Back to Journals » International Medical Case Reports Journal » Volume 16
Well-Circumscribed Intramuscular Lipoma of Superior Rectus Muscle
Authors Tangtammaruk P , Uiprasertkul M, Lumyongsatien M
Received 15 November 2022
Accepted for publication 12 January 2023
Published 27 March 2023 Volume 2023:16 Pages 215—219
DOI https://doi.org/10.2147/IMCRJ.S396382
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Phantaraporn Tangtammaruk,1 Mongkol Uiprasertkul,2 Mingkwan Lumyongsatien1
1Department of Ophthalmology, Mettapracharak Hospital, Nakhon Pathom, Thailand; 2Department of Pathology, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Mingkwan Lumyongsatien, Department of Ophthalmology, Mettapracharak Hospital, Nakhon Pathom, Thailand, Tel +66814958985, Fax +6634388744, Email [email protected]
Abstract: Extraocular muscle lipoma is a rare benign mesenchymal tumor of the orbit. We report a case of a 37-year-old woman who presented with chronic progressive proptosis and inferior globe displacement of left eye. External eye examination revealed a yellowish mass at the superior bulbar conjunctiva. Magnetic resonance imaging showed a well-circumscribed mass confined in the superior rectus muscle belly and tendon with a fat signal. Debulking surgery was performed using the transconjunctival and vertical lid split approach. A pathological study demonstrated matured adipose tissue cells encapsulated by a thin layer of fibrous tissue, in addition to the chronic non-specific inflammation of the tenon capsule tissue sample. Histopathological findings of the mass were consistent with a well-circumscribed intramuscular lipoma. The symptoms of the patient were significantly improved 3 months after surgical and short-course systemic steroid treatments. However, long-term surveillance is needed.
Keywords: intramuscular lipoma, soft tissue tumor, orbital tumor, extraocular muscle, well-circumscribed lipoma
Introduction
Lipomas are composed of mature adipose tissue encapsulated by a thin fibrous capsule. They typically originate from subcutaneous locations, usually in the upper and lower extremities, and rarely occur in the orbit.1,2 Intramuscular lipomas may be classified as infiltrative, well-defined, and mixed.3 Extraocular muscle lipoma is a rare benign tumor of the orbit with an incidence of 0.6%.4 To our knowledge, only four cases of infiltrative extraocular muscle lipoma have been reported in the literature, and they have involved the superior rectus,5,6 medial rectus,7 and superior oblique muscles.8 Histopathologic examination of previous cases showed skeletal muscle fibers incorporated within mature adipose tissue and fibrous connective tissue infiltrating striated muscle fibers.5–8
Case Report
A 37-year-old Thai woman presented with a 1-year history of painless proptosis of the left eye and complaints of diplopia during up gaze. She denied any previous history of trauma, underlying disease, or genetic disease in the family. Physical examination showed mild swelling of the left eyelid and a yellowish subconjunctival mass in the superior bulbar region, which had a soft consistency, was non-reducible, and had no apparent posterior limit (Figures 1 and 2). The best-corrected visual acuity (BCVA) was 20/20 bilaterally. The intraocular pressures were 14 mmHg in the right eye and 15 mmHg in the left eye. Extraocular movements were full for the right eye and limited in elevation for the left eye. The globe was displaced inferiorly by 5 mm (Figure 1), and proptosis of 5 mm was observed in the left eye. Hertel exophthalmometry of 10 right eye and 15 left eye with a base of 107 mm. Magnetic resonance imaging of the brain and orbits demonstrated a soft tissue mass with dimensions of 1.1×1.6 x 1.7 cm involving the superior rectus muscle belly and tendon (Figures 3 and 4). The lesion showed hyperintensity on T1- and T2-weighted images. The mass was saturated on fat-saturated sequences and suppressible on sequences with fat suppression. It was responsible for the left eye proptosis and inferior globe displacement.
 |
Figure 1 Inferior globe displacement, proptosis and eyelid swelling in the left eye. |
 |
Figure 2 A yellowish subconjunctival mass is visible in the superior bulbar area of the globe. |
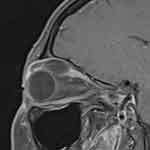 |
Figure 3 T1-weighted MRI sagittal view with fat suppression demonstrates well circumscribed mass, which decreases on fat suppression, in the superior rectus belly and tendon. |
 |
Figure 4 T1-weighted MRI coronal view demonstrates well circumscribed mass in the left superior rectus muscle with fat intensity in the left orbit. |
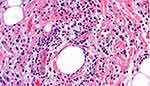
The superior bulbar mass gradually enlarged and prolapsed in the palpebral fissure over 4 months (Figure 5). A debulking procedure via a transconjunctival and vertical lid split was performed. An ovoid well-circumscribed yellowish mass was found at the superior rectus muscle in the sub-tenon and intraorbital spaces. A pathological study revealed mature adipose tissue, with minimal connective tissue stroma, enclosed in a thin fibrous capsule (Figure 6). The tenon capsule showed multiple foci of small lymphoid cells and plasma cell aggregates (Figure 7). The immunostaining results for CD3, CD5, CD10, CD20, CD23, cyclin D1, BCL2, kappa, lambda, immunoglobulin (Ig) G (IgG), IgG4, IgA, and IgM were consistent with chronic non-specific inflammation. Systemic steroid treatment (prednisolone 1 mg/kg/day) was initiated and maintained for 1 month. The BCVA last follow-up was 20/20. The proptosis and diplopia improved 3 months after treatment.
