Back to Journals » Neuropsychiatric Disease and Treatment » Volume 10
Vitamin B12, folate, and homocysteine levels in patients with obsessive–compulsive disorder
Authors Türksoy N, Bilici R, Yalçiner A, Özdemir Y , Örnek I, Tufan AE , Kara A
Received 13 May 2014
Accepted for publication 10 June 2014
Published 9 September 2014 Volume 2014:10 Pages 1671—1675
DOI https://doi.org/10.2147/NDT.S67668
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Nuray Türksoy,1 Rabia Bilici,2 Altan Yalçiner,3 Y Özay Özdemir,2 Ibrahim Örnek,4 Ali Evren Tufan,5 Ayşe Kara6
1Simurg Psychiatry and Psychotherapy Center, Istanbul, 2Erenköy State Hospital for Psychiatric and Neurological Diseases, Istanbul, 3Düzen Laboratories, Istanbul, 4Florence Nightingale Hospital, Istanbul, 5Department of Child and Adolescent Psychiatry, Abant Izzet Baysal University, Bolu, 6Bakırköy State Hospital for Psychiatric and Neurological Diseases, Istanbul, Turkey
Abstract: It is known that elevated serum homocysteine, decreased folate, and low vitamin B12 serum levels are associated with poor cognitive function, cognitive decline, and dementia. Current literature shows that some psychiatric disorders, mainly affective and psychotic ones, can be related to the levels of vitamin B12, folate, and homocysteine. These results can be explained by the importance of vitamin B12, folate, and homocysteine in carbon transfer metabolism (methylation), which is required for the production of serotonin as well as for other monoamine neurotransmitters and catecholamines. Earlier studies focused on the relationship between folate deficiency, hyperhomocysteinemia, and depressive disorders. Although depressive and anxiety disorders show a common comorbidity pattern, there are few studies addressing the effect of impaired one-carbon metabolism in anxiety disorders – especially in obsessive–compulsive disorder (OCD). This study aimed to measure the levels of vitamin B12, folate, and homocysteine specifically in order to see if eventual alterations have an etiopathogenetic significance on patients with OCD. Serum vitamin B12, folate, and homocysteine concentrations were measured in 35 patients with OCD and 22 controls. In addition, the Structured Clinical Interview for the Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition, Text Revision, Yale–Brown Obsessive Compulsive Scale, Hamilton Rating Scale for Depression, and Hamilton Rating Scale for Anxiety were conducted for each patient. It was found that vitamin B12 levels were decreased and homocysteine levels were increased in some OCD patients. Homocysteine levels were positively correlated with Yale–Brown compulsion and Yale–Brown total scores. In conclusion, findings of this study suggest that some OCD patients might have vitamin B12 deficiency and higher homocysteine levels.
Keywords: obsessive–compulsive disorder, vitamin B12, folate, homocysteine, obsession, compulsion
Introduction
It is reported that psychiatric symptoms – mainly affective and psychotic ones – can be related to the levels of vitamin B12, folate, and homocysteine.1–5 These observations may be explained by the importance of vitamin B12, folate, and homocysteine in carbon transfer metabolism (methylation), which is required for the production of serotonin, other monoamine neurotransmitters, and catecholamines.6 Earlier studies focused on the relationship between folate deficiency and depressive disorders.7,8 These were followed by several case-controlled studies which revealed increasing prevalence of folate and vitamin B12 deficiency in patients with depression.9,10 Recently, homocysteine has been considered as a sensitive marker for folate deficiency.11,12 Observations on the antidepressant effects of folate supplementation may support the importance of these nutrients in psychopathology.13,14 Although comorbidity of depressive and anxiety disorders is common, there are few studies addressing the effect of impaired one-carbon metabolism in anxiety disorders – especially in obsessive–compulsive disorder (OCD).15–18 OCD shows a prevalence of 1%–3% globally, and it follows a chronic course with increased rates of comorbidity. Thus, it is a global burden on the patients as well as on their families, ie, it decreases the quality of life for both of these parties.19–22 Due to the role of OCD in the quality of life of patients and their families, as well as providing an alternative route of augmentation for pharmacotherapy, further studies investigating the roles of vitamin B12, folate and homocysteine may be worthwhile to carry out. Therefore, this study’s aim was to measure vitamin B12, folate, and homocysteine levels specifically to see whether or not their eventual alterations play a role in the etiopathogenesis and/or subsequent course of OCD.
