamination risk was second, with 158 (53%) respondents citing this as a concern. Additionally, concerns about the performance rate were higher for reusable devices, with 136 (45%) of respondents citing this as a worry. For SUCs, the most common concern was the environmental impact, with 174 (58%) respondents citing this as a concern. Meanwhile, 74 (25%) respondents indicated that they had no concerns about SUCs, and 60 (20%) respondents indicated that they had no concerns about reusable cystoscopes (Figure 2).
 |
Figure 2 Level and type of concern, single use vs reusable. |
Willingness to Pay
The middle levels of the attributes were chosen as references. The differences in preference weights provided an estimate of the relative importance of that attribute over the range of levels. All values were statistically significant (Table 5).
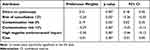 |
Table 5 Conditional Logit Model Results |
Going direct to a cystoscopy procedure from the initial consultation was the most important aspect, with a preference weight of 0.31. The WTP to undergo a cystoscopy right after the first consultation was 62 EUR (95% CI, 33; 90 EUR). A reduction in the negative environmental impact from high to neutral had a relative importance of 0.30. When the coefficients were negative, the reference point from the mid-level was then switched to the level being compared. Patients would pay approximately 59 EUR (95% CI, 25; 93 EUR) if the negative environmental impact would change from being high to neutral. The high risk of contamination had a preference weight of 0.29, and patients would be willing to pay 57 EUR (95% CI, 22; 91 EUR) to reduce the risk of contamination from 12% to 6% during a cystoscopy. A reduction in the risk of cancellation from 12% to 6% had a preference weight of 0.20, for which patients would be willing to pay 39 EUR (95% CI, 5; 71 EUR) (Figure 3).
 |
Figure 3 Overall willingness to pay by attribute level. Confidence intervals are set at 95%. |
Two subgroup analyses of WTP by gender and age, respectively, revealed the following: male patients (100 EUR) (95% CI, 40; 161 EUR) would be willing to pay 57 EUR more to have a direct cystoscopy compared to female patients (43 EUR) (95% CI, 11; 72 EUR). Similarly, male patients (86 EUR) (95% CI, −155; 16 EUR) would be willing to pay 48 EUR more to reduce the risk of high contamination from 12% to 6% compared to female patients (37 EUR) (95% CI, −77; −2 EUR). In contrast, female patients (60 EUR) (95% CI, −98; −22 EUR) would be willing to pay 8 EUR more to reduce the negative environmental impact from high to neutral compared to male patients (52 EUR) (95% CI, −116; 12 EUR) (Table 6).
 |
Table 6 WTP by Subgroup (EUR) |
Patients aged >50 years old (77 EUR) (95% CI, −128; −25 EUR) would pay a higher amount to reduce the negative environmental impact from high to neutral, with significant p values, compared to patients aged <50 years old (58 EUR) (95% CI, −100; 15 EUR). Nevertheless, those aged <50 years (71 EUR) (95% CI, 35; 107 EUR) would pay 33 EUR more to proceed directly to cystoscopy from the initial consultation compared to patients aged >50 years (38 EUR) (95% CI, −4; 80 EUR). Likewise, patients aged <50 years (60 EUR) (95% CI, −103; −18 EUR) would pay 29 EUR more compared to those aged >50 years (31 EUR) (95% CI, −85; 22 EUR) to reduce the risk of contamination from 12% to 6% (Table 6).
