Back to Journals » International Journal of General Medicine » Volume 13
Violence Against Healthcare Workers at Primary Care Centers in Dammam and Al Khobar, Eastern Province, Saudi Arabia, 2019
Authors Alsmael MM , Gorab AH, AlQahtani AM
Received 12 June 2020
Accepted for publication 2 September 2020
Published 22 September 2020 Volume 2020:13 Pages 667—676
DOI https://doi.org/10.2147/IJGM.S267446
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mustafa M Alsmael,1 Ali H Gorab,1 Areej M AlQahtani2
1Family Medicine Academy, First Health Cluster, Ministry of Health, Dammam, Saudi Arabia; 2First Health Cluster, Ministry of Health, Al Khobar, Saudi Arabia
Correspondence: Ali H Gorab PO Box 1162, Al Khobar 31952, Kingdom of Saudi Arabia
Tel +966 50 680 6538
Fax +966 13 891 1159
Email [email protected]
Purpose: Workplace violence is common throughout the world. It causes many serious problems in the healthcare sector, where it significantly impacts healthcare workers, the services provided, and organizations as a whole. However, few studies have investigated these issues in Saudi Arabia. This study examined the prevalence of violence against healthcare workers at primary care centers in Dammam and Al Khobar, in the Eastern Province of Saudi Arabia. The study also assessed the types, perpetrators, perceived causes, and consequences related to such violence. Here, the aim was to understand how healthcare workers responded to violence and gauge their awareness of a reporting system.
Patients and Methods: A total of 360 healthcare workers (180 each from primary care centers in Dammam and Al Khobar) were invited to complete structured, self-administered questionnaires. As such, this study employed a cross-sectional analytical design.
Results: The prevalence of workplace violence among all participating health workers was 46.9%, with approximately 90% of these workers reporting verbal violence, 34.3% having been subject to intimidation, and 3% reporting physical violence. Approximately 75% reported that violent events were initiated by patients, while 45.6% reported that the events were initiated by patients’ companions. Healthcare workers’ reactions included reporting events to their supervisors or the police, but 46.7% said they did nothing; the most common reason was perceived inefficacy. Finally, only 36.4% of all participants were aware of a violence reporting system.
Conclusion: This study showed that healthcare workers were commonly exposed to different forms of violence, but often either did not react to it or did not report it. Further, there was relatively little awareness of how to manage and report workplace violence, thus indicating the need for healthcare workers to receive relevant education and training. A national program should also be established to track and prevent workplace violence.
Keywords: cross-sectional study; exposure to violence, health personnel, primary health care, workplace violence
Introduction
Healthcare workers (HCWs) care for the diseased and ailing either directly (eg, as doctors and nurses) or through ancillary services (eg, as medical waste handlers). These workers are at high risk of violence; indeed, estimates indicate that 8–38% of all HCWs experience physical violence at some point in their careers, with many more are exposed to verbal violence.1 Another form of violence is intimidation or threats, defined as “expressions of intent to cause harm, including verbal threats, threatening body language, and written threats.”2 These issues lead to serious consequences for HCWs, patients, and entire organizations.3 Many healthcare professionals may experience anxiety, physical depletion, anger, work absence, the desire to change jobs, and poor professional recruitment.3,4
An expert meeting organized by the European Commission in 1994 defined workplace violence as “incidents where staff are abused, threatened or assaulted in circumstances related to their work, including commuting to and from work, involving an explicit or implicit challenge to their safety, well-being, and health.”5 The National Institute for Occupational Safety and Health (NIOSH) defined workplace violence as “violent acts (including physical assaults and threats of assaults) directed to persons at work or on duty.”2 Perpetrators of violence include patients, the relatives of patients, and visitors or coworkers (collegial or horizontal violence).3 The risk factors associated with instances of workplace violence initiated by patients have further been divided into those related to staff members (such as inadequate or nonexistent training for dealing with violence, understaffing, and working alone), the work environment (including poor security and long wait times), and issues affecting patients (such as altered mental states or substance abuse).6,7 HCWs also respond to workplace violence in a wide variety of ways, with underreporting being very common, which contributes to a general underestimation of the problem’s scope.7 This is compounded by the existence of several barriers to reporting, including the idea that violence is part of the job, uncertainty over what constitutes violence, the belief that perpetrators are not in full control of themselves due to substance abuse or mental illness, the notion that no corrective actions will be taken, and a general lack of awareness about policies and reporting systems.7