Materials and methods
Patients who were diagnosed with OCD according to the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria were approached and informed about the aims and methods of the study. Among the patients, the ones who did not have mental retardation and/or psychosis, and the ones who provided their informed consent were enrolled in the study. Other exclusion criteria were defined as the history of any endocrinological condition, being pregnant, lactating or having childbearing potential, having clinically relevant abnormal laboratory test results, including megaloblastic anemia, alcohol abuse and dependence and a positive history of immunologic disease. Twenty-two healthy control subjects who matched with the patients in terms of sex and age were chosen from the hospital staff according to exclusion criteria. The controls were interviewed with the non-patient version of the Structured Clinical Interview for the revised third edition of the DSM to exclude any Axis I Disorder.23 In addition, the controls did not have a history of major mood disorder, dementia, mental retardation, or psychosis in their first-degree relatives. All control subjects had either no history of treatment or were drug-free at least for the last 2 weeks.
The patients were diagnosed with the Structured Clinical Interview for DSM-IV Axis I Disorders.24 The Hamilton Rating Scale for Depression,25 Hamilton Rating Scale for Anxiety,26 and Yale–Brown Obsessive–Compulsive Scale27 were used for evaluating severity and comorbidities.
Venous blood samples were collected after overnight fasting. Homocysteine, folate, and vitamin B12 levels were measured in all subjects. Blood was drawn into tubes containing ethylenediaminetetraacetic acid/K3, immediately placed on ice, and centrifuged at 4°C. Plasma was separated and immediately stored at −80°C before it was analyzed. Cutoffs (given below) were used to determine vitamin deficiency. As described in the literature, they corresponded to the normal ranges of the assays. Folate deficiency was considered to be present when the serum folate level was <3 ng/mL. Vitamin B12 deficiency was defined as a level of serum vitamin B12 <200 pg/mL.16 Hyperhomocysteinemia was defined as a level of plasma homocysteine >14.0 μmol/L.17
SPSS for Windows version 15.0 (2006; SPSS Inc., Chicago, IL, USA) was used in the statistical analyses. Descriptive statistics were performed with frequency and cross tabulations for categorical variables. Means and standard deviations were measured for numerical variables. The chi-square test was used for comparing independent categorical variables. Monte Carlo simulations were run for multiple groups when comparisons did not meet the chi-square criteria; Fisher’s exact test was used in the comparison of the groups. Student’s t-test was used for comparing the numerical data displaying normal distribution; the Mann–Whitney U-test was performed for the numerical variables not displaying normal distribution. The P-value was set at 0.05 and all of the comparisons were two-tailed.
Results
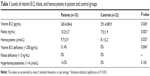
While the mean age of the patient group was 34.0±10.5 years, it was 33.1±8.3 years in the controls. The patient and control groups were mostly female (88.6% and 86.4%, respectively). The groups had no significant differences in terms of their sociodemographic data.
The mean age at onset of OCD was 22.1±8.5 years and the mean duration of OCD was 141.8±111.0 months in the patient group.
There were no significant differences between the patients and controls in terms of hemoglobin values (13.3±1.4 g/dL and 13.8±1.5 g/dL, respectively; P=0.125). The groups were then compared according to folate, vitamin B12, and homocysteine levels. The results showed that all three variables differed significantly (Table 1).
Among the 35 cases with OCD, 31 (88.6%) showed good insight; nine (15.8%) of them were diagnosed with comorbid major depressive disorder according to DSM-IV criteria. Among the ones who were diagnosed with OCD, 34 patients reported a history of treatment for the disorder (97.1%), while four (18.2%) of the control subjects declared that they had received psychiatric help in the past for problems not related to anxiety/mood disorders. Thirty-two patients (91.4%) were taking antiobsessive medicine during the study.
Compared to the control group, the level of vitamin B12 was significantly lower in the patient group (245.4±84.6 versus 291.4±80.9 pg/mL, respectively; P=0.036). The rate of vitamin B12 deficiency (<200 pg/mL) was 31.4% in the patient group, while there was no vitamin B12 deficiency in the control group (Figure 1). The difference between the groups was statistically significant (P=0.004). Although there was no folate deficiency in either of the groups, the level of homocysteine was found to be significantly higher in the patient group compared to the control group (9.7±2.9 versus 8.1±2.2 μmol/L, respectively; P=0.032). While the highest level of homocysteine was observed in the OCD group with major depressive disorder, the lowest level of homocysteine was in the controls. Levels of the group with OCD without major depressive disorder ranged between the mean averages of these two groups (P=0.06).
  | Figure 1 Scatter plot of serum vitamin B12 levels of obsessive–compulsive disorder patients and controls. |
While hyperhomocysteinemia (>14 μmol/L) was not found in the control group at all, a rate of 14.3% was observed in the patient group. However, this difference was not considered statistically significant (P=0.145).
