Back to Journals » Clinical Ophthalmology » Volume 10
Visual, aberrometric, photic phenomena, and patient satisfaction after myopic wavefront-guided LASIK using a high-resolution aberrometer
Authors Moussa S, Dexl AK, Krall EM, Arlt EM, Grabner G, Ruckhofer J
Received 8 March 2016
Accepted for publication 9 June 2016
Published 12 December 2016 Volume 2016:10 Pages 2489—2496
DOI https://doi.org/10.2147/OPTH.S108002
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Sarah Moussa, Alois K Dexl, Eva M Krall, Eva M Arlt, Günther Grabner, Josef Ruckhofer
Department of Ophthalmology, Paracelsus Medical University Salzburg, Salzburg, Austria
Purpose: The purpose of this study was to evaluate the visual, refractive, and aberrometric outcomes as well as the level of patient satisfaction and photic phenomena after myopic laser in situ keratomileusis (LASIK) surgery using wavefront-guided (WFG) ablations based on measurements obtained with a high-resolution aberrometer.
Patients and methods: This study was a prospective analysis including 253 eyes of 127 patients (aged between 19 years and 54 years) undergoing WFG LASIK using the STAR S4 IR Excimer Laser System combined with the iDesign System and iFS Femtosecond Laser. Visual, refractive, and aberrometric outcomes during a 2-month follow-up as well as patient satisfaction and photic phenomena were evaluated by means of a questionnaire.
Results: A total of 85% (215/253) and 99% (251/253) of eyes achieved a postoperative (Postop) uncorrected distance visual acuity of 20/16 and 20/20, respectively, and all eyes achieved an uncorrected distance visual acuity of 20/25. Postop spherical equivalent values were within ±0.25 D and ±0.50 D in 97% and 100% of eyes, respectively. Likewise, manifest cylinder was <0.25 D in 97% (245/253) of eyes. A statistically significant reduction was found in the total root mean square (P<0.001) and in the level of primary spherical aberration (P=0.001). Postop difficulties related to vision were graded as minimal, with low levels of photic phenomena and high levels of patient satisfaction. The level of difficulty to perform daily activities and the level of glare perceived by patients while driving car were significantly decreased (P<0.001).
Conclusion: WFG LASIK surgery using the technology evaluated is predictable and effective for the correction of myopia and leads to high levels of patient satisfaction.
Keywords: LASIK, patient satisfaction, Wave-front guided LASIK, high resolution aberrometer, photic phenomena, glare
Introduction
The use of accurate static references for centration, the improvement of accuracy of wavefront aberration measurements, and the refinement of ablation profiles are technological advances that have led the corneal refractive surgery to a high level of efficacy, predictability, and accuracy.1–3 Specifically, these advances have allowed surgeons to overcome some limitations concerning the characterization of ocular aberrations and therefore to obtain improved outcomes using wavefront-guided (WFG) ablation profiles, even in the more complex cases.2,4–6 There is a variety of studies confirming the safety and efficacy of WFG laser in situ keratomileusis (LASIK) for the correction of spherocylindrical refractive errors with the latest laser platforms as well as the ability of these treatments to minimize the induction of higher order aberrations (HOAs) and reduce the level of some preexisting HOAs.1–3,5–15
Although the evidence on the objective improvement in visual, refractive, optical, and visual quality parameters with WFG treatments is consistent, there is still limited scientific evidence on the subjective benefit of these procedures for patients in terms of patient satisfaction and reduction of photic phenomena. He and Manche16 evaluated patient self-reported visual symptoms at 1 year after surgery in eyes undergoing WFG LASIK and wavefront-optimized (WFO) photorefractive keratectomy. The average of all symptoms was lower in eyes receiving the WFO treatments, although the differences did not reach statistical significance.16 Yu et al17 found that the rate of visual symptoms, such as glare, halo, and night driving difficulty, decreased after WFG LASIK. The aim of the current study was to evaluate the visual, refractive, and aberrometric outcomes as well as the incidence of photic phenomena and the level of patient satisfaction after LASIK surgery for the correction of myopia using WFG profiles designed according to the aberrometric measurements obtained with a new high-resolution aberrometer.
