Back to Journals » Medical Devices: Evidence and Research » Volume 10
Wearable cardioverter defibrillators for the prevention of sudden cardiac arrest: a health technology assessment and patient focus group study
Authors Ettinger S , Stanak M , Szymański P , Wild C, Tandara Haček R , Erčević D, Grenković R , Huić M
Received 15 June 2017
Accepted for publication 29 August 2017
Published 14 November 2017 Volume 2017:10 Pages 257—271
DOI https://doi.org/10.2147/MDER.S144048
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Sabine Ettinger,1 Michal Stanak,1 Piotr Szymański,2 Claudia Wild,1 Romana Tandara Haček,3 Darija Erčević,3 Renata Grenković,3 Mirjana Huić3
1Ludwig Boltzmann Institute for Health Technology Assessment, Vienna, Austria; 2Institute of Cardiology, Warsaw, Poland; 3Department for Development, Research and Health Technology Assessment, Agency for Quality and Accreditation in Health Care and Social Welfare, Zagreb, Croatia
Aim: To summarize the evidence on clinical effectiveness and safety of wearable cardioverter defibrillator (WCD) therapy for primary and secondary prevention of sudden cardiac arrest in patients at risk.
Methods: We performed a systematic literature search in databases including MEDLINE via OVID, Embase, the Cochrane Library, and CRD (DARE, NHS-EED, HTA). The evidence obtained was summarized according to GRADE methodology. A health technology assessment (HTA) was conducted using the HTA Core Model® for rapid relative effectiveness assessment. Primary outcomes for the clinical effectiveness domain were all-cause and disease-specific mortality. Outcomes for the safety domain were adverse events (AEs) and serious adverse events (SAEs). A focus group with cardiac disease patients was conducted to evaluate ethical, organizational, patient, social, and legal aspects of the WCD use.
Results: No randomized- or non-randomized controlled trials were identified. Non-comparative studies (n=5) reported AEs including skin rash/itching (6%), false alarms (14%), and palpitations/light-headedness/fainting (9%) and discontinuation due to comfort/lifestyle issues (16–22%), and SAEs including inappropriate shocks (0–2%), unsuccessful shocks (0–0.7%), and death (0–0.3%). The focus group results reported that experiencing a sense of security is crucial to patients and that the WCD is not considered an option for weeks or even months due to expected restrictions in living a “normal” life.
Conclusion: The WCD appears to be relatively safe for short-to-medium term, but the quality of existing evidence is very low. AEs and SAEs need to be more appropriately reported in order to further evaluate the safety of the device. High-quality comparative evidence and well-described disease groups are required to assess the effectiveness of the WCD and to determine which patient groups may benefit most from the intervention.
Keywords: sudden cardiac arrest, ventricular tachycardia, ventricular fibrillation, cardioverter defibrillator, external, wearable, patient involvement
Three letters to the Editor have been received and published for this article
Introduction
Coronary artery disease patients most commonly die of sudden cardiac arrest (SCA). SCA causes approximately 25% of 17 million deaths of cardiovascular disease patients worldwide every year.1 About 350,000 SCAs occur out of hospital each year2 in Europe. In the US, estimations suggest that 326,000 persons are affected by SCAs outside of the hospital on an annual basis, whereby a large part of these SCAs happen in the domestic environment with 50% of the cases unnoticed by others.3 Predominantly, ventricular tachycardia (VT) and ventricular fibrillation (VF) constitute the main pathophysiological mechanisms of SCA.1,4 Untreated SCA results in sudden cardiac death (SCD).
Implantable cardioverter defibrillators (ICDs) which can automatically intervene and terminate life-threatening arrhythmias are the current standard for prevention of SCD. Pharmacological treatment and/or catheter ablation were documented to decrease the risk of SCD in some subsets of cases. Immediate cardiopulmonary resuscitation and the application of automated external defibrillators have shown improved survival from SCA.1 The wearable cardioverter defibrillator (WCD) represents a new addition to the spectrum of strategies for the prevention of SCD.
Limited information on effectiveness and safety of the WCD in the form of health technology assessment (HTA) reports or recently published reviews is available.5–7 The American Heart Association (AHA) published a science advisory on the WCD in 2016, which includes recommendations on possible use of the WCD with the intention to offer clinicians some directions for discussing therapy options with patients. The authors highlighted that discussion of patient preferences is of utmost importance.7 Furthermore, no information on possible ethical, organizational, patient, social, and legal aspects of the WCD use is available, which is also pointed out in a recent paper by Reek et al.8 Recently, the European Network for Health Technology Assessment (EUnetHTA) introduced the Core Model® for rapid relative effectiveness assessment (REA) – a methodological framework for the assessment of clinical effectiveness and safety of pharmaceuticals, diagnostic technologies, medical and surgical interventions, and screening technologies. This model was used to evaluate clinical effectiveness and safety of the WCD therapy for primary and secondary prevention of SCA in patients over 18 years of age (under CE mark) and children (outside of CE mark) at risk. In addition, the focus group study strived to evaluate perspectives of patients on areas of their cardiac disease and on the WCD therapy. Furthermore, it aimed to detect possible neglected outcomes. Both the assessment and the focus group study intended to provide information on relevant aspects of the WCD use.
