Back to Journals » Patient Preference and Adherence » Volume 9
What are the preferences of health care professionals in Germany regarding fully liquid, ready-to-use hexavalent pediatric vaccine versus hexavalent pediatric vaccine that needs reconstitution?
Authors Lloyd AJ, Nafees B, Ziani E, Nicolas L, Fordham B, Soubeyrand B, Bornhöft C
Received 23 April 2015
Accepted for publication 5 August 2015
Published 27 October 2015 Volume 2015:9 Pages 1517—1524
DOI https://doi.org/10.2147/PPA.S87229
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Andrew J Lloyd,1 Beenish Nafees,1 Eddy Ziani,2 Laurence Nicolas,2 Beth Alice Fordham,1 Benoit Soubeyrand,2 Christoph Bornhöft3
1Patient Reported Outcomes, ICON Plc, Oxford, UK; 2Medical Affairs, Sanofi Pasteur MSD, Lyon, France; 3Practice for Pediatric and Adolescent Medicine, Bensheim, Germany
Abstract: Diphtheria, tetanus and acellular pertussis (DTaP) based combined vaccines have led to significant reduction in incidence of several serious pediatric infectious diseases. A new, fully liquid combined hexavalent vaccine has been introduced and has been shown to reduce administration time. This fully liquid vaccine may also be simpler to administer and could reduce handling errors. The present study was designed to understand the value that health care providers (HCPs) place on aspects of injection devices for combined hexavalent vaccine programs in Germany. A discrete choice experiment (DCE) was designed to elicit the views of HCPs regarding hexavalent vaccines. The key attributes of injection devices were identified through a focused literature search and interviews with HCPs. Five key attributes, each with two or three levels were described which included: type of device, experience of this hexavalent vaccine on the German market, preparation time, probability of handling errors, and dosage errors. Physicians (n=150) and nurses (n=150) who administered hexavalent vaccines in Germany completed the survey. Choice data were analyzed using the conditional logit procedure. All attributes were significant and important independent influences on physicians’ and nurses’ choices. Reducing any “probability of dosage errors” was the most important attribute. Both physicians and nurses had a strong preference to reduce preparation time. All other things equal both groups also significantly preferred a fully liquid hexavalent vaccine. They also preferred vaccines that had been on the market for a few years compared to ones that had not (especially the physicians). Additional analyses explored participants’ preferences in more detail through interaction terms. The DCE choice data provide useful insights into how HCPs view each aspect of the vaccination device. Overall, the HCPs preferred fully liquid vaccines. The survey also highlighted the importance of handling and dosage errors, reducing preparation time, and also experience of the HCPs with the use of a vaccine. The survey work included physicians and nurses and explored their views separately.
Keywords: hexavalent vaccines, fully liquid vaccines, preferences, handling errors, dosage errors
Introduction
Introduction of combined hexavalent vaccines for immunization of infants and toddlers has led to high vaccine coverage and a significant reduction in incidence of pediatric infectious diseases worldwide, including diphtheria, tetanus, pertussis, hepatitis B, poliomyelitis, and invasive diseases caused by Haemophilus influenzae type b (Hib).1 The delivery of vaccination programs is usually undertaken through primary care or through well-baby clinics. In Germany, vaccines are given by both physicians and nurses, but in some countries vaccines are given solely by nurses. Physicians and nurses are responsible for administering high volumes of vaccinations, so any innovative research that can provide insight into the views of these health care providers (HCPs) regarding vaccinations may help to support a more efficient process.