Patients and methods
Patients
This study was a prospective analysis including 253 eyes of 127 patients (aged between 19 years and 54 years) undergoing LASIK for the correction of myopia or myopic astigmatism. Written informed consent was obtained from all 127 patients before being enrolled in the study. Subjects were informed about his or her rights, the purpose of the study, the procedures to be undergone, and the potential risks and benefits of participation. The sample included a total of 253 eyes, with a mean preoperative (Preop) manifest spherical equivalent (SE) value of −4.41±1.94 D (range −0.75 D to −9.50 D) and a mean cylinder value of −0.85±0.72 D (range −4.75–0.00 D). The mean age of patients included in the study was 33.7±9.4 years (range 19–54 years).
The Advanced CustomVue platform (Abbott Medical Optics Inc, Santa Ana, CA, USA) was used in this study. This platform combines the VISX STAR S4 IR Excimer Laser System and the new Hartmann–Shack aberrometer iDesign (Abbott Medical Optics Inc). The exclusion criteria for the study were hyperopia or hyperopic astigmatism, a residual corneal stromal bed of <300 μm after programming the laser ablation, age <18 years, previous corneal or intraocular surgery, active ocular pathology, a history of uveitis, autoimmune disease, and a history of recurrent corneal erosion or epithelial basement dystrophy. Users of soft contact lens and rigid gas permeable contact lens were asked to remove their lenses at least 2 weeks or 1 month prior to the Preop examination. All flaps were created using the iFS Femtosecond Laser (Abbott Medical Optics Inc).
Since the study involved only CE-marked technology and all tests performed were within the routine practice of the hospital, no ethics committee approval was required.
Clinical protocol
All patients underwent a complete Preop ophthalmological examination that included measurement of uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), manifest and cycloplegic refraction, biomicroscopy, corneal topography, ultrasound pachymetry, intraocular pressure measurement, aberrometry (4 mm and 5 mm pupils), and dilated fundoscopy. All patients followed the same postoperative (Postop) schedule of visits, including 1 day, 1 week, and 2 months after surgery. The Postop examinations included UDVA and CDVA, corneal topography, biomicroscopy, and intraocular pressure measurement. Besides these tests, patient satisfaction and the incidence of photic phenomena were evaluated Preop and at 2 months postoperatively by means of a self-developed questionnaire. Specifically, the patients were asked to score the difficulty and complaints associated with some activities as well as the incidence of some visual symptoms (scale 0= best score and 9= worst score): difficulty with daily activities, dry eye problems, problems due to changes in visual performance during the day, double image, glare/halos at night, glare/halos during work, glare/halos during car driving, glare/halos while watching TV or working with the computer, and glare/halos at night when lightened traffic signs are visualized. Likewise, the following questions were asked postoperatively to assess the level of patient satisfaction with the surgery outcome: is visual performance better compared to your Preop expectations?, would you do the same surgery again?, how satisfied are you with your vision?, did your quality of life improve after surgery?, and would you recommend the surgery to friends and relatives?
Surgery
All surgeries were performed by two experienced refractive surgeons (AKD and JR) under topical anesthesia. Treatments were programmed to ensure complete coverage of the scotopic pupil, and Preop aberrometric measurements obtained with the high-resolution aberrometer iDesign were considered for the calculation of the ablation profile that was uploaded to the STAR S4 IR Excimer Laser System. Corneal flaps were created using the iFS Femtosecond Laser, programming flaps with a diameter of 8.9 mm and a depth of 110 μm. After the creation of the flap, the laser beam was focused on the cornea using the reticule of the microscope and then the programmed treatment was applied. Standard topical Postop treatment consisting of a combination of dexamethasone and gentamicin eye drops four times a day for 5–7 days was administered to all patients. Also, patients were instructed to use an artificial tear solution at least every 2 hours on the day of surgery and at least four times a day during 1 month.