In the patient group, Spearman’s correlation analysis was performed between levels of vitamin B12, folate, and homocysteine; scores of the Hamilton Rating Scale for Anxiety, Hamilton Rating Scale for Depression, and Yale–Brown Obsession Scale; Yale–Brown compulsion and Yale–Brown total scores; and duration of disease. A statistically significant positive correlation was observed between levels of homocysteine and Yale–Brown compulsion (P=0.021, ρ=0.389) and Yale–Brown total scores (P=0.044, ρ=0.342).
Discussion
There are only a few current studies regarding folate, vitamin B12, and homocysteine values in patients with anxiety disorders – especially with OCD. Hermesh et al indicated that vitamin B12 deficiency was more frequent in OCD patients than controls.15 This suggests that obsessive–compulsive symptoms can be a marker for vitamin B12 deficiency and predicts more well-known symptoms of it. Sharma and Biswas reported a case of a middle-aged male patient presenting with OCD, low levels of serum vitamin B12, and a positive family history of vitamin B12 deficiency who responded well to methylcobalamin replacement.18 Based on this, they suggested a possible etiological role of vitamin B12 in OCD.18 Atmaca et al reported that serum folate values were significantly lower in OCD patients than controls, while homocysteine concentrations were higher in patients compared to controls.16
In the current study, it was found that vitamin B12 levels were decreased and homocysteine levels were increased in at least some of the patients with OCD. Among the OCD patients, the rate of vitamin B12 deficiency was significantly higher compared to the control group while folate deficiency was not found in either group. The rate of hyperhomocysteinemia in the OCD patients seemed to be higher than the control group, although the difference did not have statistical significance. Hyperhomocysteinemia was observed in mood disorders, especially in depressive states, in several studies.9–11 The current finding that the level of homocysteine was most frequent in the group with major depressive disorder may be suggestive of this well-documented relationship, although the association with OCD in general is intriguing and may justify further research.
Hermesh et al suggested that it might point to the possibility that vitamin B12 deficiency characterizes a subgroup of OCD patients.15 Atmaca et al also indicated that folate levels in those patients were significantly and negatively correlated with the scores on the Yale–Brown Obsessive–Compulsive Scale while levels of homocysteine were positively correlated with the duration of illness and Yale–Brown Obsessive–Compulsive Scale scores.16 In the current study, homocysteine levels had a statistically significant positive correlation with Yale–Brown compulsion and Yale–Brown total scores. Considering that the current sample largely consisted of patients who had received previous antiobsessive treatment but had not benefited from it, the high rates of B12 deficiency (and, to a degree, high homocysteine) may be suggestive of a selected group featuring a larger than usual representation of a patient subgroup resistant to treatment in addition to high rates of vitamin B12 deficiency (and hyperhomocysteinemia).
Conclusion
This study showed that some of the patients with OCD had vitamin B12 deficiency and higher homocysteine levels. However, the sample was too small to conclude that this finding is an important biological indicator for OCD. Although more detailed studies regarding this phenomenon are to be carried out, these findings can provide a starting point for future research.
