Back to Journals » Clinical Ophthalmology » Volume 17
Vision-Related Quality of Life and Associated Factors Among an Adult Population with Glaucoma Attending a Comprehensive Specialized Hospital, Northwest Ethiopia
Authors Guchi GS , Mersha GA, Alimaw YA, Assem AS , Fekadu SA
Received 17 November 2022
Accepted for publication 12 January 2023
Published 18 January 2023 Volume 2023:17 Pages 225—237
DOI https://doi.org/10.2147/OPTH.S397775
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Girma Shallo Guchi,1 Getasew Alemu Mersha,2 Yezinash Addis Alimaw,2 Abel Sinshaw Assem,2 Sofonias Addis Fekadu2
1Department of Ophthalmology, Madda Walabu University Goba Referral Hospital, Goba City, Ethiopia; 2Department of Optometry, University of Gondar Comprehensive Specialized Hospital, Gondar City, Ethiopia
Correspondence: Getasew Alemu Mersha, Tel +251 932823935, Fax +251-058-114 1240, Email [email protected]; [email protected]
Background: Glaucoma is a group of ocular conditions that leads to irreversible blindness. It can affect the vision-related quality of life in many ways. In Ethiopia, limited information is available on how and to what extent the vision-related quality of life of the glaucoma population has been affected.
Objective: This study attempted to assess the vision-related quality of life and associated factors among an adult population with glaucoma attending Felege Hiwot Comprehensive Specialized Hospital, Northwest Ethiopia.
Methods: The cross-sectional study was conducted on the adult population with glaucoma attending Felege Hiwot Comprehensive Specialized Hospital. Systematic random sampling was employed to select 319 study participants. Descriptive and summary statistics were calculated. Simple and multiple linear regressions were performed to determine factors associated with vision-related quality of life. A p-value of < 0.05 in multivariable regression was considered statistically significant at a 95% confidence level.
Results: The mean glaucoma quality of life-15 score in this study was 47.85 ± 15.41. Below primary education, primary education, visual acuity of the better eye, visual acuity of the worse eye, and severe glaucoma were significantly associated with the glaucoma quality of life-15 score.
Conclusion and Recommendation: The study observed poorer vision-related quality of life in the glaucoma population than previously reported in Ethiopia and around the globe. The vision-related quality of life was significantly associated with educational status, visual acuity of the better and worse eye, and stage of glaucoma in the better eye. Educating the glaucoma population on the nature of the disease, advice on early presentation, and better-coping strategies for the condition are warranted.
Keywords: vision, quality of life, glaucoma, Ethiopia
Introduction
Glaucoma is a group of eye diseases signified by permanent optic nerve damage associated with progressive visual field loss.1 It is one of the leading causes of irreversible blindness in adults aged 50 years and above worldwide.2,3
Globally, 64.3 million (3.54%) people aged 40–80 were affected by glaucoma in 2013, with Asia and Africa accounting for 60% and 13% of the world’s total glaucoma cases, respectively. The global magnitude is estimated to rise to about 111.8 million in 2040, disproportionally affecting people living in Asia and Africa.4–6
In a recent epidemiological study conducted in Ethiopia on voluntary people coming for a glaucoma screening program at Jimma University alone, 10.24% were diagnosed to have glaucoma.7 The increasing magnitude of the problem, along with other chronic aging eye diseases and an increasing number of aged population in the world today, is posing a significant healthcare burden.2,8
Quality of Life (QOL): an important measure of the physical, emotional, and social well-being of a person,9 is a highly subjective broad-ranging concept as it can refer both to the experience an individual has of his or her own life and to the living conditions in which individuals find themselves.10 So, it is influenced in a complex way by the person’s physical health, level of independence, social relationships, personal beliefs, and psychological state.