Discussion
To our knowledge, this is the first study to estimate cystoscopy patients’ WTP in reference to attributes related to the cystoscopy procedure. The main findings of this study were the dominant preference of patients for SUCs (265, 88%) and the varying WTP considering specific attributes, such as proceeding directly to cystoscopy and the reduction in the negative environmental impact, associated with a cystoscopy procedure. Existing studies have examined patients’ anxiety and pain levels while focused on the insertion of the cystoscope and stent removal rather than on their overall preferences, and even though SUCs have shown more versatility and efficiency when performing JJ stent removals as reflected in the less anxiety experienced by patients,10 research has not assessed the difference in pain or anxiety levels of single-use versus reusable cystoscopes.14–18 A recent study asked 20 patients to rate their level of satisfaction on a scale from 1 to 10 points regarding the use of an SUC (aScope™ 4 Cysto; Ambu, Ballerup, Denmark) compared to a reusable device (CYF-240; Olympus Corporation, Tokyo, Japan), and the obtained results included a significant difference in scores (9.65 vs 9.05 points respectively) and a p value of 0.0455. Furthermore 95% of the patients preferred to undergo the procedure with a SUC compared to 5% who did not have any preference.8 Interestingly, this study found similar results where most of the individuals (228, 89.76%) will prefer a SUC. Another study reported that anxiety levels tend to be higher in the pre-procedure state when the patient does not know what to expect.28 Moreover, the importance of providing written and understandable information to the patient, from a patient perspective, regarding the flexible cystoscopy procedure has been highlighted. Many experts involved in such studies claim the need to pay attention to handle and manage the pain of patients by either using better drugs for anesthesia or a different type of cystoscope, such as a flexible one. Patients’ experiences may contribute and allow inferences of patient preferences.
This study also uncovered the WTP in 4 main attributes related to cystoscopy procedures through a DCE method. First, the most important attribute was the capability to go direct to cystoscopy, with a WTP of 62 EUR. A study assessing 500 respondents, including 336 men, with a mean age of 66 years showed that 85% of 193 respondents who were undergoing cystoscopy for the first time preferred to progress directly to cystoscopy, avoiding the need for a pre-procedural consultation. This trend was also seen among patients who had a better understanding of the procedure to come.20 Second, there was a reduction in the high environmental impact to neutral with a WTP of 59 EUR. To our knowledge, there are no studies that have assessed the environmental impact of SUCs; nevertheless, an assessment of reusable flexible ureteroscopes and single-use flexible ureteroscopes measured the carbon footprint of these devices, analyzing manufacturing data, repairs, replacement instruments, and device disposal, ultimately revealing a comparable environmental impact.24 Further assessment of the environmental aspects of cystoscopes is recommended.
Third, there was a reduction in the risk of contamination from 12% to 6% with 57 EUR. SUCs have been shown to reduce hospital stay lengths10 while eliminating the risk of cross-contamination. This attribute becomes more relevant due to the greater concern for contamination exposure after COVID-19.
Lastly, the risk of cancellation from 12% to 6% with a WTP of 39 EUR. A previous study examining the introduction of SUCs at a hospital in UK have shown that SUCs can reduce the rate of cancellation.6 This study further showed that SUCs were associated with an increase in diagnostic capacity, fewer complications and reduced readmissions.6
Moreover, SUCs have been shown to be a more efficient option, offering several advantages like cost-efficiency and efficacy; portability; user friendliness;6,8,10 guaranteed sterility; reliable quality;11 suitability; and no risk of wear or the need for cleaning, maintenance, or repairs compared to traditional flexible cystoscopy. Consequently, SUCs have the capacity to accommodate the preferences of patients found in this study.
Limitations
The most common indication for receiving a cystoscopy procedure was a UTI1 (42, 47%), followed by a hyperactive bladder (84, 28%) and recurrent UTIs (77, 26%). Other causes (45, 15%) included BPH (Benign prostatic hyperplasia) and prostate cancer. Most of our patients were between 18–49 years of age. Our sample may not represent most bladder cancer patients, who are commonly aged 60–80 years, in Spain, so these results should be taken with caution when estimating patient preferences among cystoscopy patients aged >50 years. Study recruitment was voluntarily via the IQVIA database, and patient age and their ease with using the online platform could have influenced the resulting sample. To overcome this potential barrier, patient recruitment was also planned in hospitals using surveys distributed in print. However, due to COVID-19 restrictions during the study period, the handling of surveys in print was not allowed.