Methods
Systematic literature search, study selection, and internal validity
We conducted a comprehensive systematic literature search on July 14, 2016 in MEDLINE via OVID, Embase, the Cochrane Library, and CRD (DARE, NHS-EED, HTA) databases, without any restriction on timeframe or study design, which we complemented by a “Scopus search” (ie, citation tracking of three recent key publications of the WCD) and by hand search. We assessed registries of clinical trials to identify registered ongoing clinical trials and observational studies: ClinicalTrials.gov and International Clinical Trials Registry Platform. Furthermore, we performed a distinct guideline search (G-I-N, National Guidelines Clearinghouse, TRIP-Database, and hand search).
We applied inclusion criteria for the literature selection that were defined using the Population-Intervention-Comparison-Outcome-(Study design) model shown in Table 1. No minimum number of participants in a study was applied as an inclusion criterion. However, individual case reports were excluded. Furthermore, we did not consider studies discussing induced VT/VF in hospitals. Two researchers autonomously selected references for inclusion and assessed the internal validity of studies. In case of differences in the results, agreement was reached by discussion. A third researcher was contacted in case of disagreements. In order to assess the risk of bias of included prospective studies without a control group, the quality appraisal tool for case series was applied.9
  | Table 1 Inclusion criteria for selecting the literature according to the Population-Intervention-Comparison-Outcome-(Study design) model Note: Data from Ettinger et al.14 Abbreviations: AEs, adverse events; CABG, coronary artery bypass grafting; GL, guideline; HRQoL, health-related quality of life; ICD, implantable cardioverter defibrillator; LVEF, left ventricular ejection fraction; MI, myocardial infarction; PCI, percutaneous coronary intervention; RCTs, randomized controlled trials; SAEs, serious adverse events; SCA, sudden cardiac arrest; VF, ventricular fibrillation; VT, ventricular tachycardia; WCD, wearable cardioverter defibrillator. |
Data extraction and management
One researcher performed the extraction of data. The second researcher autonomously examined whether the data are correct and complete. A third researcher was contacted in case of disagreements, and differences were settled by discussion.
Outcome measures
Outcomes were selected according to the recommendations from pertinent clinical guidelines1,10 and were compliant with the EUnetHTA guidelines,11,12 which state that rapid REAs should be based whenever possible on final clinical end points relevant for patients (which mainly fall under the categories of mortality, morbidity, health-related quality of life [HRQoL]) and not surrogate end points. Furthermore, outcomes were discussed among the assessment team in consultation with a clinical cardiologist. Primary outcomes for the clinical effectiveness domain were all-cause mortality and disease-specific mortality (ie, prevention of SCA). Secondary outcomes were incidence of VT or VF, appropriate shocks and withheld shocks (use of response button for delaying therapy), first shock success, improvement of left ventricular ejection fraction (LVEF), avoidance of ICD implantation, HRQoL, hospitalization rate, satisfaction with the WCD, and patient compliance with the technology (WCD wear time, WCD daily use). For the safety domain, the outcomes were adverse events (AEs), frequency of discontinuation due to AEs, frequency of unexpected AEs, serious adverse events (SAEs), and frequency of SAEs leading to death.
Synthesis of evidence
The Grading of Recommendations, Assessment, Development and Evaluation – GRADE methodology – was used to summarize and evaluate the strength of the evidence.13 A classification (critical; important, but not critical; of limited importance) of the importance of the outcomes was performed. Only the outcomes that were considered critical were the primary factors influencing the conclusion. It was not possible to perform a meta-analysis because no prospective controlled studies were identified.
Other data sources and respective quality assessment
The manufacturer ZOLL Medical Corporation (Pittsburgh, PA, USA) was contacted on May 10, 2016 and asked to complete the EUnetHTA medical devices evidence submission file template, which mainly included questions on the WCD and its current use. The revised completed document was received on July 26, 2016. (ZOLL Medical Corporation, unpublished data, 2016). Relevant literature from the literature search and information from the submission file were used for the background. For ethical, organizational, patient, social, and legal questions, appropriate literature from the search was applied and complemented by a hand search for qualitative studies. No quality assessment tool was applied for these parts, but the use of several sources served in validation of individual, maybe biased, sources. After critical appraisal of these distinct information sources, their content was described.
Methodological framework
The present analysis was performed as the EUnetHTA collaborative assessment/HTA14 based on the EUnetHTA Core Model®, which is a methodological framework for the production and sharing of HTA information. It includes generic questions that are translated into actual research questions. In this context, the application for REA (version 4.2)15 including some additional questions from the ethical, organizational, patient, social, and legal domains of the EUnetHTA Core Model® (version 3.0),16 relevant for medical and surgical interventions, was used.