Vision-related quality of life is related to visual function and represents the extent to which vision affects activities of daily living (ADL) and the social, emotional, and economic well-being of an individual.11 Glaucoma affects the population’ Vision-related quality of life (VRQOL) in several ways: reduced peripheral Visual Field (VF) and visual acuity (VA), inconvenience of daily applications of eye drops, potential side effects of treatments, increment of psychological and economic burden.12–14
In the advanced stages of the disease, patients may also experience difficulty in recognizing faces, navigation, reading activities, watching television, noticing objects in their peripheral visual area, and adapting to different levels of light. Moreover, glaucoma is an independent risk factor for falling accidents. The adverse impacts of advanced glaucoma lead to increased healthcare expenditures and decreased VRQOL, and overall QOL as well.13,15
The clinicians often focus on the objective signs of disease severity such as intraocular pressure level and optic nerve appearance, whereas what is of interest to patients is the extent to which these factors influence functional status, emotional well-being, and eventually their health-related quality of life.16 Only a few clinicians discuss the specific glaucoma quality of life with their patients.17 However, it is crucial to consider the patient’s subjective interpretation of the disease and the way it affects them outside the clinic. Patient’s perception of the disease and its treatment can also play a huge role in enhancing QOL.18 Thus, maintaining the QOL of glaucoma patients should be considered one of the most important goals for glaucoma treatment and follow-up.
Despite the globally increasing magnitude of the disease along with its impacts on the QOL of patients, sufficient information is not available in different parts of our country regarding how and to what extent the QOL of the glaucoma population is affected. So, this study aimed to assess VRQOL and associated factors among an adult population with glaucoma attending Felege Hiwot Comprehensive Specialized Hospital, Northwest Ethiopia.
Methods and Materials
Study Design and Period
A cross-sectional study was applied to the glaucoma population. Participants were recruited in the study via a systematic random sampling scheme from June 18 to August 20/2021.
Source and Study Population
Felege Hiwot Specialized Hospital, with its integrated ophthalmology unit, is one of the few eye care centers situated in Northwest Ethiopia. The center has been providing comprehensive eye care services for millions of people in the city of Bahir Dar and the surrounding. Based on data obtained from the glaucoma follow-up registration book, there were around 360 glaucoma patients attending at ophthalmology unit during the preceding month. Ophthalmologists, optometrists, and ophthalmic nurses are involved in the diagnosis, management, and follow-up of patients with glaucoma in the center. The target populations of the study are adult patients previously diagnosed with glaucoma with a minimum of six months duration, attending the Felege Specialized Hospital Ophthalmology Unit.
Exclusion Criteria
- Glaucoma population who had mobility, cognitive, and hearing problems.
- Glaucoma population who had a history of incisional eye surgery in the last 3 months.
- Glaucoma population who were visually significant cataracts (greater than stage 2 LOCS III Classification).
- Glaucoma population who were high refractive errors >5 Diopter.
- Glaucoma population who were having age-related macular degeneration and other retinal diseases which may affect the vision-related quality of life.
Sample Size Calculation
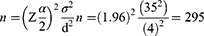
The sample size for the outcome variable was determined by using the single population mean formula, considering the following assumptions: Level of significance (α) = 5% (with a confidence level of 95%), Marginal error (d) = 4% Mean Glaucoma Quality of Life taken from a similar study= 46.3 (±35)13 and Z-value of 1.96 was used at 95% CI while n= Sample size.
After adjusting for a 10% for non-response rate and incomplete patient chart the total maximum sample size was determined to be 325. A sampling interval of 2 was decided by dividing the number of glaucoma population over two months (720) to the final calculated sample size of 321 (Figure 1).
 |
Figure 1 A flow chart showing the potential participants and sampling. |
Ethical Considerations
The study adhered to the tenets of the Declaration of Helsinki and approval was sought and obtained from the Ethical Review Board of the College of Medicine and Health Sciences, University of Gondar under Institutional Review Board Number 641/6/21. Written informed consent was obtained from all voluntary participants. The participants were informed of the study would not inflict any harm on them. Neither the data collectors nor the authors were allowed to access the personal identifiers of participants. The confidentiality of the study participants was maintained at all stages of data collection and processing.