While a great deal of research has been conducted on this topic throughout the world, studies have employed many different methodologies, definitions for violence against HCWs, study populations, settings, and variables, thus making comparisons difficult. However, important results have emerged. For instance, a study conducted by the Spanish Medical Association in 2014 showed that 48% of aggressions against HCWs occurred in the primary care setting, 16% in hospitals, 10% during ambulatory emergencies, and 16% in other settings.8 A large 2015 study conducted among six hospitals in the United States that included more than 5000 HCWs showed that 50% of violent events were perpetrated by patients or visitors, with a 12-month prevalence rate of 39% and the majority of events defined as verbal abuse.9 A similar study conducted in North China in 2017 among 1899 HCWs (including doctors, nurses, and various others) throughout seven hospitals found that 83.3% of respondents had reported violence, with 68.9% having reported nonphysical violence.10
Several studies have also been conducted in the Middle East. For example, a nationwide Iranian study published in 2018 was conducted among 6500 participants (78.5% nurses) at teaching hospitals to investigate physical violence against HCWs; results showed that many (23.5%) reported physical violence, while the main victims were nurses (78%), and the most frequent perpetrators were family members of patients (56%).11 A 2015 study conducted in 14 emergency departments in Palestine investigated 444 participants (nurses, physicians, and administrative staff) and found that 76.1% had experienced workplace violence during the 12-month period prior to study, with 35.6% reporting physical violence and 71.2% reporting non-physical violence.12 Finally, a 2017 cross-sectional study conducted among 134 emergency department workers in Egypt found that 59.7% had experienced violence (58.2% verbal and 15.7% physical); however, only 23.8% of the physical and 29.5% of the verbal events were reported to hospital authorities.13
While it is not uncommon to hear about victims of violence, and even murders, among healthcare providers in Saudi Arabia, very few studies have investigated the issue. A 2018 cross-sectional study conducted among 738 HCWs throughout two government hospitals and 10 primary health care centers (PHCCs) in Abha City showed that 57.5% had experienced workplace violence at least once, with 55.9% of cases involving verbal abuse, 11.1% involving physical abuse, and 32.9% involving both types.14 Further, a 2016 cross-sectional study conducted among 267 HCWs at four family medicine centers operating in a military medical city in Riyadh revealed that 45.6% had experienced work-related violence during the 12-month period prior to study, with 94.3% of those respondents having experienced verbal abuse, 6.5% having experienced physical abuse, and 22% having experienced intimidation.15 Another 2016 study conducted among 370 nurses at a university hospital in Riyadh found that almost half had experienced violence, with verbal violence being the most frequent type.16 A similar study was conducted at a university hospital in the Eastern Province in 2015 among 450 nurses, in which 30.7% reported experiencing verbal abuse in the 12-month period prior to the study.17 A 2012 cross-sectional study conducted among 258 HCWs at two public hospitals in Riyadh showed that 67.4% had experienced violence during the 12-month period prior to study,18 while a 2010 cross-sectional study conducted among 1091 HCWs in Al-Hassa City found that 28% had experienced at least one violent event during the previous year, the majority emotional/verbal abuse (92.1%) versus physical violence (7.9%).19