Reporting
This analysis was reported based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.17
Patient involvement – focus group study
The focus group represents a qualitative research method where a small group of participants discuss a topic guided by a moderator. It was selected as the most appropriate qualitative research method for involvement of patients in this context. It was the first time that patients were involved by means of a focus group study in an HTA by the EUnetHTA. A standardized e-mail reached members of the nine regional associations of the Austrian organization for heart and lung transplant patients aiming to find eligible patients/volunteers for the focus group. The aim was to include a small sample of patients who would have (had) an indication for the WCD. Semi-structured interview questions were developed by the assessment team and were based upon a hand search of patient involvement websites, such as the Scottish Medicine Consortium and its PACE process, and a review of appropriate literature.18,19 A set of questions was divided into three parts. The first part consists of engagement questions, the second part contains exploration questions, and the third part exit questions (Table 2). The four-hour meeting that was held in German was chaired by a patient support expert, who also assisted in finding and preparing volunteers for the focus group. The participants agreed that the meeting could be recorded. The anonymized transcript was analyzed based on framework analysis.18 Extraction of patient-relevant end points (clustering/charting), including main statements relevant for ethical, organizational, patient, social, legal, or other aspects of WCD use, was done by one researcher and checked by the second. Participants needed to provide informed consent as well as confirm that they had no conflict of interest and received remuneration. The Austrian Ethics Committee did not request an ethical approval with reference to section 15a, subsection 3a, of the Viennese Law on health institutions.
  | Table 2 Semi-structured interview questions of the focus group study Notes: This is a set of questions for patients who were diagnosed with any indication(s) that may lead to SCA, but who have not been treated with the LifeVest®. Questions were posed in German. Data from Ettinger et al.14 Abbreviations: AEs, adverse events; SCA, sudden cardiac arrest. |
Results
Search results
The systematic literature search yielded 601 references, and further 139 citations were identified through other sources (Figure 1). According to our selection criteria, no randomized controlled trials (RCTs) or non-randomized controlled trials assessing the clinical effectiveness of the WCD were found. For the assessment of safety, one prospective interventional single-arm study,20 two prospective case series,21,22 and two prospective registry studies23,24 fulfilled our inclusion criteria.
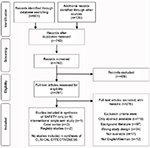  | Figure 1 Flow chart of the selection process according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.17 Note: Data from Ettinger et al.14 |
Study and patient characteristics
Study characteristics
The study inclusion criteria for the assessment of clinical effectiveness of the WCD were not met by any study.
A total of five non-comparative studies were included in the assessment of safety of the WCD: the prospective interventional single-arm study20 included 289 patients, two prospective case series included a total of 36 patients,21,22 and two prospective registry studies included a total of 2089 patients23,24 (Table 3).
  | Table 3 Results from prospective non-comparative studies – study/patient characteristics and safety outcomes Notes: aSource of funding was not stated. bTen centers. cFeb 1998 to July 2001 according to FDA approval document.43 dOne hundred and seventy-seven patients in WEARIT and 112 in BIROAD. eWCD recommended to 9 out of 12 patients, but two refused; hence, data were available on seven patients. fSixty-six consecutive patients of whom 24 (36%) were in the early post-MI phase. gOut of 89 patients, data on 82 were collected, four lost to follow-up, and three dropped out after wearing the WCD for a couple of hours. hIn an unspecified statistical measure. iUnclear, as the number 24.0±11.8% was also reported in the paper. jPatients followed biweekly and monthly, but no last follow-up stated. kEighty-one days (25–345) in seven women receiving a WCD. lAt 1, 3, and 12 months (12-month follow-up ongoing at time of paper). mPatient experienced numerous false alarms and “thus revealed reduced compliance to WCD wearing (16.3 hours/day)”. nIn WEARIT study: 30%; In BIROAD study: 11%; 65 patients discontinued due to comfort and lifestyle issues and three discontinued due to AEs. oSix patients discontinued due to discomfort and other reasons and seven due to unknown/other reasons. pDue to ECG artifacts while none due to induced VT/VF. qBoth occurred in patients who had incorrectly placed the therapy electrodes – one of the events was nonfatal as the patient received a successful external defibrillation. rOccurred in a patient who removed the leads. Data from Ettinger et al.14 Abbreviations: AADs, antiarrhythmic drugs; ACE, angiotensin-converting enzyme; AEs, adverse events; ARBs, angiotensin II receptor blockers; CABG, coronary artery bypass grafting; CM, cardiomyopathy; DCM, dilated cardiomyopathy; EF, ejection fraction; ICD, implantable cardioverter defibrillator; LVEF, left ventricular ejection fraction; MI, myocardial infarction; NA, not available; NYHA, New York Heart Association; PCI, percutaneous coronary intervention; PPCM, peripartum cardiomyopathy; SAEs, serious adverse events; SCA, sudden cardiac arrest; SD, standard deviation; VAs, ventricular arrhythmias; VT, ventricular tachycardia; WCD, wearable cardioverter defibrillator. |
Patient characteristics
Patient inclusion criteria within the included studies demonstrated some heterogeneity regarding LVEF (<30%,20 ≤40%,23 the other included studies did not report on this outcome) and in terms of the nature of heart disease (newly diagnosed peripartum cardiomyopathy,21 early post-myocardial infarction (MI)/MI phase,22 combination of several heart disease groups20,23,24). However, all patients were considered to be at high risk of SCA. Only two studies indicated having an active ICD and being unable to use the WCD because of impairment as exclusion criteria for study participants.20,23 Three out of five studies20,21,23 reported on previous patient treatments (Table 3).
Effectiveness
No RCTs or non-randomized controlled trials were found to assess the clinical effectiveness of the WCD.