Vaccine preparation may require reconstitution, whereby the Hib component for an established hexavalent vaccine (Infanrix hexa: GlaxoSmithKline Biologicals, Middlesex, UK) has to be mixed with five other components prior to administration. In 2013, a new, fully liquid hexavalent vaccine (Hexyon: Sanofi Pasteur MSD, Lyon, France) was licensed in Europe. Several studies report that fully liquid vaccines can increase time efficiency.2–5
Other factors such as mishandlings and the number of steps involved with vaccine preparation may also be important to HCPs. Fully liquid vaccines may reduce vaccination wastage rates, but may have bulkier packaging which is difficult to store.2 Fully liquid vaccines have fewer preparation steps than non-fully-liquid based vaccines. The choice of fully liquid or non-fully-liquid vaccines may also simply be determined by the way clinics are organized and structured. The choice between different vaccines is dependent on a range of factors, such as time taken per vaccination, mishandlings, and possibly packaging. The importance of each of these factors in driving decisions is not clear. One method to understand the value of tangible and slightly less tangible features of a vaccine or vaccination program is through the use of stated preference methods such as discrete choice experiment (DCE). DCE methods can be used to understand the strength of preference or value that HCPs place on design features in vaccination devices. The validity and appropriateness of standardized methods for eliciting preferences for a vaccine or treatment in health care research are quite well understood.6,7 These methods provide information regarding the significance of different vaccine attributes for HCPs’ decision making.
The present study was designed to reveal HCPs’ preferences regarding injection devices for hexavalent vaccine programs in Germany. The survey explores the importance of different features (or attributes) of fully liquid and non-fully-liquid vaccines.
Methods
Literature review
A focused literature review was undertaken to identify the key attributes of interest to include in the DCE survey. The review examined research into vaccine delivery and vaccination devices. A search strategy was implemented across the EMBASE and MEDLINE databases to identify research on user preferences for vaccine devices.
Of the 99 titles which were identified from the search strategy, 10 were retrieved as abstracts and nine were directly relevant to the study objective.2–4,8–13 Only six studies provided any useful information. The literature review identified four broad themes. These themes related to time saving, vaccine safety (eg, needlesticks), vaccine accuracy in terms of dosage, and wastage. The literature review was limited however, and so, qualitative research with HCPs was undertaken to better understand the issues related to hexavalent vaccines.
HCP interviews
Telephone interviews were conducted with HCPs to further explore the findings from the literature review and to identify possible study attributes. A market research patient panel identified and recruited pediatricians (n=3) and nurses (n=2) based in Germany, who were currently responsible for preparing and/or administering at least 15 pediatric vaccinations per month. Interviews were conducted by an experienced German interviewer. The objective of the interviews was to identify the attributes of vaccination devices which may be important for HCPs. Participants were asked to describe each attribute and their experience while preparing and administering hexavalent vaccines for children.
The findings from the interviews are described here briefly. In terms of preparation time, participants explained that non-fully-liquid vaccines would take 1–2 minutes longer to prepare than fully liquid vaccines. When discussing the fully liquid vaccine devices, the participants considered that they had several possible advantages. These included being faster to prepare, more hygienic, and have lower chance of mishandlings and less risk of needlestick injuries. Fully liquid vaccines may also prevent any chance of dosing error by either failure to properly reconstitute the vaccine or by accidentally leaving some of the vaccine in the vial.
The physicians agreed that mishandlings were a very serious issue and that they had protocols in place to prevent this happening. When asked to describe their ideal device, all physicians agreed that it would be a ready-to-use (prefilled) device with a sharp needle or the option to change the needle and an easy-to-use plunger device.
Survey development
The findings from the qualitative interviews and the literature review were used to develop a preliminary list of attributes that was discussed and went through two rounds of review. Each attribute was described in terms of three distinct levels considered to reflect a relevant and realistic range for that attribute by the study team (Table 1).
  | Table 1 Attribute list with associated descriptions and the levels that were used in the survey |
The final five attributes and their levels were combined into hypothetical choices (called choice sets) which included each attribute with a distinct level. The combination of attributes and levels was based on an orthogonal fractional factorial design which was folded over to produce the alternative choice sets. The survey included a participant information sheet/informed consent form, an introductory screen, sociodemographic form, questions regarding HCP’s current vaccination experience, and the DCE survey.
It was translated into German and sent to four German HCPs (two pediatricians and two nurses) who were asked to complete the survey (as a pilot phase) before a cognitive debriefing telephone interview. These four participants were asked to comment on the clarity of the instructions, appropriateness of choices/questions, the face validity of the choices, overall length of the survey, and language used. From these interviews, seven linguistic changes were recommended, for example, to replace the word “Kleinkinder” (infants) with “Säüglinge und Kleinkinder” (toddlers and infants) to cover the relevant age group. These changes were implemented and translations checked before finalizing the survey. The final survey included a logical consistency check whereby one choice question was reversed and repeated.