Statistical analysis
SPSS statistics software package Version 19.0 for Windows (IBM Corporation, Armonk, NY, USA) was used for statistical analysis. The normality of data samples was evaluated by means of the Kolmogorov–Smirnov test. When parametric analysis was possible, the Student’s t-test for paired data was used for comparisons between the Preop and Postop data, whereas the Wilcoxon rank sum test was applied to assess the significance of such differences when parametric analysis was not possible. For all statistical tests, a P-value <0.05 was considered as statistically significant.
Results
The sample included a total of 253 eyes, with a mean Preop manifest SE value of −4.41±1.94 D (range −0.75 D to −9.50 D) and a mean cylinder value of −0.85±0.72 D (range −4.75–0.00 D). The mean age of patients included in the study was 33.7±9.4 years (range 19–54 years).
Visual and refractive outcomes
The visualization of the data concerning efficacy, predictability, and safety was based on the publication of Dupps et al.18 Figure 1A summarizes the distribution of Postop UDVA at 2 months after surgery in the sample of eyes evaluated. As shown, the percentage of eyes that achieved 20/16, 20/20, and 20/25 or better UDVA at 2 months after surgery was 85% (215/253), 99% (250/253), and 100%, respectively (efficacy index 1.15; Figure 1A). Regarding refraction, the 2-month Postop manifest SE and cylinder values were within ±0.25 D in 97% (245/253) of eyes (Figure 1). All eyes had a 2-month Postop SE and cylinder values within ±0.5 D (Figure 1D and E). Concerning safety, all eyes maintained CDVA or gained one LogMAR line (safety Index 1.15; Figure 1B). The reduction of the SE value achieved after surgery was statistically significant (Preop: −4.43±1.88 D vs −0.03±0.12 D, P<0.001). Figure 1C shows the achieved SE correction at the end of the follow-up plotted against the intended. A strong and statistically significant correlation was found among the achieved and the intended correction (r=0.998, P<0.01). Figure 1E shows that Postop results stayed stable over 2 months.
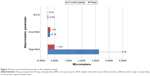
Aberrometric outcomes
Figure 2 summarizes the corneal aberrometric outcomes obtained in the analyzed sample. As shown, a statistically significant reduction was found in the total root mean square (RMS) value (P<0.001). A significant reduction was also observed in the Zernike term corresponding to the primary spherical aberration (P=0.001). In contrast, a small but statistically significant change was observed in the RMS value corresponding to higher aberrations (P<0.001).
Patient satisfaction and photic phenomena
A total of 80 patients finally answered the subjective questionnaire evaluating subjectively the patient vision and the incidence of photic phenomena. Table 1 shows the Preop and 2-month Postop results obtained with this subjective questionnaire. In general terms, Postop difficulties related to vision were graded as minimal, with low levels of photic phenomena (Table 1). Furthermore, there was a significant decrease in the level of vision-related difficulty to perform daily activities as well as a significant decrease in the level of glare perceived by patient while driving car (P<0.001) with surgery (Table 1).
Besides all these questions about Preop and Postop patient vision and photic phenomena perception, the patients were asked postoperatively about their satisfaction with the surgery outcome. The following mean scores (scale from 0 to 9; 0= completely false, 9= completely true) were obtained: 8.59 (SD 0.84; median 9.00, range 5–9) for “Is visual performance better compared to your expectations?”, 8.47 (SD 1.76; median 9.00, range 0–9) for “Would you do the same surgery again?”, 8.71 (SD 0.58; median 9.00, range 7–9) for “How satisfied are you with your vision?”, 8.80 (SD 0.59; median 9.00, range 6–9) for “Did your quality of life improve after surgery?”, and 8.74 (SD 0.69; median 9.00, range 6–9) for “Would you recommend the surgery to friends and relatives?”.