Safety
Comparative studies
Since no study with a control group was identified, no assessment of relative safety of the WCD could be performed.
Non-comparative studies
Not all the included non-comparative studies reported on the different AEs and SAEs (Table 3). The following AEs were identified: skin rash and itching (in 6% of patients20), false alarms (in 14% of patients21), and palpitations, light-headedness, and fainting (in 9% of patients23); discontinuation due to comfort and lifestyle issues (in 22%20 and 16% of patients,23 respectively) was also reported. Unexpected AEs were not indicated in any of the included studies. SAEs mentioned were inappropriate shocks and unsuccessful shocks. The definition of inappropriate WCD therapy referred to non-VT/VF episodes detected and treated by a WCD shock.24 Two studies indicated that 2%20 and 0.5%24 of patients respectively were affected by inappropriate shocks. The other three studies indicated no inappropriate shocks. Four out of five studies mentioned unsuccessful shocks. In one study, 0.7% of patients20 experienced unsuccessful shocks because the therapy electrodes were placed incorrectly. Unsuccessful shocks21,22,24 were indicated in three studies and not reported in one study. All five studies indicated the frequency of SAEs leading to death, where death occurred in one study (0.3%)20 (Table 3). However, with reference to the GRADE methodology, the quality of the body of evidence of the studies included for the assessment of safety was very low (Table 4).
  | Table 4 Quality of the body of evidence of the studies included for the assessment of safety according to GRADE methodology13 Notes: aNo definition of skin rash/itching (severity, nature, location, etc.) was provided. There was no comparison group, and patients were not consecutively recruited. No data were gathered on psychological issues, eating habits, etc. It is unclear whether additional interventions have been performed (which could have caused side effects). bFew events were reported, and there was no control group. cSample size was very low. dPatients were not consecutively recruited, and there was no control group. No definition of nature and severity was provided. ePatients in both studies were not consecutively recruited. Patients might have been different with regard to confounding factors. fSince there was no control group, statement on mortality cannot be made. Data from Ettinger et al.14 Abbreviations: AEs, adverse events; NA, not applicable; SAEs, serious adverse events. |
Focus group results
Ten eligible patients (nine men and one woman) responded to the standardized email, among which five men, who were 55–73 years old (mean age 65 years) from Austria and Germany, were able to participate. All respondents had experienced heart transplantation, and four had received the ICD before. Patients who would have qualified for the WCD prior to their heart transplantation explained their disease history, and no one had experiences with using the WCD or had any knowledge regarding this technology. Only men volunteered for the focus group; therefore, no issues regarding gender could be assessed. Furthermore, the majority of patients were exercising competitive sports. Main results are summarized in Table 5.
  | Table 5 Main results from the focus group study Note: Data from a previous study.14 Abbreviations: HRQoL, health-related quality of life; ICD, implantable cardioverter defibrillator; QoL, quality of life; WCD, wearable cardioverter defibrillator. |
Discussion
No RCTs or non-randomized controlled studies were found to assess the clinical effectiveness of the WCD; therefore, strong evidence on patient benefit is missing. Since no comparative studies were available, assessment of relative safety of the WCD could not be performed. Results from five non-comparative studies comprising 2414 patients undergoing WCD therapy propose that the WCD might be a relatively safe intervention for a short-to-medium period of time, but the quality of the body of evidence was very low. The patients’ focus group study was successfully implemented, providing the data on ethical, organizational, patient, social, and legal aspects of the WCD use; for example, reservations of patients toward the WCD were identified.
At present, just one WCD, namely the LifeVest® produced by ZOLL Medical Corporation, is available. The patient needs to wear the WCD all day and night long, except while taking a bath or shower.25 The vest is worn around the chest of the patient and includes electrodes. The monitor is attached around the waist or carried using shoulder strap. The heart of the patient is permanently monitored, and in the event of a life-threatening heart rhythm like VT or VF that can be treated by the WCD, an automatic treatment shock is triggered. The conscious patient can press two response buttons on the monitor anytime during the treatment sequence in order to delay therapy. In Europe, the LifeVest® was granted CE mark for its first-generation model, WCD 1, in 1999, and for the latest fifth generation, WCD 4000, in 2011. The indication for the LifeVest® refers primarily to patients 18 years of age and older who are at risk of SCA and are not candidates for or refuse an ICD (ZOLL Medical Corporation, unpublished data, 2016). In the US, the LifeVest® was granted initial FDA approval in 2001; in 2015, it was also approved for children who are at risk of SCA, but are not candidates for an ICD because of certain medical conditions or in case the parents did not give their consent.26 To date, the WCD does not include pacing capabilities for backup bradycardia pacing or anti-tachycardia overdrive pacing.25,27 Therefore, particularly patients for whom ICDs are a comparator are left unprotected, because recent models of ICDs provide these functions.28 The WCD claims to temporarily protect from SCD in phases of enhanced risk during diagnosis or an event of post-VT/VF and the adequate therapy or its optimization.