Study sample
HCPs, either pediatricians or nurses – working in Germany – who administer (or prepare) a minimum of 15 hexavalent vaccinations per month to children and who were not in paid employment with the pharmaceutical industry were recruited for the survey. Participants were recruited across medical practices in Germany using a convenience sampling method by a specialist recruitment company (May–June 2014).
Data collection
Participants were invited to participate through email, and if they chose to follow the link, they were then directed to the informed consent form. Once signed, participants entered the screening section of the survey, and if they were eligible, they began the survey. Upon completion of the survey, participants were reimbursed a small recommended fee.
Statistical analysis
Sociodemographic and current vaccine usage data were analyzed as means, standard deviations, and frequencies or percentages. Data from the DCE survey were analyzed using a conditional logit model. This explored the impact of each attribute (independent variable) on the participants’ choices (dependent variable). Analyses were separated by profession (physician and nurse). The conditional logit model evaluated choice responses after conditioning them on the attributes of the other vaccine alternatives available within the choice set. Hence, if, for example, “Hexavalent injection device A” was preferred in the choice set number 1, this preference was conditional on the attributes of “Hexavalent injection device B.” The coefficients obtained from the logit model provided an estimate of the (log) odds ratios (ORs) of preference for attributes. In addition, interactions were explored to see whether there were any profession-specific differences in the preferences of HCPs. All analyses were conducted in SAS v.9.2 (SAS Institute Inc., Cary, NC, USA). Subgroup analyses explored how preferences varied by professions (physicians vs nurses), current role (administer only vs prepare and administer/prepare only), and HCP vaccine preference (non-fully-liquid vaccine vs fully liquid vaccine).
Results
Participant characteristics
A total of 300 participants (n=150 physicians, n=150 nurses) completed the online survey (Table 2). All participants completed the consistency check in the choice section correctly and were thus included in the analyses.
  | Table 2 Sociodemographic and current clinical practice profile of the sample by profession |
Table 2 presents the demographic data and clinical practice profile of all participants. The majority of physicians were male (69%) with a median age range from 51 to 54 years. The majority of nurses were female (63%) with a median age range of 35–40 years. Among the physicians, 69% only administered the vaccine, whereas the nurses prepared and sometimes administered the vaccines. All participants (nurses and physicians) were asked to consider the hexavalent vaccine they used most frequently and to describe this vaccine in terms of the attributes used in the DCE. For example, they identified if the vaccine was in a prefilled syringe (PFS) or not, what they perceived the risk of dosing errors to be, and how long preparation took. This question identified that the majority of the physicians currently use a vaccine which requires reconstitution (67%), whereas more nurses reported using a PFS (77%). Over half of the participants (59%) felt that the number of years that a hexavalent injection device had been available was not important and that it did not play a role in their choice of device. Participants reported that it took about 1 minute to prepare their current hexavalent vaccine. There were a variety of responses regarding mishandlings and dosage errors.
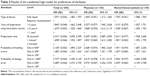
Participant preference findings
Physicians
All attributes were significant predictors of choice, which means that all attributes were an important influence on physicians’ choices (Table 3). The attribute “probability of dosage errors” was the most important attribute as indicated by the high ORs. Physicians were almost four times more likely to prefer a vaccine that had an associated dosage error rate of 1:1,000 compared with one that had an error rate of 1:100 (OR =3.62, 95% CI =3.10–4.22). “Preparation time” was also an important attribute, with participants 2.5 times as likely to prefer a vaccine that took 30 seconds to prepare compared to the one that took 2 minutes (OR =2.45, 95% CI =2.089–2.870). Participants preferred vaccines that would have been available on the market for more than 3 years (OR =2.26, 95% CI =1.94–2.63). Physicians also preferred a fully liquid vaccine more than a non-fully-liquid vaccine (OR =1.45, 95% CI =1.312, 1.602).