Conclusions
This study investigated the preference of patients through their WTP for the cystoscopy procedure in Spain. The study found a dominant preference for SUCs compared to reusable cystoscopes in nearly 265 (88%) patients. Thereafter, the WTP in 4 main attributes related to cystoscopy procedures was assessed through a DCE method, making this investigation a pioneering study of patients’ preferences. The most important attribute was the capability to proceed directly to a cystoscopy, with a WTP of 62 EUR; meanwhile, the reduction of the high environmental impact to neutral with a WTP of 59 EUR, the reduction in the risk of contamination from 12% to 6% with 57 EUR, and the reduction in the risk of cancellation from 12% to 6% with a WTP of 39 EUR were second through fourth in terms of importance, respectively. All values were statistically significant. Our results support the validity of analysis and further assessment of the influence an attribute of a product can have on the choice of the consumer or patient.
Disclosure
C. N. B. B. started her research as a non-remunerated master thesis project with Ambu A/S, Ballerup, Denmark for the program BA and Innovation in Healthcare, Ambu sponsored the collection of raw data through IQVIA. Months after the submission of the master thesis she became employed by Ambu A/S, Ballerup, Denmark. D. K. R. is currently employed by Ambu A/S, Ballerup, Denmark. The authors report no other conflicts of interest in this work.
References
1. Engelsgjerd JS, Deibert CM. Cystoscopy. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022.
2. Ellis G, Pridgeon S, Lamb BW, et al. Psychological distress in out-patients undergoing flexible cystoscopy for the investigation of bladder cancer. J Clin Urol. 2015;8(3):196–201. doi:10.1177/2051415814551821
3. Gao J, Tian DW, Zhou DS, Wu CL. Flexible cystoscopy can improve anxiety and subjective feelings of bladder cancer patients during follow-up. Videosurgery Other Miniinv Tech. 2021;16(2):397–402. doi:10.5114/WIITM.2020.100860
4. Bywall KS, Veldwijk J, Hansson MG, Kihlbom U. Patient perspectives on the value of patient preference information in regulatory decision making: a qualitative study in Swedish patients with rheumatoid arthritis. Patient. 2019;12(3):297–305. doi:10.1007/S40271-018-0344-2/TABLES/4
5. EUnetHTA. EUnetHTA JA2 WP8 Deliverable HTA Core model version 3.0 for the full assessment of diagnostic technologies, medical and surgical interventions, pharmaceuticals and screening technologies; 2016. Available from: www.htacoremodel.info/ViewHandbook.aspx.
6. Baston EL, Wellum S, Bredow Z, et al. Office-based ureteric stent removal is achievable, improves clinical flexibility and quality of care, whilst also keeping surgeons close to their patients. Cent European J Urol. 2018;71(2):196–201. doi:10.5173/CEJU.2018.1519
7. Phan YC, Cobley J, Mahmalji W. Cost analysis and service delivery on using isiris αTM to remove ureteric stents. J Endol Endourol. 2018;1(1):e3–e16. doi:10.22374/JELEU.V1I1.5
8. Wong A, Phan YC, Thursby H, Mahmalji W. The first UK experience with single-use disposable flexible cystoscopes: an in-depth cost analysis, service delivery and patient satisfaction rate with ambu® aScopeTM 4 Cysto. J Endolum Endourol. 2021;4(1):e29–e44. doi:10.22374/jeleu.v4i1.120
9. Su ZT, Huang MM, Matlaga BR, Hutfless S, Koo K. A micro-costing analysis of outpatient flexible cystoscopy: implications for adoption of single-use flexible cystoscopes. World J Urol. 2021;1–7. doi:10.1007/s00345-021-03724-3
10. Oderda M, Antolini J, Falcone M, Lacquaniti S, Fasolis G. Cost-effectiveness analysis of a single-use digital flexible cystoscope for double J removal. Urologia. 2020;87(1):29–34. doi:10.1177/0391560319859797