Regarding safety of the WCD, AEs were not systematically reported in the included studies. The registry study including the highest number of participants (2000 patients) only outlined SAEs.24 Each one of the three smaller studies described distinct AEs: skin rash/itching, false alarms, and palpitations, light-headedness, and fainting.20,21,23 According to the literature, allergic contact dermatitis could be induced by metal hypersensitivity during the WCD use.29 Compliance with the WCD use might also be linked to climate: patients tend to wear it less during the summer season,30 which could also be associated with skin-related AEs. Three out of five included studies indicated earlier treatments,20,21,23 whereas none of the included studies outlined whether the patients received treatment in the course of the WCD use, which could have had an impact on part of the outcomes (ie, pharmacological therapy could result in side effects). AEs and SAEs stated were of importance to patients, but since there was a lack of reporting, this list might not be complete. Discontinuation due to comfort and lifestyle issues could be initiated by different causes: it is required to wear the WCD 24/7 that influences everyday life including routine. The focus group showed that patients might not want to wear the WCD in public, which further shows that user-dependent harms (such as unsuccessful shocks because of not having placed the therapy electrodes correctly,20 use of the response button without indication, and averting a treatment that could potentially save a life) could be connected to compliance and personal attitude. The WCD needs to be fitted to each patient; however, it could occur that some patients have difficulties in wearing it because of their body shape;31 that is, it could be an issue especially for women.
Results regarding unsuccessful shocks (in 0–0.7% of patients), inappropriate shocks (in 0–2% of patients), and frequency of SAEs leading to death (in 0–0.3% of patients) are homogenous. Further safety concerns could be bystander intervention and unsuccessful shocks due to signal interruption when the body falls and wedges.32 Inappropriate shocks could differ in the subgroups as well. The risk of motion-related sensory artifacts is enhanced in WCDs (compared to ICDs) because they are applied externally.27 Noise detected externally might also result in inappropriate shocks.31 The WCD could also possibly not be compatible with unipolar pacing devices.33 Furthermore, inappropriate WCD shocks have the potential to induce VF since they might not be synchronized in a correct way.34
The eventual autonomy and freedom gained in living a normal life through moving in the out-of-hospital setting needs to be balanced against the patient’s responsibility of having to decide between appropriate and inappropriate shocks. The focus group study stated that they would not want to decide whether to use the WCD’s response button or not. The patients indicated that they would be afraid of possibly preventing an appropriate therapy and that they lack the knowledge and the decision-making competence that clinicians possess, which is in line with previous research.35 Additionally, the autonomy is given at the expense of false security since the patients might understand that they are protected from all lethal arrhythmias and not just from VT and VF. The focus group also raised concerns about the WCD’s lack of pacing capabilities.
The principles of beneficence and non-maleficence have to be weighted. Uncertainties regarding the benefits of the WCD need to be discussed in contrast to the psychological benefit, that is, to feel secure and the opportunity for patients to remain in their normal surroundings. These highly subjective advantages need to be balanced with harms of which some might induce further arrhythmias that potentially result in death – contributing to psychological stress and fear/anxiety of technical failures.36,37 The focus group highlighted that experiencing a sense of security is crucial to them. They expected to be able to exercise, that is, to be athletes and to live with few restrictions despite receiving a therapy – which was the case when using the ICD. In addition, since relatives and/or caregivers should be around whenever the patient removes the garment25 and need to react after the WCD intervention, as the patient needs medical treatment post-shock,27 they may also be susceptible to a psychological harm caused by the fear or anxiety. The WCD therapy was not considered an option for weeks or even months by the focus group due to expected restrictions because of efforts of wearing it and possible issues with its weight. They were afraid of being permanently reminded of their disease by wearing the defibrillator on the outside instead of having it implanted.
Against the backdrop of the limited knowledge on the appropriate patient group for the device and because of the large indication group and an uncertain or marginal benefit, the question regarding the principle of distributional justice of investing resources in devices of unproven benefit while not investing the resources elsewhere needs to be posed. Furthermore, the costs of the WCD as recognized by physicians as well as the question of cost-effectiveness of the WCD for a quality-adjusted life year and cost-effectiveness thresholds of different countries might lead to difficulties in accessing the WCD.38,39 Due to the lack of effectiveness data, assumptions regarding the WCD’s cost-effectiveness are calculated referring to the marginal effect of the WCD in the included studies with higher number of participants (<2%) and the published cost-effectiveness analyses as referenced above.
The WCD invades the sphere of privacy through collecting data regarding heart functions of the patient and through submitting it to the particular cardiologists (ZOLL Medical Corporation, unpublished data, 2016). However, this manipulation of personal data could be justified in case the benefit of the WCD is confirmed.
A number of limitations need to be considered when reviewing the present results. The main limitation of this analysis is connected with the absence of high-quality data on clinical effectiveness as well as with the limited number and quality of studies included in the assessment of safety. Four of the five included studies were characterized by high risk of bias, and the fifth study to very high risk of bias.22 The limitations of the methodology were the following: study participants were not recruited consecutively,20,23,24 it is uncertain whether participants entered the study at a similar point in the disease status20,24 (or not meeting this criteria23), conflicts of interest or sources of funding for the study were not reported,20,22 and there was high loss to follow-up.20 Four studies received funding from the manufacturer ZOLL Medical Corporation, and the fifth study did not clearly indicate possible funding.22 Selection bias can especially occur in case series because patients are recruited from a specific population, that is, the hospital, which may not represent the general population appropriately (eg, multimorbidity, noncompliant personality traits). Because of the absence of comparators exposed to the same variables, effects shown could be a result of intervening effects (eg, in case of skin rash). The existing studies did not include the following relevant information: device model, settings of the monitor, number of response button use, number of false alarms, possible device–device interactions, information whether ICDs were indicated at the start of the WCD use and potentially could be avoided post-WCD use, and data on disease status (stage of disease) at baseline. Information on HRQoL and satisfaction with the WCD needs to be gathered using a standardized approach. Information on hospitalization would be of interest. Challenges regarding the focus group included the identification of participants representative for this patient group and the complexity of patient histories.