Nurses
The data from nurses were similar to those from the physicians. The nurses also placed high value on “probability of dosage errors” and preferred a vaccine with the least probability of errors (OR =3.95, 95% CI =3.40–4.60). “Preparation time” and “probability of mishandlings” were also important attributes of choice whereby participants preferred vaccines that took least time to prepare (OR =2.24, 95% CI =1.93–2.61) and included least likelihood for mishandlings (OR =1.95, 95% CI =1.69–2.26). Nurses preferred vaccines which they had some experience of using (as opposed to a vaccine and device that had not been on the market previously), but this preference was not as strong as for the physicians. Nurses placed significantly higher value on a fully liquid vaccine than the physicians (OR =1.76, 95% CI =1.59–1.94), confirmed in independent analyses (P<0.001).
Further interaction analyses explored whether there were significant differences in strength of preference by profession. Compared to nurses, the physicians placed significantly more value on “years of experience of using hexavalent vaccine”; and on injection devices which took less time to prepare (P<0.01).
Analyses were conducted to compare the preferences of HCPs who prepared vaccines (including preparing and administering) compared to those who only administered the vaccine. Participants who prepared the vaccine had a significantly greater preference for a fully liquid vaccine (P<0.01). Those HCPs who only administered the vaccine placed significantly higher value on avoiding “dosage errors” (P<0.01).
Finally, interaction analyses were also conducted to determine whether preferences varied by the vaccine that the HCPs were using currently, fully liquid or non-fully-liquid vaccine. Participants who were currently using fully liquid vaccine placed significantly higher value on a fully liquid vaccine than participants who were using non-fully-liquid vaccine (P<0.02). Participants who were using fully liquid vaccine placed less value on the years of experience they had with the vaccine (P<0.01). The non-fully-liquid vaccine group had a significantly stronger preference for injection devices with shorter preparation time (P<0.01) and on avoiding dosage errors than the fully liquid vaccine group (P<0.01).
Discussion
This study reports a survey of HCPs regarding the importance of different features of vaccination devices for hexavalent pediatric vaccines. The study used a DCE survey which is a well-recognized stated preference method. Vaccination programs are perhaps unique within medicine in terms of the number of patients that a HCP will treat. Some of the HCPs in this study reported that they administered as many as 250 doses of vaccine a month. Because of this high number of patients, there is potential for innovations in the design of devices to improve the efficiency of the service. This survey attempted to explore this aspect with HCPs. The survey specifically avoided aspects related to the safety or immunogenicity of vaccines because the immunogenicity and safety of the two hexavalent vaccines are considered to be similar.14 Instead the survey focused on issues such as the need for reconstitution, years of experience in using a vaccine, preparation time, and handling or dosage errors.
The study captured the views of physicians and nurses separately. At the outset of the study, we understood that in Germany generally vaccines were given to children by both physicians and nurses. However, the present data suggest that practice is much more variable. Over half of our nurse sample indicated that they prepare and administer the vaccine. Interestingly, 30% of the physicians prepare their vaccine as well as administer it.
The in-depth interviews with physicians and nurses during the survey development phase provided different information to the main DCE survey. In the qualitative interviews, the physicians describe mishandlings such as needlestick injuries as a rarity, which could lead to disciplinary action. In contrast, the survey data suggested that mishandlings occurred more frequently. Almost 15% of nurses (and 10% of physicians) indicated that they thought that mishandlings occurred at least once in every 200 patients. Dosing errors such as a failure to administer the entire vaccine or a failure to properly reconstitute were also reported to occur. A Time and Motion study performed in Belgium5 comparing preparation time with a fully liquid hexavalent vaccine (Hexyon, Sanofi Pasteur MSD) and a non-fully-liquid hexavalent vaccine (Infanrix hexa, GlaxoSmithKline Biologicals) has shown that mishandlings occurred five times more with the hexavalent vaccine that needs reconstitution (47 mishandlings with the non-fully-liquid hexavalent vaccine and 10 with the fully liquid hexavalent vaccine out of 192 preparations).