Operational Definitions
- Vision-Related Quality of Life: a QOL related to visual function measured by a mean score of the GQL-15 questionnaire.19
- Mild Glaucoma: Early glaucomatous disc features (Vertical CD ratio<0.65).20
- Moderate Glaucoma: Moderate glaucomatous disc features (Vertical CD ratio 0.7–0.85).20
- Advanced or Severe Glaucoma: Advanced glaucomatous disc features (Vertical CD ratio>0.9).20
- Distance vision impairment21
- Mild visual impairment: VA worse than 6/12 to 6/18.
- Moderate visual impairment: VA worse than 6/18 to 6/60.
- Severe visual impairment: VA worse than 6/60 to 3/60.
- Blind: VA worse than 3/60.
Data Collection Procedures and Quality Control
Data were collected using a checklist of clinical examinations, and a pretested, structured questionnaire. The questionnaire consists of the following parts; part I: which contains questions on socio-demographic characteristics, part II: GQL-15 questionnaire19 to assess VRQOL, and part II: which contains a checklist of clinical variables.
The GQL-15 has 15 questions with each question having five answers represented by values ranging from 0 to 5 (0 = Abstinence from activity owing to non-visual reasons, 1 = No difficulty, 2 = A little bit of difficulty, 3 = Some difficulty, 4 = Quite a lot of difficult, 5 = Severe difficulty). This tool has four subscales which include: Central and Near Vision (Reading newspapers, sewing, handcrafting, and Recognizing faces), Peripheral vision (Walking on uneven roads, Tripping over objects, Seeing objects coming from the side, Walking on steps stairs, Bumping into objects and Judging distance of foot to step/surb), Glare and dark adaptation (Walking after dark, Seeing at night, Adjusting to bright lights, Adjusting to dim lights, Going from the dark room and vice versa and Finding dropped objects) and Outdoor mobility (Crossing the road).
The data were collected by three trained optometrists under the supervision of one ophthalmic officer. Eligible participants with glaucoma were approached by the optometrists, after completing their follow-up evaluations and treatment at the glaucoma clinic. The local language (Amharic) translated structured questionnaire was administered through the face-to-face interview by the data collectors. All other required clinical variables were retrieved from patients’ medical folders using a data collection checklist.
Before the actual data collection, the questionnaire was translated and pretested on five percent of the sample size (16 glaucoma patients) at Gondar Tertiary Eye Care Center, Northwest Ethiopia. Necessary modifications and adjustments were made to the final questionnaire accordingly. Internal consistency was assessed using Cronbach’s α value (0.94). Training and supervision of the data collectors were done to ensure the quality of the data. Finally, the completeness and consistency of collected data were checked by the supervisor and the principal investigator (PI).
Data Processing and Statistical Analyses
The data were entered into EpiData version 4.6.0.4 software and exported to and analyzed using IBM Statistical Package for the Social Sciences (SPSS) version 26. The descriptive statistics were summarized and presented with frequency, percentage, median, mean, standard deviation, and range. A continuous score for GQL-15 questions was taken as a primary outcome of the study. Multiple linear regressions were performed to determine factors associated with quality of life in the glaucoma population. All tests were two-sided, and variables with a p-value <0.05 in multivariable linear regression were considered statistically significant at a 95% confidence level.
The response of study participants to the GQL-15 questionnaire ranges from 15 to 75, and the mean of the responses was calculated to determine the quality of life among participants, with higher numbers denoting poorer and lower numbers the better quality of life.
The assumptions of Linear Regression were checked for a linear relationship, multicollinearity, normal distribution of the residuals, homoscedasticity, and outliers. Variables were assessed for normality using the Kolmogorov–Smirnov test. For normally distributed variables, the mean and standard deviation were presented.
Variables including residence, educational status, VA of the better and worse eyes, stages of glaucoma for better and worse eyes, and Visual Impairment were correlated with the quality of life in bivariable linear regression. In multivariable linear regression, Visual Impairment (VI) and VA of the better eye were strongly correlated in multicollinearity checks. Then the variable that did not explain the outcome variable (VI) was excluded. Finally, the variables which include residence, educational status, VA, and stage of glaucoma for the better and worse eyes were properly fitted into the model.