When it comes to the risk factors of violence in healthcare settings, the abovementioned study in Spain found that violent events were caused by dissatisfaction with provided care (36.3%), wait times (17.0%), and pharmaceutical prescriptions (12.9%).8 Further, a study in the United States found that many such events stemmed from altered mental states and behavioral issues (63.7%), pain/medication withdrawal (37.8%), and dissatisfaction with care (33.3%).9 In the Middle Eastern context, a study in Palestine found that the main perceived reasons for violence against HCWs were long wait times, lack of prevention measures, and unmet expectations.12 In the Abha City study mentioned earlier, HCWs perceived the main reasons for violence to be patients’ or relatives’ lack of education and long wait times followed by culture and personality issues, understaffing, overcrowding, workloads, and a lack of security.14 On the HCW side, the abovementioned study in Riyadh found that 72% of participants reported lacking an encouraging environment for submitting official violence reports; although 58.8% knew that such a reporting system was available, 22.8% reported no system was available, while 18.4% said they did not know whether one existed.15 Perhaps most notably, 48% of responding HCWs who experienced violence did nothing about it.15 Another local study found that most participants (70.8%) were aware that procedures for reporting violence existed; however, 86.7% of verbal abuse victims did not report the incident, mainly (45.5%) due to the perceived ineffectiveness of available procedures.17
However, few studies have investigated these issues in Saudi Arabia, especially in the Eastern Province. As such, this survey study examined the prevalence of violence against primary HCWs in Dammam and Al Khobar in the Eastern Province of Saudi Arabia. We specifically aimed to identify types of violence, perpetrators, perceived causes, and consequences, while assessing HCWs’ responses to violence and their levels of awareness about the Ministry of Health’s reporting system.
Materials and Methods
This cross-sectional survey study was conducted at PHCCs in Dammam and Al Khobar, Saudi Arabia from May to August 2019. Approval was first obtained from the Institutional Review Board of the Ministry of Health in the Eastern Province. All study objectives were explained to participating HCWs prior to interviews. Those who verbally agreed to participate also provided written informed consent. The self-administered questionnaire used in this study was previously developed based on previous literature and the International Labour Office/International Council of Nurses/WHO/Public Services International questionnaire and validated by Al Turki et al15 It was administered face-to-face in both English and Arabic by a recruited team that was monitored to ensure research quality. Confidentiality and anonymity were also preserved.
The PHCCs were selected via multistage clustering and a systematic random sampling technique. Stage 1 involved two clusters, including 15 PHCCs (50%) from Dammam and seven from Al Khobar (50%). All PHCCs were then ranked from high to low based on HCW coverage. In stage 2, questionnaires were distributed to all HCWs at participating PHCCs. These consisted of three parts, including one to gather demographic characteristics (eg, age, gender, marital status, occupation, and nationality), another to assess occupational history, and a third to determine factors related to violence reporting.
The required sample size was calculated using the Raosoft website (http://www.raosoft.com/samplesize.html; 5% margin of error and 95% CI) based on HCW numbers in Al Khobar and Dammam. Based on these calculations, a sufficient sample size was found to be 360 participants. As such, the final sample consisted of 360 total HCWs, with a response rate of 64%. All statistical analyses were conducted using IBM SPSS for Windows, Version 23.0 (IBM Corporation, Armonk, NY, USA). Descriptive statistics were calculated and presented as frequencies and percentages for categorical variables, while means and standard deviations were used for numerical variables. A chi-square test was conducted to assess the associations between demographic and occupational characteristics and workplace violence. Significance levels were set to 5% (p-values of 0.05).
Results
This study recruited a total of 360 HCWs at PHCCs, with equal numbers from Dammam and Al Khobar. The mean age of participating HCWs was 34.7±6.4. The majority were women who usually worked with both male and female patients. Most participants were doctors and nurses. The vast majority of participants were Saudis who worked the morning shift, usually with more than 10 coworkers. Most had ≥6 years of work experience, while very few had less than one year (Table 1).
 |
Table 1 Demographic and Occupational Characteristics of Participating Healthcare Workers (n = 360) |
In this study, approximately half of the participants had experienced workplace violence, the majority in the form of verbal violence, followed by intimidation, with physical violence being the least common.