The DCE choice data provide useful insights into how HCPs view each aspect of the vaccination device. Overall, the HCPs preferred fully liquid vaccines. The samples were approximately 50% more likely to choose a vaccine if it was fully liquid. However, the nurses revealed a larger preference for fully liquid vaccines compared to the physicians. The use of fully liquid vaccines perhaps has more impact on the workload of nurses – particularly those who are focused on the preparation of vaccines only. This is consistent with previous studies which report that fully liquid vaccines that did not require reconstitution, saved time, and were more efficient. Kumar et al2 reviewed a survey of 200 National Health Service nurses in the UK who administered vaccinations to children. The authors reported that administration of the fully liquid vaccine saved 4 minutes and 47 seconds across three doses when compared to a vaccine which required reconstitution (non-fully-liquid vaccine). Wiedenmayer et al3 observed 312 vaccinations in India and found that the fully liquid vaccine saved 46 seconds on average, when compared to the non-fully-liquid vaccine. Lafuma and Mara4 reported that injectable fully liquid products saved 52 seconds on average, decreasing the time spent on injection preparation by 35%. More recently, De Coster et al5 also reported in a population of 96 physicians and nurses that time needed to prepare a fully liquid hexavalent vaccine was about 50% lower than time needed to prepare a non-fully-liquid hexavalent vaccine. When considered in the context of mass immunization programs, these time savings can become quite significant. In the same study, these time savings were estimated to 664 days per year.5
When we look at the data for HCPs overall, they indicate that they are almost twice as likely to choose a vaccine which has been used for over 3 years compared to one that has been in use for less than a year. However, this effect differed between the two groups. Physicians placed significantly more value on this attribute than nurses did and this aspect of preference has not been explored previously in research and may be an important consideration for decision making. Both groups significantly preferred being able to reduce preparation time to just 30 seconds from 2 minutes. The physicians placed more value on this than the nurses, which may reflect their workload or their perceived value of their time. In previous work, HCPs have highlighted the importance of time saving and how much it can affect resource management.3
The avoidance of handling errors and dosing errors was important to participants. Overall, the HCPs were twice as likely to choose an option where the probability of handling errors slips to only 1:500 vaccinations compared to 1:100. Handling errors included needlesticks, contamination, and missing vials. Physicians placed significantly more value than nurses on reducing this risk to 1:500. Interestingly, both physicians and nurses placed more value on avoiding dosage errors than handling errors. HCPs were over three times as likely to prefer a vaccine with the lowest risk of dosage errors. The physicians placed more importance or value on reducing this risk (specifically at the 1:500 risk). Sharp and Whyte10 report that PFSs provided more accurate dosage than reconstitution devices, which may also explain the preference for PFS in the current study.
In addition to the primary analysis and the split by type of HCP, a series of additional analyses was also undertaken to determine the influence of other variables on participants’ preferences by exploring interaction terms on the analysis. Interesting differences did emerge here. For example, those HCPs engaged in the preparation of vaccines had a stronger preference for the fully liquid vaccine compared with HCPs who only administered vaccines. And those people who administered vaccines placed more value on vaccines which had been in use for a number of years. HCPs who administer vaccines placed more value on avoiding dosing errors compared with those involved in any preparation.
Further analyses explored the influence of the type of vaccine that the HCP had most experience with – either fully liquid or non-fully-liquid vaccine. Experience with a specific vaccine clearly had a large effect on participants’ preferences. For example, fully liquid hexavalent vaccine users had a strong preference for fully liquid syringes, and were significantly less concerned about the amount of time that a vaccine had been available for use. Fully liquid hexavalent vaccine users valued rapid preparation time more and were significantly less concerned about dosage errors.