The AHA presented the WCD as a treatment option for VT and VF.7 Further, the WCD is seen as an option for primary prevention (in patients post-MI or post-explantation of an ICD when immediate reimplantation is not possible) and for secondary prevention (in patients with a history of SCA or sustained VT and VF, in whom ICD is ineffective). Further clarification and definition of the WCD’s role in treatment and prevention are needed.
It must be highlighted that there remain several opacities with regard to the WCD use. A clear definition of the target population for the WCD is required. The possibility of an overuse of the WCD is caused by the fear behind the risk of SCD. Therefore, more data40 on risk stratification of patients at high risk is needed. These data might be available, but until now have been just shown as part of larger subgroups. That produces skewed results and offers the WCD as the treatment option for the whole subgroup, although it is most needed for high-risk patient groups. One example is a study24 where former SCA and syncope patients at highest risk are included in the general subgroup of nonischemic cardiomyopathy (NICM). This study showed that patients with ischemic and congenital/inherited heart disease revealed significantly enhanced probabilities of sustained VT/VF than those with NICM.24 In a retrospective study, none of the 254 NICM patients received an appropriate WCD shock.41 Furthermore, appropriate shocks in the included studies varied between 1.1 and 8%20,22,24 up to 43%,21 although one registry study left this outcome unreported.23 The WCD was shown to have limited preventive impact; maximum of 2% of patients who used the LifeVest® experienced appropriate shocks in nearly any cohort (in total >8500 patients).31 More data on the use of WCD in individual patient populations are needed to better define highest risk groups.
A proper definition of risk factors for SCA is still outstanding and that further exacerbates the choice of appropriate indications for the WCD. Different baseline risks of patients need to be assessed, which could be done by conducting an individual patient data analysis. In addition, data on the management of patients who did not respond to the first-line therapy of SCA are lacking.
Previous reviews included different study designs for the assessment of clinical effectiveness and safety of the WCD. However, only the inclusion of prospective evidence can provide robust data, and therefore, the present HTA excluded retrospective studies. In 2014, the Haute Autorité de Santé in France published an HTA, which includes prospective and retrospective studies and provides a reimbursement recommendation for a selected number of indications: ICD explantation, awaiting cardiac transplant, and post-MI with low ejection fraction.5 The Blue Cross and Blue Shield Association in the US published a report in 2010,6 in which the authors include two studies regarding the WCD;20,42 the remainder of studies are referring to controlled trials of ICDs. The authors summarized that the two studies focused on detecting and aborting VT/VF, not on evaluating the WCD’s effect since no direct evidence in controlled trials was available to assess its efficacy in relation to comparators like usual treatments or alternatives, which is consistent with our results.
Conclusion
Since no prospective comparative studies on the use of the WCD are available, neither the assessment of clinical effectiveness nor the comparative assessment of safety with the standard treatments can be made. Non-comparative data indicate that the WCD might be a relatively safe intervention for a short-to-medium period of time, but the quality of available evidence is very low. AEs and SAEs need to be more appropriately reported in order to further evaluate the safety of the device. The literature search and the focus group yield important insights into patient-relevant outcomes and ethical, organizational, patient, social, and legal aspects of the WCD use, which should be taken into account when therapy options are discussed between clinicians and patients. More high-quality comparative data are needed on efficacy and safety of WCDs in order to determine the patient groups that would derive highest benefit from the intervention.
Acknowledgments
The authors would like to acknowledge the European Society of Cardiology (ESC). The collaboration with clinical societies, such as the ESC, is highly appreciated to ensure latest professional expertise in the field, to spread, and to disseminate the results. The authors thank Dr. Josef Kautzner for his comments on a draft version of the manuscript. The authors thank Prof. Dr. Diana Delić-Brkljačić and Dr. Olaf Weingart for serving as external experts in the EUnetHTA rapid REA of the WCD. Furthermore, the authors are grateful to Dr. Leonor Varela Lema, Janet Puñal Riobóo, Dr. Sebastian Grümer, and Dr. Stefan Sauerland for the review of the draft EUnetHTA rapid REA report. This work was supported by the European Commission in the framework of the 3rd EU Health Program, which funded the EUnetHTA Joint Action 3 (Grant Agreement No. 724130). Sole responsibility for its contents lies with the author(s), and neither the EUnetHTA nor the European Commission is responsible for any use that may be made of the information contained therein. Since 2006, the EUnetHTA projects aim at sustainably stimulating European collaboration and international information transfer in the field of HTA: in one EU project (EUnetHTA 2006–2008) and 2 Joint Actions (Joint Action 1 2010–2012 and Joint Action 2 2012–2015) involving around 70 HTA organizations from the EU and EFTA countries, processes and tools to reduce redundancies in EU-wide HTA production were developed. In Joint Action 3 (2016–2020), the aim is to support optional collaboration at scientific and technical level between HTA bodies to validate the model for joint work which should be continued after the Joint Action 3.