Results
Socio-Demographic Characteristics of the Study Participants
A total of 319 glaucoma population participated in this study with a response rate of 98.15%. The median age of the participants was 60 years, with a range from 18 to 87 years and 241 (75.5%) were male. More than half of the respondents, 165 (51.7%), were rural residents, and 174 (54.5%) were farmers. The majority of the respondents, 207 (64.9%) were below primary education and about 148 (71.5%) of these were rural residents. More than three-fourths, 246 (77.1%) of the participants were married, and 295 (92.5%) were orthodox Christian religion followers (Table 1).
 |
Table 1 Socio-Demographic Characteristics of the Study Participants |
Clinical Characteristics of the Study Participants
More than half, 191 (59.9%) of the study participants had visual impairment of which 107 (33.5%) were having moderate visual impairment. Blindness was reported among 20 (6.3%) participants. Nearly all of the participants, 290 (90.9%), of the participants had a bilateral diagnosis of glaucoma. About 287 (90.0%) participants had open-angle glaucoma; the rest had angle closure and pseudo-exfoliative glaucoma. Nearly half, 155 (48.6%), of the study participants, were in the severe stage of the condition. All participants were on topical anti-glaucoma medications, and 34 (10.7%) of them had additional systemic anti-glaucoma drugs. The majority of the glaucoma population, 237 (74.3%) had 2 or more anti-glaucoma medications (Table 2).
 |
Table 2 Clinical Findings of the Study Participants with Glaucoma |
Vision-Related Quality of Life of Participants
Multiple linear regression analyses indicated that socio-demographic variables explained relatively a small proportion (23.7%) of the variance in the GQL-15 summary scores than clinical factors (48.7%). The socio-demographic and clinical variables together explained the variance in the GQL-15 score of 50.8%.
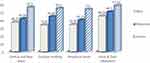
The mean summary score of GQL in the present study was 47.85 (95% CI; 46.11–49.62). The score was 42.51 among urban and 52.84 for rural residents. Among all domains of GQL-15, the highest score was reported for the dimension of glare and dark adaptation (51.95± 15.38), followed by central and near vision (46.76 ±18.63) and outdoor mobility (45.61 ± 22.17), and the lowest scores were for the peripheral vision (44.31 ±18.13) (Table 3).
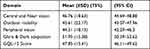 |
Table 3 Distribution of the Four Subscales of the GQL-15 Scores in Glaucoma Patients |
The three most affected ADLs reported for all participants in this study were adjusting to bright lights (3.78 ± 1.4), going from the dark room and vice versa (3.7 ± 1.2), and adjusting to dim lights (3.63 ± 1.3). Bumping into objects (2.53 ± 1.5) was the least affected GQL-15 item.
Factors Associated with Vision Related Quality of Life
Among the variables fitted into the multiple linear regression models: educational status (Below Primary, and Primary Education), VA of the worse and better eye, and severe stage of glaucoma in the better eye showed a statistically significant association with VRQOL of glaucoma patients at 95% confidence level.
Compared to the participants with the educational level of college and above, participants who were below primary education level were associated with a 5.42 reduction in the quality of life, and those participants who had an educational level of primary education had a 5.9 less GQL score, keeping all other variables constant. In addition, a unit increase in Snellen’s decimal equivalent of VA of the better and worse eyes improves the glaucoma-related quality of life by 14.80 and 14.92 times, respectively, holding other variables constant.
Additionally, participants with a severe form of glaucoma had an 8.02 less quality of life score as compared to those with early stage, while other variables are kept constant (Table 4).
 |
Table 4 Multivariable Analysis of Variables with Vision-Related Quality of Life Among the Study Participants |
Correlations of Factors with Vision-Related Quality of Life of Participants
A point bi-serial correlation was run to determine the relationship between predictors and each domain of GQL-15. Educational status of those below primary education and those in secondary education were significantly correlated with all subscales of GQL-15. (Figure 2) Visual acuity of the better and worse eyes, and the severe stage of both the better and worse eyes were also significantly correlated with the entire subscales of GQL-15. Furthermore, the moderate stage of glaucoma on the better eye was significantly correlated with the Central and Near Vision and the Peripheral Vision subscales, whereas the moderate glaucoma of the worse eye was significantly correlated with all except the Glare and Dark Adaptation subscale (Table 5).