There are some limitations to this work which should be considered. The survey was restricted to recruiting HCPs in Germany only. We believe that the results are representative of practice in Germany, but they may not generalize well to other countries. There are some important differences regarding how vaccination programs are organized in different countries and this could have quite a large effect on the results. In the UK, for example, pediatric vaccination programs are undertaken by nurses alone. It would be interesting therefore to extend this work to other countries to see how these preference weights vary. The study was undertaken relatively soon after fully liquid hexavalent vaccine was introduced into the German market, and the distribution of fully liquid hexavalent vaccine and non-fully-liquid hexavalent vaccine users in the survey may not represent the current distribution. This is a source of potential bias. Over time as physicians gain greater experience of the use of the fully liquid hexavalent vaccines, we can speculate that they may value such features (convenience, speed etc) more highly.
This study has provided extensive detail regarding the views of different HCPs about hexavalent vaccinations for children. The survey focused on issues related more to the process of giving vaccinations, such as the use of fully liquid hexavalent vaccines, the importance of errors, reducing preparation time, and also the views of HCPs regarding the value that arises or accrues through the use of vaccines over several years. The findings indicated that, overall, all HCPs preferred fully liquid vaccines but there were some differences between nurses and physicians. This study identifies the aspects of hexavalent vaccination devices that HCPs in Germany consider important.
Disclosure
This work was conducted by ICON on behalf of Sanofi Pasteur MSD. EZ, LN, and BS are full-time employees of Sanofi Pasteur MSD. BN and AL are freelance consultants of ICON Plc. BF was a full-time employee of ICON Plc at the time of the study. The authors report no other conflicts of interest in this work.
References
World Health Organisation. Global status of immunization safety: report based on the WHO/UNICEF joint reporting form, 2004 update. Wkly Epidemiol Rec. 2005;80(42):361–367. | ||
Kumar G, Padhiar A, Carroll S, Woods B, Shread K. Estimating the cost impact of switching from a vial to a pre-filled syringe mode of administration for the DTaP-IPV-Hib ‘5-in-1’ vaccine in infants. Value Health.2013;16:A345. | ||
Wiedenmayer KA, Weiss S, Chattopadhyay C, et al. Simplifying paediatric immunization with a fully liquid DTP-HepB-Hib combination vaccine: evidence from a comparative time-motion study in India. Vaccine. 2009;27:655–659. | ||
Lafuma A, Mara Y. Comparison of the time to prepare contrast media injection in CT scan exam with prefilled syringes and bottles in 7 European countries. Value Health. 2009;12:A254. | ||
De Coster I, Fournie X, Ziani E, Soubeyrand B, Van Damme P. Assessment of preparation time with fully liquid versus reconstituted paediatric hexavalent vaccines: a time and motion study. Arch Dis Child. 2014;99:A80–A81. | ||
Lancsar E, Louviere J. Conducting discrete choice experiments to inform health care decision making: a user’s guide. Pharmacoeconomics. 2008;26:661–677. | ||
Bridges JF, Hauber AB, Marshall D, et al. Conjoint analysis applications in health – a checklist: a report of the ISPOR good research practices for conjoint analysis task force. Value Health. 2011;14:403–413. | ||
Chan E, Maa Y-F, Overcashier D, Hsu C. Investigating liquid leak from pre-filled syringes upon needle shield removal: effect of air bubble pressure. PDA J Pharma Sci Technol. 2011;65:363–371. | ||
DiLuzio W, Nguyen P. Considerations of critical formulation and syringe parameters during pre-filled syringe product development. Am Pharm Rev. 2011;14:20–28. | ||
Sharp B, Whyte P. New directions in the development of pre-filled syringes. Innovat Pharmaceut Technol. 2010;32:64–68. | ||
DeGrazio FL. Risk mitigation strategies for pre-filled syringe systems. Innovat Pharmaceut Tech. 2010;34:22–25. | ||
Hwang R, Noolandi P, Amgen DB. From vial to autoinjector. Am Pharma Rev. 2007;10:2. | ||
Basurto I, Traverso ML. Pharmaco-economic assessment of morphine pre-filled syringe preparation in an intra-venous mixture unit. Farmac Hosp. 2001;25:164–168. | ||
McCormack PL. DTaP-IPV-Hep B-Hib vaccine (Hexaxim®): a review of its use in primary and booster vaccination. Paediatr Drugs. 2013;15(1):59–70. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.