Disclosure
The authors report no conflicts of interest in this work.
References
Priori SG, Blomström-Lundqvist C, Mazzanti A, et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: the Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J. 2015;36(41):2793–2867. | ||
APA-OTS. Ärztekammer: Höhere Überlebensraten bei Herzstillstand sind machbar [Austrian Medical Chamber: higher survival rates in cardiac arrest patients are feasible]. 2013. Available from: http://www.ots.at/presseaussendung/OTS_20131015_OTS0124/aerztekammer-hoehere-ueberlebensraten-bei-herzstillstand-sind-machbar. Accessed September 29, 2016. German. | ||
Mozaffarian D, Benjamin EJ, Go AS, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–e322. | ||
Myerburg RJ, Juntilla MJ. Sudden cardiac death caused by coronary heart disease. Circulation. 2012;125(8):1043–1052. | ||
Haute Autorité de Santé. LifeVest 4000. St Denis: Haute Autorité de Santé; 2014. | ||
BlueCross Blue Shield Association (BCBSA) Technology Evaluation Center (TEC). Wearable Cardioverter-Defibrillator as a Bridge to Implantable Cardioverter-Defibrillator Treatment. Chicago, IL: Blue Cross Blue Shield Association (BCBSA); 2010. | ||
Piccini JP Sr, Allen LA, Kudenchuk PJ, Page RL, Patel MR, Turakhia MP; American Heart Association Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology and Council on Cardiovascular and Stroke Nursing. Wearable cardioverter-defibrillator therapy for the prevention of sudden cardiac death: a science advisory from the American Heart Association. Circulation. 2016;133(17):1715–1727. | ||
Reek S, Burri H, Roberts PR, et al; EHRA Scientific Documents Committee (as external reviewers). The wearable cardioverter-defibrillator: current technology and evolving indications. Europace. 2017;19(3):335–345. | ||
Moga C, Guo B, Schopflocher D, Harstall C. Development of a Quality Appraisal Tool for Case Series Studies Using a Modified Delphi Technique. Edmonton, AB: Institute of Health Economics; 2012. | ||
Klein HU, Goldenberg I, Moss AJ. Risk stratification for implantable cardioverter defibrillator therapy: the role of the wearable cardioverter-defibrillator. Eur Heart J. 2013;34(29):2230–2242. | ||
European Network for Health Technology Assessment (EUnetHTA). Endpoints used in relative effectiveness assessment: surrogate endpoints. 2015. Available from: http://www.eunethta.eu/outputs/endpoints-used-relative-effectiveness-assessment-surrogate-endpoints-amended-ja1-guideline-f. Accessed June 6, 2016. | ||
European Network for Health Technology Assessment (EUnetHTA). EUnetHTA guidelines. 2015. Available from: http://www.eunethta.eu/eunethta-guidelines. Accessed June 6, 2016. | ||
Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–406. | ||
Ettinger S, Stanak M, Huic M, et al. Wearable cardioverter-defibrillator therapy in primary and secondary prevention of sudden cardiac arrest in patients at risk. Rapid assessment on other health technologies using the HTA Core Model for Rapid Relative Effectiveness Assessment. EUnetHTA Project ID: OTCA01. 2016. Available from: http://www.eunethta.eu/outputs/1st-collaborative-assessment-wearable-cardioverter-defibrillator-wcd-therapy-primary-and-sec. Accessed January 31, 2017. | ||
European Network for Health Technology Assessment (EUnetHTA). Rapid relative effectiveness assessments (4.2). 2016. Available from: http://meka.thl.fi/htacore/ViewApplication.aspx?id=25468. Accessed June 6, 2016. | ||
European Network for Health Technology Assessment (EUnetHTA). HTA Core Model. 2016. Available from: http://meka.thl.fi/htacore/BrowseModel.aspx. Accessed June 6, 2016. | ||
Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [Updated March 2011]. London: The Cochrane Collaboration; 2011. | ||
Durand MA, Chantler T. Principles of Social Research. London: Open University Press; 2014. | ||
Fried A, Wild C. Beteiligung von BürgerInnen und PatientInnen in HTA Prozessen. Internationale Erfahrungen und Good Practice Beispiele [Participation of Citizens and Patients in HTA Processes. International Experience and Good Practice Examples]. Wien: Ludwig Boltzmann Institut für Health Technology Assessment; 2016. German. | ||
Feldman AM, Klein H, Tchou P, et al; WEARIT investigators and coordinators; BIROAD investigators and coordinators. Use of a wearable defibrillator in terminating tachyarrhythmias in patients at high risk for sudden death: results of the WEARIT/BIROAD.[Erratum appears in Pacing Clin Electrophysiol. 2004 May;27(5):following table of contents]. Pacing Clin Electrophysiol. 2004;27(1):4–9. | ||