 |
Table 5 Comparison of Linear Correlations of GQL-15 Subscales Scores with the Predictive Variables |
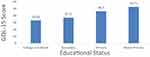 |
Figure 2 Comparison of GQL-15 Summary Scores by Educational Status among glaucoma patients attending Felege-Hiwot Comprehensive Specialized Hospital, Northwest Ethiopia, 2021. |
Distribution of GQL-15 Scores by Visual Impairment
The following diagram shows an increase in the mean GQL-15 scores as VA decreases (as the severity of VI increases) from the normal to the blindness stage (Figure 3).
 |
Figure 3 Comparison of GQL-15 summary scores by visual impairment status among glaucoma patients attending Felege-Hiwot Comprehensive Specialized Hospital, Northwest Ethiopia, 2021. |
Vision-Related Quality of Life of Participants by Stage of Glaucoma
The GQL-15 mean scores and all four subscale scores showed a uniform rise in their value from mild to severe stages of the disease, indicating that all four visual parameters are affected in glaucoma, and worsen with an increase in the disease severity (Figure 4).
Discussion
Glaucoma is a chronic, progressive group of eye disorders that requires long-term treatment and frequent follow-ups. The patients are at increased risk of various complications secondary to treatments and the disease itself contributing to poor VRQOL.22 Thus, the present study evaluated the Vision-Related Quality of Life of patients with glaucoma at Felege Hiwot Tertiary Hospital, Northwest Ethiopia.
The mean VRQOL score among patients with glaucoma in the current study using GQL-15 was 47.85 (95% CI, 46.11–49.62). The finding was consistent with that of previously conducted in Gondar, Ethiopia,13 46.3. However, the finding was higher denoting poorer VRQOL, compared to the findings of the previous studies conducted in Nigeria, 24.07,23 India, 26.0,24 China; 26.0,25 28.79,14 and 31.86,22 Australia, 30.5,26 England, 22.0919 and the Netherlands, 28.27 These discrepancies may be explained by various factors including variation in the socio-economic and clinical characteristics of the study participants, sampling methods, and inclusion and exclusion criteria used by the studies.
For instance, studies conducted in Nigeria,23 China,25 and the Netherlands27 were merely involving participants having ocular hypertension and primary open-angle glaucoma as a case. Similarly, glaucoma in England19 was determined based on visual field loss with normal visual acuity. These would limit the number of advanced glaucoma and in turn, contribute to a lower mean score of VRQOL against the present study. Besides, twenty-five percent of the participants in the current study were aged above 67 years compared to the previous studies.14,19 This might have also contributed to the poorer VRQOL in the current study, as the quality of life gets low in the older age groups.13
Additionally, the late presentation of patients in Sub-Saharan Africa particularly the present study area, with advanced stage of the disease can cause significant peripheral and central visual impairment.28 These impairments potentially challenge the performance of ADL, moving around, finding objects, and adapting to changing lighting conditions, contributing to a higher GQL-15 score reported in the current study.
Thus, creating awareness among the society by giving health education about the overall eye exams, and particularly, glaucoma, for screening and early detection of glaucoma, prevent the late presentation of patients at an advanced stage of the condition.
The mean scores of the four GQL-15 subscales, namely, “Central and Near vision”, “Outdoor mobility”, “Peripheral vision” and “Glare and Dark adaptation” were 46.76, 45.61, 44.31 and 51.95 respectively, indicating that, greater difficulties were noted in the glare and dark adaptation domain. This pattern was supported by previous reports of studies conducted in Ethiopia,13 Nigeria,23 India,24 China,14,22 and Australia.26 The possible justification for such a pattern might be because glare sensitivity is one of the biggest side effects of glaucoma-related fear of light resulting from the intra-ocular pressure rise in the eye.