The vast majority of violent incidents occurred inside the workplace during the morning shift. Most offenders were male, and four out of five were 21–45 years of age. Moreover, participants said that three-quarters of the violent events were perpetrated by patients, while nearly half were initiated by patients’ companions. Further, the majority of participants were not aware of having a violence reporting system in their institute. Among those who reported available systems, 59.5% knew how to use them, while 26.7% said there was no encouragement to do so at their institutes (Table 2).
 |
Table 2 Types and Characteristics of Violence Against Participating Healthcare Workers |
The most commonly reported perceived causes of violent events were the lack of a penalty for the offender and overcrowding. In descending order, the next most common were misunderstandings, long wait times, inadequate training, and unmet service demands (Table 3). As for the consequences, the majority of participants reported that nothing occurred, followed by decreased performance, feeling guilty, and absenteeism. While many reported monthly violent events, an even higher percentage reported a greater frequency of violence. Participant reactions toward violent events varied; 46.7% said they did nothing, 46.2% said they reported it to their supervisors, and about 6% notified the police. Inefficacy was the most commonly reported reason when asked why they did not react to the violent event, while most were unsatisfied with the consequences. Notably, most participants believed that the violent events they experienced were preventable (Table 3).
 |
Table 3 The Mechanisms of Violence and Subsequent Reactions of Targeted Healthcare Workers |
The mean age of participating HCWs (34.7±6.4) was similar among those who had and had not been exposed to workplace violence (Table 4).
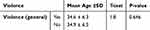 |
Table 4 Comparing Mean Ages of Healthcare Workers Who Experienced Violence to Those Who Had Not |
While analyses revealed that gender, marital status, occupation, nationality, city, and experience were not significant factors for exposure to workplace violence (Table 5), significant associations were found for some workplace characteristics, including awareness of the available violence reporting system and perceived reporting system effectiveness (Table 6). More violence was reported among participants who were not aware of a violence reporting system at their workplaces than those who reported having such a system. Similarly, more violence was experienced among those who thought their system was ineffective than those who reported having an effective system.
 |
Table 5 Associations Between Demographic Characteristics of Participating Healthcare Workers and Violent Events |
 |
Table 6 Associations Between Workplace Characteristics and Violent Events |
Discussion
This study investigated workplace violence among HCWs at Ministry of Health primary care centers, which in Saudi Arabia are the major providers of primary care services and are responsible for providing access to secondary care through referrals. Few other studies have examined this topic in Saudi Arabia, and the majority were conducted in hospitals.14–19
A total of 47% of HCWs in this study experienced workplace violence during the 12-month period prior to our investigation. This is very similar to reports from a study conducted at family medicine centers in Riyadh (45.6%), but it substantially exceeds the rate reported in two other studies conducted in the Eastern Province, in Al Khobar (30.7%) and Alhassa (28%).15,17,19 However, this study’s rate was lower than those reported by others in Abha (57.5%) and Riyadh (67%).14,18 The higher prevalence rates found in these two studies may be because they were conducted among HCWs in hospitals where patients were typically sicker and more volatile.2 Further, international prevalence rates vary widely, ranging from 39% in the United States to 83% in China.9,10
Our survey revealed that verbal violence was the most common, comprising 90% of the total. This finding is consistent with many local and international studies. For instance, the abovementioned study by Al-Turki et al15 found that verbal violence comprised 94% of all total violent incidents. Further, a cross-sectional study conducted in Chinese hospitals showed that 59.6% of participants were victims of psychological violence.20 That study also found the prevalence rate of physical violence to be 9.6%, while the present study found a physical violence prevalence rate of 3%, which is consistent with other local studies that found rates ranging from 5% to 12%, with the highest rates found among hospital care workers.14–16,18–20 However, violence in general and physical violence in particular are more prevalent in certain healthcare settings, such as high-volume emergency departments, psychiatric wards, and geriatric care units.2,21 For example, a national survey conducted in the United States among emergency medicine residents and attending physicians found a violence prevalence rate of 78%, with physical violence constituting 21% of cases.22 Further, in a local study conducted at three psychiatric hospitals in 2017 among 310 nurses, 90.3% reported workplace violence, with 57.7% reporting both verbal and physical abuse.23