11. Whelan P, Kim C, Tabib C, Preminger GM, Lipkin ME. Evolution of single-use urologic endoscopy: benchtop and initial clinical assessment of a new single-use flexible cystoscope. J Endourol. 2022;36(1):13–21. PMID: 34235971. doi:10.1089/end.2021.0219
12. Scotland K, Wong VKF, Chan JYH, et al. Evaluation of a single-use flexible cystoscope: a multi-institutional international study. J Endourol. 2020;34(9):981–986. doi:10.1089/end.2020.0002
13. Talso M, Emiliani E, Baghdadi M, et al. The new grasper-integrated single use flexible cystoscope for double J stent removal: evaluation of image quality, flow and flexibility. World J Urol. 2017;35(8):1277–1283. doi:10.1007/S00345-016-1987-Z
14. Abdulmajed MI, Shergill IS. Flexible cystoscopy removal of ureteric stent: is it painful? Br J Med Surg Urol. 2011;4(5):223. doi:10.1016/J.BJMSU.2011.06.020
15. Tan WS, Teo CH, Chan D, et al. Exploring patients’ experience and perception of being diagnosed with bladder cancer: a mixed‐methods approach. BJU Int. 2020;125(5):669–678. doi:10.1111/BJU.15008
16. Loh-Doyle JC, Low RK, Monga M, Nguyen MM. Patient experiences and preferences with ureteral stent removal. J Endourol. 2015;29(1):35–40. doi:10.1089/END.2014.0402
17. Oliver R, Wells H, Traxer O, et al. Ureteric stents on extraction strings: a systematic review of literature. Urolithiasis. 2018;46(2):129–136. doi:10.1007/S00240-016-0898-1/TABLES/3
18. Guner E, Seker KG. Comparison of two different scoring systems in encrusted ureteral stent management: a single-center experience. Urol J. 2020;17(3):248–251. doi:10.22037/UJ.V0I0.5516
19. Kjaer T. A review of the discrete choice experiment - with emphasis on its application in health care — university of Southern Denmark. Health Econ Papers. 2005;1:1–139.
20. Assmus MA, McLarty R, Senthilselvan A, De SK. Direct to cystoscopy: a prospective quality assessment of patient preferences. Can J Urol. 2020;14(4):118–121. doi:10.5489/cuaj.6013
21. Rutala WA, Weber DJ. Sterilization, high-level disinfection, and environmental cleaning. Infect Dis Clin North Am. 2011;25(1):45–76. doi:10.1016/J.IDC.2010.11.009
22. Rutala W, Weber D. Guideline for disinfection and sterilization in healthcare facilities; 2008. Available from: https://stacks.cdc.gov/view/cdc/47378.
23. Saliou P, le Bars H, Fournier G, Baron R. Évaluation microbiologique de la désinfection des cystoscopes souples au CHRU de Brest de janvier 2007 à décembre 2014 [Microbiological evaluation of the disinfection of flexible cystoscopes at Brest CHRU from January 2007 to December 2014]. Prog Urol. 2016;26(2):103–107. doi:10.1016/J.PUROL.2015.10.012
24. Davis NF, McGrath S, Quinlan M, Jack G, Lawrentschuk N, Bolton DM. Carbon footprint in flexible ureteroscopy: a comparative study on the environmental impact of reusable and single-use ureteroscopes. J Endourol. 2018;32(3):214–217. doi:10.1089/end.2018.0001
25. Bridges JFP, Hauber AB, Marshall D, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR good research practices for conjoint analysis task force. Value Health. 2011;14(4):403–413. doi:10.1016/J.JVAL.2010.11.013
26. World medical association. Declaration of Helsinki, Ethical principles for scientific requirements and research protocols; 2013. Available from: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/.
27. Agencia Estatal Boletin Oficial del Estado. Legislación, Real Decreto 1090/2015, de 4 de diciembre [Legislation, Royal Decree 1090/2015, of 4 December]; 2016. Available from: https://www.boe.es/buscar/doc.php?id=BOE-A-2015-14082.
28. Wehner S, Saiz Y, Woodard H, Garcia D. Avoiding same-day cystoscopy cancellations by veterans: nurse-led education improved efficiency for cystoscopy in VA urology clinics. Urol Nurs. 2016;36(6):275–281. doi:10.7257/1053-816X.2016.36.6.275
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