Duncker D, Haghikia A, König T, et al. Risk for ventricular fibrillation in peripartum cardiomyopathy with severely reduced left ventricular function-value of the wearable cardioverter/defibrillator. Eur J Heart Fail. 2014;16(12):1331–1336. | ||
Kondo Y, Linhart M, Andrié RP, Schwab JO. Usefulness of the wearable cardioverter defibrillator in patients in the early post-myocardial infarction phase with high risk of sudden cardiac death: a single-center European experience. J Arrhythm. 2015;31(5):293–295. | ||
Kao AC, Krause SW, Handa R, et al; Wearable defibrillator use In heart Failure (WIF) Investigators. Wearable defibrillator use in heart failure (WIF): results of a prospective registry. BMC Cardiovasc Disord. 2012;12:123. | ||
Kutyifa V, Moss AJ, Klein H, et al. Use of the wearable cardioverter defibrillator in high-risk cardiac patients: data from the Prospective Registry of Patients Using the Wearable Cardioverter Defibrillator (WEARIT-II Registry). Circulation. 2015;132(17):1613–1619. | ||
Chung MK. The role of the wearable cardioverter defibrillator in clinical practice. Cardiol Clin. 2014;32(2):253–270. | ||
US Food and Drug Administration (FDA). FDA approves wearable defibrillator for children at risk for sudden cardiac arrest. 2015. Available from: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm466852.htm. Accessed April 14, 2016. | ||
Adler A, Halkin A, Viskin S. Wearable cardioverter-defibrillators. Circulation. 2013;127(7):854–860. | ||
Ganz LI. General principles of the implantable cardioverter-defibrillator. Uptodate. 2016. Available from: http://www.uptodate.com/contents/general-principles-of-the-implantable-cardioverter-defibrillator. Accessed October 5, 2016. | ||
Garner AM, Aneja S, Jahan-Tigh RR. Allergic dermatitis from a defibrillator vest. Dermatitis. 2016;27(3):151. | ||
Cronin EM, Bianco NR, Chung R, et al. Abstract 14183: some like it cool-seasonal temperature, as well as clinical and demographic factors, predicts compliance with the wearable cardioverter defibrillator. Circulation. 2011;124 (Suppl 21):A14183. | ||
Chung MK. Wearable cardioverter-defibrillator. In: Page RL, Downey BC, editors. UpToDate. Waltham, MA: UpToDate; 2016. | ||
Chung MK, Szymkiewicz SJ, Shao M, Niebauer MJ, Lindsay BD, Tchou PJ. Aggregate national experience with the wearable cardioverter-defibrillator vest: event rates, compliance and survival. J Am Coll Cardiol. 2010;55(10):A10.E98. | ||
LaPage MJ, Canter CE, Rhee EK. A fatal device-device interaction between a wearable automated defibrillator and a unipolar ventricular pacemaker. Pacing Clin Electrophysiol. 2008;31(7):912–915. | ||
Francis J, Reek S. Wearable cardioverter defibrillator: a life vest till the life boat (ICD) arrives. Indian Heart J. 2014;66(1):68–72. | ||
Gawande A. Complications: A Surgeon’s Notes on a Imperfect Science. New York: Picador; 2002. | ||
Lenarczyk R, Potpara TS, Haugaa KH, Hernández-Madrid A, Sciaraffia E, Dagres N; Scientific Initiatives Committee, European Heart Rhythm Association. The use of wearable cardioverter-defibrillators in Europe: results of the European Heart Rhythm Association survey. Europace. 2016;18(1):146–150. | ||
Ketilsdottir A, Albertsdottir HR, Akadottir SH, Gunnarsdottir TJ, Jonsdottir H. The experience of sudden cardiac arrest: becoming reawakened to life. Eur J Cardiovasc Nurs. 2014;13(5):429–435. | ||
La Page MJ, Saltzman GM, Schumacher KR. Cost effectiveness of the wearable automated defibrillator for primary prevention in pediatric heart transplant candidates. J Card Fail. 2013;19(8):S64. | ||
Kondo Y, Kurita T, Ueda M, et al. Efficacy and cost-effectiveness of wearable cardioverter-defibrillator as a lifesaving-bridge therapy for decision in high risk Japanese patients of sudden arrhythmic death. Heart Rhythm. 2016;13(5):S150. | ||
Adelstein E, Voigt A, Saba S, Wang N, Jain S, Singh M. Reply: no utility of the wearable cardioverter-defibrillator in patients with nonischemic cardiomyopathy? J Am Coll Cardiol. 2016;67(23):2808. | ||
Singh M, Alluri K, Voigt A, et al. Abstract 12637: utility of the wearable cardioverter-defibrillator for patients with newly diagnosed non-ischemic cardiomyopathy? Circulation. 2014;130 (Suppl 2):A12637. | ||
Auricchio A, Klein H, Geller CJ, Reek S, Heilman MS, Szymkiewicz SJ. Clinical efficacy of the wearable cardioverter-defibrillator in acutely terminating episodes of ventricular fibrillation. Am J Cardiol. 1998;81(10):1253–1256. | ||
U.S. Food and Drug Administration. Premarket approval (PMA). 2016 [cited August 22, 2016]. Available from: http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?id=P010030. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