Acknowledgment
The authors would like to express their thanks to the Istanbul Offices of Düzen Laboratories for providing the laboratory analyses of the blood samples used in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
Fafouti M, Paparrigopoulos T, Liappas J, Mantouvalos V, Typaldou R, Christodoulou G. Mood disorder with mixed features due to vitamin B12 and folate deficiency. Gen Hosp Psychiatry. 2002;24(2):106–109. | ||
Stanger O, Fowler B, Piertzik K, et al. Homocysteine, folate, and vitamin B12 in neuropsychiatric diseases: review and treatment recommendations. Expert Rev Neurother. 2009;9(9):1393–1412. | ||
Kale A, Naphade N, Sapkale S, et al. Reduced folic acid, vitamin B12, and docosahexaenoic acid and increased homocysteine and cortisol in never-medicated schizophrenia patients: implications for altered one-carbon metabolism. Psychiatry Res. 2010;175(1–2):47–53. | ||
Kim TH, Moon SW. Serum homocysteine and folate levels in Korean schizophrenic patients. Psychiatry Investig. 2011;8(2):134–140. | ||
Ezzaher A, Mouhamed DH, Mechri A, et al. Hyperhomocysteinemia in Tunisian bipolar I patients. Psychiatry Clin Neurosci. 2011;65(7): 664–671. | ||
Bottiglieri T. Folate, vitamin B12, and neuropsychiatric disorders. Nutr Rev. 1997;54(12):382–390. | ||
Coppen A, Swade C, Jones SA, Armstrong RA, Blair JA, Leeming RJ. Depression and tetrahydrobiopterin: the folate connection. J Affect Disord. 1989;16(2–3):103–107. | ||
Bottiglieri T, Laundy M, Crellin R, Toone BK, Carney MW, Reynolds EH. Homocysteine, folate, methylation, and monoamine metabolism in depression. J Neurol Neurosurg Psychiatry. 2000;69(2):228–232. | ||
Sachdev PS, Parslow RA, Lux O, et al. Relationship of homocysteine, folic acid, and vitamin B12 with depression in a middle-aged community sample. Psychol Med. 2005;35(4):529–538. | ||
Kim JM, Stewart R, Kim SW, Yang SJ, Shin IS, Yoon JS. Predictive value of folate, vitamin B12, and homocysteine levels in late-life depression. Br J Psychiatry. 2008;192(4):268–274. | ||
Stabler SP, Marcell PD, Podell ER, Allen RH, Savage DG, Lindenbaum J. Elevation of total homocysteine in the serum of patients with cobalamin or folate deficiency detected by capillary gas chromatography-mass spectrometry. J Clin Invest. 1988;81(2):466–474. | ||
Lindenbaum J, Healton EB, Savage DG, et al. Neuropsychiatric disorders caused by cobalamin deficiency in the absence of anemia or macrocytosis. N Engl J Med. 1988;318(26):1720–1728. | ||
Alpert JE, Mischoulon D, Rubenstein GE, Bottonari K, Nierenberg AA, Fava M. Folinic acid (leucovorin) as an adjunctive treatment for SSRI-refractory depression. Ann Clin Psychiatry. 2002;14(1):33–38. | ||
Başoğlu C, Alpay Ateş M, Algül A, et al. Adjuvant folate with escitalopram treatment and homocysteine, folate, vitamin B12 levels in patients with major depressive disorder. Bulletin of Clinical Psychopharmacology. 2009;19(2):135–142. | ||
Hermesh H, Weizman A, Shahar A, Munitz H. Vitamin B12 and folic acid serum levels in obsessive compulsive disorder. Acta Psychiatr Scand. 1988;78(1):8–10. | ||
Atmaca M, Tezcan E, Kuloglu M, Kirtas O, Ustandag B. Serum folate and homocysteine levels in patients with obsessive–compulsive disorder. Psychiatry Clin Neurosci. 2005;59(5):616–620. | ||
Levine J, Timinsky I, Vishne T, et al. Elevated serum homocysteine levels in male patients with PTSD. Depress Anxiety. 2008;25(11): E154–E157. | ||
Sharma V, Biswas D. Cobalamin deficiency presenting as obsessive compulsive disorder: case report. Gen Hosp Psychiatry. 2012; 34(5):e7–e8. | ||
Fireman B, Koran LM, Leventhal JL, Jacobson A. The prevalence of clinically recognized obsessive–compulsive disorder in a large health maintenance organization. Am J Psychiatry. 2001;158(11): 1904–1910. | ||
Tükel R, Polat A, Özdemir Ö, Aksüt D, Türksoy N. Comorbid conditions in obsessive–compulsive disorder. Compr Psychiatry. 2002;43(3): 204–209. | ||
Türksoy N, Tükel R, Özdemir Ö, Karali A. Comparison of clinical characteristics in good and poor insight obsessive–compulsive disorder. J Anxiety Disord. 2002;16(4):413–423. | ||
Gururaj GP, Math SB, Reddy JY, Chandrashekar CR. Family burden, quality of life, and disability in obsessive compulsive disorder: an Indian perspective. J Postgrad Med. 2008;54(2):91–97. | ||
Spitzer RL, Williams JBW, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R, Non-patient Edition (SCID-NP). Washington, DC: American Psychiatric Press; 1990. | ||
First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinical Version (SCID-CV). Washington, DC: American Psychiatric Press; 1996. | ||
Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychology. 1967;6(4):278–296. | ||
Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32(1):50–55. | ||
Goodman WK, Price LH, Rasmussen SA, et al. The Yale–Brown Obsessive–Compulsive Scale: I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46(11):1006–1011. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.