The profile of the most frequent perpetrator found in this study was as follows: a patient, male or female (similar rates, constituting 60%) between 21 and 45 years of age, who committed violence inside the workplace. With the exception of gender, which was found to be predominately male, the same profile was reported by another local study.15 However, this differs from Algwaiz et al’s finding that patients’ friends and/or relatives were the most frequent sources of violence.18 This study found that doctors and nurses were equally exposed to violence (50% and 48%, respectively), followed by clerks (44%) and pharmacists (33%), which contradicts the finding by Alqwaiz et al that nurses were more likely to experience violence (76.3%) than physicians (50.7%; P < 0.001).18 Although any hospital worker may be a victim of violence, those with the most direct contact with patients are thought to be at higher risk.2 This study found that most violent events (99%) occurred during the morning shift, as few PHCCs in the region have evening shifts. Other local studies found that HCWs working evening and night shifts or working multiple/variable shifts were at greater risk of violence (P < 0.001).14,15 On the other hand, neither the demographic characteristics of violence perpetrators nor victims were significant predictors of workplace violence, which is also consistent with other local and international studies.15,24
The causes of violence differed according to the setting and type of care provided, among other factors.2 The most common perceived causes of violence found in this study were, in descending order, lack of penalty for the offender, overcrowding, lack of security, misunderstanding, long waiting times, inadequate training for dealing with violence, and unmet service demands. These and other causes (eg, drugs and alcohol, access to firearms) are known to increase the risk of workplace violence.2 It is thus essential to identify the specific risk factors for violence, thereby enabling the development of appropriate violence prevention programs in the workplace; in this regard, worker participation is paramount.2 It is also worth noting that Ministry of Health primary care centers lack security officers, a concern that should be addressed.
In this study, 46% of participants responded to workplace violence by doing nothing, while a different 46% reported the events to their supervisors. Other responses were requesting to move from the workplace, consulting a colleague or friend, and reporting to the police, with similar frequencies of about 5% each. Around 39% of those who responded to violence by doing nothing chose this option because they thought the results would be inefficient. Most participants who were exposed to violence thought the events were preventable, a finding which is consistent with other local studies.15,17 NIOSH suggests that violence can be prevented by altering worker practices and administrative procedures.2 A local study also showed that around 58% of those exposed to violence reported that they did not know how to respond at all, and a similar percentage somewhat knew how to handle an aggressive person.14 Similar findings were shown in a study conducted among nurses in five European countries in 2016, finding that 71.7% of verbal abuse incidents and 69.9% of physical attacks were not reported, mainly because victims believed reporting to be unimportant or useless.25 Such a lack of response results in the underreporting of violence, which leads to the underestimation of a problem that is thought to be common.26 Many HCWs also believe that exposure to violence is part of the job, which further contributes to underreporting.7 NIOSH recommends an atmosphere of open communication, in which HCWs are provided with written procedures about how to respond to and report violence.2 In this study, around 77% of HCWs were dissatisfied with the consequences of their experience with a violent event. This is similar to what Al-Turki et al15 found at family medicine centers in Riyadh.
The absence of clear policies and training programs for identifying and managing hostile and assaultive behaviors at healthcare organizations is thought to increase the risk of workplace violence.27 In this study, approximately two-thirds of all participants were unaware of a system for reporting violence at their respective institutes, while around half of those who were aware of such a system did not know how to use it and believed there was no encouragement for reporting violent events. However, HCWs who were aware of reporting systems were less likely to experience violence, especially those who thought the system was effective; further, this relationship was statistically significant (P < 0.001). A local study showed that 58.8% of participants were aware of a reporting system at their institute, but that only 70% knew how to use it.15 The overall increased level of awareness found in that study may have been because the workplace was located at a military institute, which may have implemented clearer policies. However, 75% of those participants thought there was no encouragement for reporting violent events.15 The abovementioned study in Abha City also found that 60% of HCWs were trained to manage violent events.14 Higher levels of awareness about the presence of a reporting system (80.6%) and how to use it (81.6%) were found in a study conducted among nurses in emergency departments in Oman.28 This could be, as reported by the same study’s participants, due to the presence of policies for violence prevention (38.8%) and training on workplace violence (42.7%).28
The present study has some limitations. The self-administered questionnaire may have been subject to recall bias. Also, our having explained the objectives of the study to participants makes social appeasement a possible limitation. As the study was carried out in the primary care sector and Ministry of Health facilities, results cannot be generalized to all HCWs in Saudi Arabia or other healthcare institutions.