Discussion
This study evaluated the performance in terms of visual, refractive, and aberrometric outcomes of myopic WFG LASIK using a high-resolution wavefront sensor. The efficacy of the surgery was good in the sample evaluated, with 20/20 UDVA achieved in almost all cases (99% [250/253]) and visual acuity beyond 20/20 reported in a high percentage of cases (84% [213/253]). This is consistent or even better than the results of previous series evaluating the visual performance after myopic LASIK surgery with different laser platforms using WFG profiles.2,3,7–15 Tanzer et al10 found a percentage of 98% of eyes achieving 20/20 UDVA in a group of naval aviators undergoing myopic LASIK with the VISX STAR S4 IR. In a study conducted recently by Schallhorn et al,2 a total of 93.4% of eyes undergoing WFG LASIK for the correction of myopia with the same excimer laser platform (VISX STAR S4 IR laser + iDesign aberrometer) used in our study achieved 20/20 UDVA postoperatively. Percentages of eyes with 20/20 UDVA after WFG LASIK ranging from 80% to 95% have been reported for other excimer laser platforms.3,12,15,17 Likewise, our results are better than those obtained with the same excimer laser used in our study using an aberrometer of lower resolution (WaveScan; AMO, Abbott Medical Optics Inc.) for the characterization of ocular aberrations.9,14 It should be considered that the WaveScan system is a Hartmann–Shack aberrometer that captures an average of 240 data points for a 7.0-mm pupil, whereas the iDesign aberrometer is an improved version of this system, allowing the analysis of 1,257 data points for a 7.0-mm pupil. Indeed, significant differences in the measurements of refraction and ocular aberrations obtained with these two aberrometers have been previously reported.5
Regarding refraction, an excellent level of predictability of the refractive correction was achieved, with 97% (245/253) of eyes with a 2-month Postop manifest SE value within ±0.25 D of emmetropia and a manifest cylinder value of 0.00 D or 0.25 D. All eyes showed a Postop SE value within ±0.50 D of emmetropia. This excellent level of predictability is similar to that obtained with the same laser technology and better than those obtained with WFG LASIK based on measurements obtained with other types of aberrometers.2,3,7,9,12,15,17 Specifically, 83.9%, 88.0%, and 86.5% of eyes within ±0.50 D have been reported by Wu et al,3 Taneri et al,12 and Ryan and O’Keeffe15 after WFG LASIK using other laser platforms. This suggests that the resolution of the aberrometer used for planning the WFG ablation profiles in our study has a crucial role in the achievement of a better level of predictability of the refractive correction. Indeed, there is some scientific evidence showing the high control of HOAs and excellent refractive predictability achieved with WFG LASIK treatments performed using the excimer laser and the high-resolution Hartmann–Shack aberrometer used in the current study.2,7 The control of potential torsional misalignments of the laser platform evaluated has been already shown to increase significantly the predictability of refractive correction achieved with LASIK as well as to reduce the induction of HOAs.19,20 In our series, a significant reduction in the total RMS value and the level of spherical aberration was observed. Therefore, myopic LASIK treatments with the laser platform evaluated avoid the induction of spherical aberration and even reduce this aberration in some cases. Other authors have reported no spherical aberration change or minimal increase after WFG LASIK for the correction of a similar range of myopic refractive errors.1,10,12,14 Khalifa et al found in a sample of myopic eyes with SE values ranging from −6.63 D to 0.00 D that the mean change in spherical aberration after WFG LASIK using the STAR S4 IR Excimer Laser System combined with the WaveScan aberrometer was 0.18 μm (6-mm pupil).14 Mean changes of +0.05 μm and +0.01 μm were reported by Tanzer et al10 and Jabbur et al21 at 3 months and 6 months, respectively, both also using the WaveScan aberrometer.10,21 The RMS value corresponding to HOAs experienced a statistically significant increase but of very small magnitude (0.02 μm) and was not clinically relevant considering the variability of this parameter in the normal healthy population.22 This confirms the ability of the treatment applied for maintaining the level of HOAs within a physiological range.22