The glare sensitivity which gets worse under sunlight and artificial light exposure makes a challenging performance of ADL such as driving at night and outdoor activities. The high proportion of participants with advanced glaucoma in the present study could also reflect the pattern, as patients with advanced or severe glaucoma have more difficulty with glare than with mild or moderate glaucoma.29
Additionally, in the present study, participants with primary education and below were significantly associated with higher mean GQL-15 scores. Conversely, the association signified those participants with low educational status showed poorer VRQOL compared with high educational status.
A similar finding was revealed by studies in China14,30 and Greek.31 The association could be explained in a way that, participants with lower educational status might not have adequate information on the nature of the disease.32–34 Thus, they could not adopt a good practice pattern35 (better coping mechanism) and this ultimately compromises their vision-related quality of life.
In addition, a unit increase in Snellen’s decimal equivalent of VA of the better and worse eyes improves the vision-related quality of life by 14.8 and 14.9 in the present study respectively. This trend was supported by previous studies in Ethiopia,13 China,14,30 Australia,26 Slovakia,36 and Brazil.37 This could be because visual acuity is a major factor controlling the activities of daily living which were included in the four domains of glaucoma-related quality of life, which enhances the overall vision-related quality of life.
Moreover, the severe stage of glaucoma was significantly associated with a reduction of VRQOL in the current study, consistent with other previous studies done in Ethiopia,13 India,24 China,14 Australia,12,26 and Brazil.37 In the advanced stage of glaucoma, all the visual functions including mobility-related components of quality of life will be significantly affected which would, in turn, affects the whole vision-related quality of life.38,39 Severe visual field loss in advanced glaucoma can affect driving activities, the psychological condition, and peripheral and central vision which ultimately reduce the overall VRQOL.40,41
Limitation
Due to the cross-sectional nature of the study, the association between Vision-Related Quality of Life and the predictive variables may not be causal. Unlike some other studies which have used visual field assessment for staging, we used a vertical CD ratio-based staging in this study, because we had no visual field testing service in the study area, and this may lead to inconsistency of results and make difficult comparisons with the findings of the previous studies.
Conclusion
The study observed poorer vision-related quality of life in a glaucoma population attending Felege Hiwot Referral Hospital Northwest Ethiopia than previously reported in Ethiopia and around the globe. The vision-related quality of life was significantly associated with educational status, visual acuity of the better and worse eye, and stage of glaucoma in the better eye.
The poorer quality of life in the study area reflects the need to consider educating the glaucoma population on the nature of the disease and advise them on the better-coping strategy of glaucoma in the overall care and management of the condition. Further study with a prospective longitudinal cohort design for a better assessment of the quality of life in glaucoma is warranted.
Abbreviations
ADL, Activity of Daily Living; CD, Cup to Disc; CI, Confidence Interval; GQL, General Quality of Life; LOCS III, Lens Opacity Classification System; QOL, Quality of Life; VA, Visual Acuity; VRQOL, Vision Related Quality of Life.
Acknowledgment
Our deepest gratitude goes to all staff of Felege Hiwot Comprehensive Specialized Hospital Ophthalmology Department for their cooperation and engagement throughout the data collection period. We would also like to extend our gratitude to our patients who willingly participated in the study.
Funding
The study did not receive funding from any organization.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Riva I, Legramandi L, Rulli E, et al. Vision-related quality of life and symptom perception change over time in newly-diagnosed primary open angle glaucoma patients. Sci Rep. 2019;9(1):6735. doi:10.1038/s41598-019-43203-9
2. Steinmetz JD, Bourne RRA, Briant PS, et al. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the right to sight: an analysis for the global burden of disease study. Lancet Glob Health. 2021;9(2):144–160. doi:10.1016/S2214-109X(20)30489-7
3. Flaxman SR, Bourne RRA, Resnikoff S, et al. Global causes of blindness and distance vision impairment 1990–2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(12):1221–1234. doi:10.1016/S2214-109X(17)30393-5
4. Allison K, Patel D, Alabi O. Epidemiology of glaucoma: the past, present, and predictions for the future. Cureus. 2020;12(11):11686.
5. Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081–2090. doi:10.1016/j.ophtha.2014.05.013
6. Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262–267. doi:10.1136/bjo.2005.081224
7. Daba KT, Gessesse GW, Sori SB. Proportion of glaucoma among voluntary people coming for glaucoma screening program at Jimma University Department of Ophthalmology, Jimma, Ethiopia. Ethiop J Health Sci. 2020;30(1):13–22. doi:10.4314/ejhs.v30i1.3
8. Burton MJ, Ramke J, Marques AP, et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Glob Health. 2021;9(4):489–551.
9. Assi L, Chamseddine F, Ibrahim P, et al. A global assessment of eye health and quality of life: a systematic review of systematic reviews. JAMA Ophthalmol. 2021;2021:1–16.
10. Jenkinson C Quality of life. Encyclopaedia Britannica, Inc; 2020. Available from: https://www.britannica.com/topic/quality-of-life.
11. Angeles-Han ST, Griffin KW, Harrison MJ, et al. Development of a vision-related quality of life instrument for children ages 8–18 years for use in juvenile idiopathic arthritis-associated uveitis. Arthritis Care Res. 2011;63(9):1254–1261. doi:10.1002/acr.20524
12. Skalicky S, Goldberg I. Depression and quality of life in patients with glaucoma: a cross-sectional analysis using the geriatric depression scale-15, assessment of function related to vision, and the glaucoma quality of life-15. J Glaucoma. 2008;17(7):546–551. doi:10.1097/IJG.0b013e318163bdd1
13. Ayele FA, Zeraye B, Assefa Y, Legesse K, Azale T, Burton MJ. The impact of glaucoma on quality of life in Ethiopia: a case-control study. BMC Ophthalmol. 2017;17(1):248–256. doi:10.1186/s12886-017-0643-8
14. Zhou C, Qian S, Wu P, Qiu C. Quality of life of glaucoma patients in China: sociodemographic, clinical, and psychological correlates—a cross-sectional study. Qual Life Res. 2014;23(3):999–1008. doi:10.1007/s11136-013-0518-2
15. Montana CL, Bhorade AM. Glaucoma and quality of life: fall and driving risk. Curr Opin Ophthalmol. 2018;29(2):135–140. doi:10.1097/ICU.0000000000000455
16. Nassiri N, Mehravaran S, Nouri-Mahdavi K, Coleman AL. national eye institute visual function questionnaire: usefulness in glaucoma. Optom Vis Sci. 2013;90(8):745–753. doi:10.1097/OPX.0000000000000003
17. Sleath B, Sayner R, Vitko M, et al. Glaucoma patient-provider communication about vision quality-of-life. Patient Educ Couns. 2017;100(4):703–709. doi:10.1016/j.pec.2016.11.018
18. Biggerstaff KS, Lin A. Glaucoma and quality of life. Int Ophthalmol Clin. 2018;58(3):11–22. doi:10.1097/IIO.0000000000000230
19. Nelson P, Aspinall P, Papasouliotis O, Worton B, O’Brien C. Quality of life in glaucoma and its relationship with visual function. J Glaucoma. 2003;12:2. doi:10.1097/00061198-200304000-00009
20. Canadian Ophthalmological Society Glaucoma Clinical Practice Guideline Expert Committee. Canadian ophthalmological society evidence-based clinical practice guidelines for the management of glaucoma in the adult eye. Can J Ophthalmol. 2009;44:7–54.
21. World Health Organization. Blindness and vision impairment; 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment.
22. Zhao C, Li J, Cun Q, et al. Impact of binocular integrated visual field defects on healthy related quality of life in glaucoma. Medicine. 2021;100(2):1–10.