 |
Figure 5 The picture shows the mass progressive growth and prolapse into the palpebral fissure. |
 |
Figure 6 Hematoxylin and eosin (H&E) (1×) Whole mount section of the orbital mass demonstrates an encapsulated adipose tissue mass, with foci of lymphoid aggregates. |
Discussion
The diagnosis of lipoma is based on clinical, imaging, and standard histopathologic findings. The intramuscular lipoma has distinctive histopathological features that can be categorized as infiltrative, well-circumscribed, or mixed. Histological findings for the infiltrative type include an abundance of mature adipose tissue without a capsule admixed with skeletal muscle and fibroblastic elements.4,5 The well-circumscribed type is composed of a discrete mass of uniform mature adipocytes and encapsulated by a delicate fibrous stroma. No muscle fibers or entrapped muscles are located within the tumor.
Magnetic resonance imaging shows that the signal intensity of lipomas is similar to that of fat, and it decreases with fat suppression and is not enhanced by gadolinium. Benign lipomas may contain streaky structures that correspond to areolar fibrous tissues.9 In our patient the lipoma was a homogenous mass with a fat signal involving the superior rectus muscle belly and tendon.
In addition, histopathological findings of the mass were consistent with a well-circumscribed intramuscular lipoma. There were multifocal aggregates of lymphoid cells and plasma cells, with mild fibrotic tissue of the adjacent tenon capsule. Hence, immunohistochemical staining was performed to characterize the lymphoid aggregates. The result showed chronic non-specific inflammation with fibrosis in the tenon capsule that correlates with the exposed lesion in the palpebral fissure. To the best of our knowledge, this is the first report of a well-circumscribed intramuscular lipoma of the extraocular muscle.
The treatment of choice for lipoma is complete surgical excision; local recurrence may occur if the excision is incomplete. However, intramuscular lipomas tend to infiltrate surrounding tissues, and complete excision without injury to adjacent tissues may not be possible. For extraocular muscle lipoma, total resection may lead to significant functional morbidity. Thus, debulking surgery was suitable to improve symptoms without compromising function. For the residual tumor and chronic non-specific inflammation with fibrosis in the tenon capsule, the oral prednisolone 1 mg/kg/day was initiated and maintained for 1 month. Because lipomas have a high recurrence rate, long-term surveillance is required.
In conclusion, this case was the first well-circumscribed intramuscular lipomas presenting with diplopia, progressive proptosis and upgaze impairment. Diagnosis was made by clinical, imaging and histopathological to comfirm nature of disease. Treatment of choice is surgical excision. However, debulking may be considered to avoid functional morbidity, and long-term surveillance is needed.
Ethical and Consent Statements
Since the data were anonymous and no threat to patient’s rights, the Ethics Committee of Mettapracharak Hospital exempts the need for ethical approval. Written informed consent was provided by the patients to have the case details and any accompanying images published. The patient agreed to the publication of the case and images.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: the 2002 Montgomery Lecture, part 1. Ophthalmology. 2004;111:997–1008. doi:10.1016/j.ophtha.2003.01.002
2. Günalp I, Gündüz K. Mesenchymal orbital tumors. Orbit. 2006;15:225–228. doi:10.3109/01676839609150242
3. McTighe S, Chernev I. Intramuscular lipoma: a review of the literature. Orthop Rev. 2014;6(4):5618. doi:10.4081/or.2014.5618
4. Shah NB, Chang WY, White VA, et al. Orbital lipoma: 2 cases and review of literature. Ophthal Plast Reconstr Surg. 2007;23:202–205. doi:10.1097/IOP.0b013e318050ca52
5. Hristodulopulos V, Medel R. Intramuscular lipoma of the superior rectus muscle. Ophthal Plast Reconstr Surg. 2016;32:e52–e55. doi:10.1097/IOP.0000000000000230
6. Vahdani K, Mcveigh K, Ford R. Superior rectus intramuscular lipoma. Ophthal Plast Reconstr Surg. 2017;33:396–397. doi:10.1097/IOP.0000000000000967
7. Shiraki K, Kamo M, Sai T, et al. Rare site for an intramuscular lipoma. Lancet. 2002;359:2077. doi:10.1016/S0140-6736(02)08906-7
8. Dutton JJ, Wright JD
9. Nishida J, Morita T, Ogose A, et al. Imaging characteristics of deep-seated lipomatous tumors: intramuscular lipoma, intermuscular lipoma, and lipoma-like liposarcoma. J Orthop Sci. 2007;12:533–541. doi:10.1007/s00776-007-1177-3
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.