Conclusion
In conclusion, this study found that HCWs were commonly exposed to different forms of violence and that inappropriate reactions were common. Further, a significant relationship was found between the awareness of an available reporting system that was thought to be effective and a lower prevalence of violence. However, there was an overall lack of awareness about managing and reporting workplace violence, which suggests that HCWs should receive relevant education and training. Finally, it may be necessary to develop a national program for tracking and preventing workplace violence.
This study’s results show that additional research is needed to assess the magnitude and impact of problems related to workplace violence in healthcare settings. Current findings suggest that several measures should be implemented, including training to improve communication skills for HCWs while helping them learn when to suspect and how to identify and manage workplace violence. It is also important to ensure that trained security officers are available to promote safety in the workplace, and measures should be taken to increase overall awareness of any violence reporting system, which HCWs should be encouraged to use when needed. Administrators should then take appropriate action to investigate reported incidents, thus helping prevent similar events while reducing the burdens of injury and stress on personnel. At a higher level, a national policy and prevention program may ultimately be needed to address workplace violence.
Abbreviations
HCWs, healthcare workers; NIOSH, National Institute for Occupational Safety and Health; PHCCs, primary health care centers; WHO, World Health Organization.
Acknowledgments
The authors would like to thank Dr. Mohamed A. Alamin for his reviews of the data analysis and results and Dr. Hashim H. Al-Nahwi for his contributions during data collection.
Disclosure
The authors report that they have no financial disclosures and no conflicts of interest in this work.
References
1. World Health Organization. Violence against health workers. Available from: https://www.who.int/violence_injury_prevention/violence/workplace/en/. Accessed April 20, 2020.
2. National Institute for Occupatioan Safety and Health (NIOSH) CfDCaPC. Violence: occupational hazards in hospitals. NIOSH Atlanta^ eGA GA. 2002;1:1254.
3. Edward K-L, Ousey K, Warelow P, Lui S. Nursing and aggression in the workplace: a systematic review. Brit J Nurs. 2014;23(12):653–659.
4. Lanctôt N, Guay S. The aftermath of workplace violence among healthcare workers: a systematic literature review of the consequences. Aggress Violent Behav. 2014;19(5):492–501. doi:10.1016/j.avb.2014.07.010
5. Milczarek M. Workplace Violence and Harassment: A European Picture. Publications Office of the European Union; 2010.
6. Martinez AJS. Managing workplace violence with evidence-based interventions: a literature review. J Psychosoc Nurs Ment Health Serv. 2016;54(9):31–36. doi:10.3928/02793695-20160817-05
7. Phillips JP. Workplace violence against health care workers in the United States. N Engl J Med. 2016;374(17):1661–1669. doi:10.1056/NEJMra1501998
8. Rincón-Del TT, Villanueva-Guerra A, Rodríguez-Barrientos R, et al. Aggressions towards primary health care workers in Madrid, Spain, 2011–2012. Rev Esp Salud Publica. 2016;90:e1−e12.