23. Onakoya AO, Mbadugha CA, Aribaba OT, Ibidapo OO. Quality of life of primary open angle glaucoma patients in Lagos, Nigeria: clinical and sociodemographic correlates. J Glaucoma. 2012;21(5):287–295. doi:10.1097/IJG.0b013e31820d7cfd
24. Dhawan M, Hans T, Sandhu PS, Midha N. Evaluation of vision-related quality of life in patients with glaucoma: a hospital-based study. J Curr Glaucoma Pract. 2019;13(1):9–15. doi:10.5005/jp-journals-10078-1242
25. Lee JW, Chan CW, Chan JC, Li Q, Lai JS. The association between clinical parameters and glaucoma-specific quality of life in Chinese primary open-angle glaucoma patients. Hong Kong Med J. 2014;20(4):274–278. doi:10.12809/hkmj134062
26. Goldberg I, Clement CI, Chiang TH, et al. Assessing quality of life in patients with glaucoma using the Glaucoma Quality Of Life-15 (GQL-15) questionnaire. J Glaucoma. 2009;18(1):6–12. doi:10.1097/IJG.0b013e3181752c83
27. van Gestel A, Webers CAB, Beckers HJM, et al. The relationship between visual field loss in glaucoma and health-related quality-of-life. J CME. 2010;24(12):1759–1769.
28. Gessesse GW, Damji KF. Advanced glaucoma: management pearls. Middle East Afr J Ophthalmol. 2013;20(2):131. doi:10.4103/0974-9233.110610
29. Hamedani M, Dulley B, Murdoch I. Glaucoma and glare. Eye. 2021;35(6):1741–1747. doi:10.1038/s41433-020-01164-8
30. Wu N, Kong X, Gao J, Sun X. Vision-related quality of life in glaucoma patients and its correlations with psychological disturbances and visual function indices. J Glaucoma. 2019;28(3):207–215. doi:10.1097/IJG.0000000000001178
31. Labiris G, Katsanos A, Fanariotis M, Zacharaki F, Chatzoulis D, Kozobolis VP. Vision-specific quality of life in Greek glaucoma patients. J Glaucoma. 2010;19(1):39–43. doi:10.1097/IJG.0b013e31819d5cf7
32. Sathyamangalam RV, Paul PG, George R, et al. Determinants of glaucoma awareness and knowledge in urban Chennai. Indian J Ophthalmol. 2009;57(5):355–360. doi:10.4103/0301-4738.55073
33. Tenkir A, Solomon B, Deribew A. Glaucoma awareness among people attending ophthalmic outreach services in Southwestern Ethiopia. BMC Ophthalmol. 2010;10(1):17. doi:10.1186/1471-2415-10-17
34. Alemu DS, Gudeta AD, Gebreselassie KL. Awareness and knowledge of glaucoma and associated factors among adults: a cross sectional study in Gondar Town, Northwest Ethiopia. BMC Ophthalmol. 2017;17(1):154. doi:10.1186/s12886-017-0542-z
35. Anbesse DH, Gessesse W. Knowledge and practice towards glaucoma among glaucoma patients at University of Gondar Tertiary Eye Care and Training Center. Eur J Ophthalmol. 2022;2022:11206721221074203.
36. Majerníková Ľ, Hudáková A, Obročníková A, Grešš Halász B, Kaščáková M. Quality of life of patients with glaucoma in Slovakia. Int J Environ Res Public Health. 2021;18(2):485. doi:10.3390/ijerph18020485
37. Machado LF, Kawamuro M, Portela RC, et al. Factors associated with vision-related quality of life in Brazilian patients with glaucoma. Arq Bras Oftalmol. 2019;82:463–470. doi:10.5935/0004-2749.20190089
38. Heijl A, Bengtsson B, Hyman L, Leske MC. Natural history of open-angle glaucoma. Ophthalmology. 2009;116(12):2271–2276. doi:10.1016/j.ophtha.2009.06.042
39. Takahashi G-I, Otori Y, Urashima M, Kuwayama Y. Evaluation of quality of life in Japanese glaucoma patients and its relationship with visual function. J Glaucoma. 2016;25(3):150–156. doi:10.1097/IJG.0000000000000221
40. Lisboa R, Chun YS, Zangwill LM, et al. Association between rates of binocular visual field loss and vision-related quality of life in patients with glaucoma. JAMA Ophthalmol. 2013;131(4):486–494. doi:10.1001/jamaophthalmol.2013.2602
41. McKean-Cowdin R, Varma R, Wu J, Hays RD, Azen SP. Severity of visual field loss and health-related quality of life. Am J Ophthalmol. 2007;143(6):1013–1023. doi:10.1016/j.ajo.2007.02.022
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.