Besides the visual, refractive, and corneal aberrometric outcomes, patient satisfaction and incidence of photic phenomena were also evaluated. For such a purpose, a self-developed questionnaire was designed according to the most common complaints and disturbances referred by patients after LASIK in our clinical practice. The patients were asked to grade different difficulties related to vision and visual disturbances using a numerical scale ranging from 0 to 9, 9 being the worst situation. A significant improvement was found in the level of difficulty related to vision to perform daily activities as well as in the level of glare perceived by patients while driving car. The reduction in vision-related difficulty to perform daily activities seems to be related to the predictable refractive correction and the corneal aberrometric control achieved with the surgery, providing complete spectacle independence. The potential contribution of the significant improvement in the self-perceived uncorrected vision that is referred in some occasions by patients after LASIK should also be considered.23 Regarding the reduction in the glare perceived while driving car, it may be attributable to the effective control of corneal HOAs, leading to the preservation of the optical performance of the eye. Yu et al17 demonstrated in a comparative study evaluating patient satisfaction and visual symptoms after WFG and WF-optimized LASIK that the rate of visual symptoms such as glare, halo, and night driving difficulty decreased postoperatively after both treatment protocols. Future studies should be performed to evaluate the correlation between changes in different types of HOAs and visual performance after WFG LASIK and the reduction in the incidence of photic phenomena with the excimer laser technology evaluated. Regarding patient satisfaction, it was maximal for most of the patients (close to 9 that represented the best score), as in previous studies.17,24 Yu et al found that 95% of patients in a sample of myopes undergoing WFG-LASIK were satisfied with the surgery and would recommend the procedure to a friend or family member.17 Awwad et al24 found a significant improvement in the quality of life after WFG-LASIK for the correction of myopic refractive errors between −1.00 D and −7.50 D, with the main changes pertaining to psychological well-being and social role, more than the changes in visual function.
Conclusion
WFG LASIK using the excimer laser technology evaluated combined with the high-resolution aberrometer is predictable and efficacious for the correction of myopia or myopic astigmatism. The high-level refractive correction and ocular optics lead to high levels of patient satisfaction and minimal incidence of Postop photic phenomena. Further studies about the correlation of the visual, refractive, and aberrometric benefits of WFG treatments with the level of patient satisfaction and photic phenomena perception with a longer follow-up should be performed.
Acknowledgments
The authors have no proprietary or commercial interest in the medical devices that are involved in this manuscript. This research was funded with an unrestricted educational grant from Abbott Medical Optics Inc.
Disclosure
The authors report no conflicts of interest in this work.
References
Zhang J, Zhou YH, Li R, Tian L. Visual performance after conventional LASIK and wavefront-guided LASIK with iris-registration: results at 1 year. Int J Ophthalmol. 2013;6(4):498–504. | ||
Schallhorn S, Brown M, Venter J, Teenan D, Hettinger K, Yamamoto H. Early clinical outcomes of wavefront-guided myopic LASIK treatments using a new-generation Hartmann-Shack aberrometer. J Refract Surg. 2014;30(1):14–21. | ||
Wu J, Zhong X, Yang B, Wang Z, Yu K. Combined wavefront-guided laser in situ keratomileusis and aspheric ablation profile with iris registration to correct myopia. J Cataract Refract Surg. 2013;39(7):1059–1065. | ||
López-Miguel A, Maldonado MJ, Belzunce A, Barrio-Barrio J, Coco-Martín B, Nieto JC. Precision of a commercial Hartmann-Shack aberrometer: limits of total wavefront laser vision correction. Am J Ophthalmol. 2012;154(5):799–807. | ||
Jung JW, Chung BH, Han SH, Kim EK, Seo KY, Kim TI. Comparison of measurements and clinical outcomes after wavefront-guided LASEK between iDesign and WaveScan. J Refract Surg. 2015;31(6):398–405. | ||
Shaheen MS, El-Kateb M, Hafez TA, Piñero DP, Khalifa MA. Wavefront-guided laser treatment using a high-resolution aberrometer to measure irregular corneas: a pilot study. J Refract Surg. 2015;31(6):411–418. | ||
Smadja D, De Castro T, Tellouck L, et al. Wavefront analysis after wavefront-guided myopic LASIK using a new generation aberrometer. J Refract Surg. 2014;30(9):610–615. | ||
Yu CQ, Manche EE. Comparison of 2 wavefront-guided excimer lasers for myopic laser in situ keratomileusis: one-year results. J Cataract Refract Surg. 2014;40(3):412–422. | ||
Shaheen MS, Massoud TH, Ezzeldin H, Khalifa MA. Four-year visual, refractive, and contrast sensitivity outcomes after wavefront-guided myopic LASIK using an advanced excimer laser platform. J Refract Surg. 2013;29(12):816–822. | ||
Tanzer DJ, Brunstetter T, Zeber R, et al. Laser in situ keratomileusis in United States Naval aviators. J Cataract Refract Surg. 2013;39(7):1047–1058. | ||
Lee K, Ahn JM, Kim EK, Kim TI. Comparison of optical quality parameters and ocular aberrations after wavefront-guided laser in-situ keratomileusis versus wavefront-guided laser epithelial keratomileusis for myopia. Graefes Arch Clin Exp Ophthalmol. 2013;251(9):2163–2169. | ||
Taneri S, Oehler S, MacRae SM. Aspheric wavefront-guided versus wavefront-guided LASIK for myopic astigmatism with the Technolas 217z100 excimer laser. Graefes Arch Clin Exp Ophthalmol. 2013;251(2):609–616. | ||
Sáles CS, Manche EE. One-year outcomes from a prospective, randomized, eye-to eye comparison of wavefront-guided and wavefront-optimized LASIK in myopes. Ophthalmology. 2013;120(12):2396–2402. | ||
Khalifa MA, Allam WA, Shaheen MS. Visual outcome after correcting the refractive error of large pupil patients with wavefront-guided ablation. Clin Ophthalmol. 2012;6:2001–2011. | ||
Ryan A, O’Keefe M. Wavefront-guided and aspheric ablation for myopia – one-year results of the Zyoptix personalized treatment advanced algorithm. Am J Ophthalmol. 2012;153(6):1169–1177. | ||
He L, Manche EE. Prospective randomized contralateral eye evaluation of subjective quality of vision after wavefront-guided or wavefront-optimized photorefractive keratectomy. J Refract Surg. 2014;30(1):6–12. | ||
Yu J, Chen H, Wang F. Patient satisfaction and visual symptoms after wavefront-guided and wavefront-optimized LASIK with the WaveLight platform. J Refract Surg. 2008;24(5):477–486. | ||
Dupps WJ Jr, Kohnen T, Mamalis N, et al. Standardized graphs and terms for refractive surgery results. J Cataract Refract Surg. 2011;37:1–3. | ||
Khalifa M, El-Kateb M, Shaheen MS. Iris registration in wavefront-guided LASIK to correct mixed astigmatism. J Cataract Refract Surg. 2009;35(3):433–437. | ||
Venter J. Outcomes of myopic LASIK with and without NIDEK active torsion error correction. J Refract Surg. 2009;25(11):985–990. | ||
Jabbur NS, Kraff C, Visx Wavefront Study Group. Wavefront-guided laser in situ keratomileusis using the WaveScan system for correction of low to moderate myopia with astigmatism: 6-month results in 277 eyes. J Cataract Refract Surg. 2005;31(8):1493–1501. | ||
Wang L, Koch DD. Ocular higher-order aberrations in individuals screened for refractive surgery. J Cataract Refract Surg. 2003;29(10):1896–1903. | ||
Tahzib NG, Bootsma SJ, Eggink FA, Nabar VA, Nuijts RM. Functional outcomes and patient satisfaction after laser in situ keratomileusis for correction of myopia. J Cataract Refract Surg. 2005;31(10): 1943–1951. | ||
Awwad ST, Alvarez-Chedzoy N, Bowman RW, Cavanagh HD, McCulley JP. Quality of life changes after myopic wavefront-guided laser in situ keratomileusis. Eye Contact Lens. 2009;35(3):128–132. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.