9. Pompeii LA, Schoenfisch AL, Lipscomb HJ, Dement JM, Smith CD, Upadhyaya M. Physical assault, physical threat, and verbal abuse perpetrated against hospital workers by patients or visitors in six US hospitals. Am J Ind Med. 2015;58(11):1194–1204. doi:10.1002/ajim.22489
10. Sun P, Zhang X, Sun Y, et al. Workplace violence against health care workers in North Chinese hospitals: a cross-sectional survey. Int J Environ Res Public Health. 2017;14(1):96. doi:10.3390/ijerph14010096
11. Fallahi-Khoshknab M, Oskouie F, Najafi F, Ghazanfari N, Tamizi Z, Afshani S. Physical violence against health care workers: a nationwide study from Iran. Iran J Nurs Midwifery Res. 2016;21(3):232. doi:10.4103/1735-9066.180387
12. Hamdan M, Abu Hamra A. Workplace violence towards workers in the emergency departments of Palestinian hospitals: a cross-sectional study. Hum Resourc Health. 2015;13(1):28. doi:10.1186/s12960-015-0018-2
13. Abdellah RF, Salama KM. Prevalence and risk factors of workplace violence against health care workers in emergency department in Ismailia, Egypt. Pan Afr Med Jl. 2017;26(1):1–8.
14. Alsaleem SA, Alsabaani A, Alamri RS, et al. Violence towards healthcare workers: a study conducted in Abha City, Saudi Arabia. J Fam Community Med. 2018;25(3):188.
15. Al-Turki N, Afify AA, AlAteeq M. Violence against health workers in family medicine centers. J Multidiscip Healthc. 2016;9:257.
16. Alkorashy HAE, Al Moalad FB. Workplace violence against nursing staff in a Saudi university hospital. Int Nurs Rev. 2016;63(2):226–232. doi:10.1111/inr.12242
17. Al-Shamlan NA, Jayaseeli N, Al-Shawi MM, Al-Joudi AS. Are nurses verbally abused? A cross-sectional study of nurses at a university hospital, Eastern Province, Saudi Arabia. J Family Community Med. 2017;24(3):173. doi:10.4103/jfcm.JFCM_45_17
18. Algwaiz WM, Alghanim S. Violence exposure among health care professionals in Saudi public hospitals. Saudi Med J. 2012;33(1):76–82.
19. El-Gilany A-H, El-Wehady A, Amr M. Violence against primary health care workers in Al-Hassa, Saudi Arabia. J Interpers Violence. 2010;25(4):716–734. doi:10.1177/0886260509334395
20. Liu W, Zhao S, Shi L, et al. Workplace violence, job satisfaction, burnout, perceived organisational support and their effects on turnover intention among Chinese nurses in tertiary hospitals: a cross-sectional study. BMJ Open. 2018;8(6):e019525. doi:10.1136/bmjopen-2017-019525
21. Kowalenko T, Gates D, Gillespie GL, Succop P, Mentzel TK. Prospective study of violence against ED workers. Am J Emerg Med. 2013;31(1):197–205. doi:10.1016/j.ajem.2012.07.010
22. Behnam M, Tillotson RD, Davis SM, Hobbs GR. Violence in the emergency department: a national survey of emergency medicine residents and attending physicians. J Emerg Med. 2011;40(5):565–579. doi:10.1016/j.jemermed.2009.11.007
23. Basfr W, Hamdan A, Al-Habib S. Workplace violence against nurses in psychiatric hospital settings: perspectives from Saudi Arabia. Sultan Qaboos Univ Med J. 2019;19(1):e19. doi:10.18295/squmj.2019.19.01.005
24. Gates D, Gillespie G, Kowalenko T, Succop P, Sanker M, Farra S. Occupational and demographic factors associated with violence in the emergency department. Adv Emerg Nursing J. 2011;33(4):303–313. doi:10.1097/TME.0b013e3182330530
25. Babiarczyk B, Turbiarz A, Tomagová M, Zeleníková R, Önler E, Sancho Cantus D. Violence against nurses working in the health sector in five European countries—pilot study. Int J Nurs Pract. 2019;25(4):e12744. doi:10.1111/ijn.12744
26. Wolf LA, Delao AM, Perhats C. Nothing changes, nobody cares: understanding the experience of emergency nurses physically or verbally assaulted while providing care. J Emerg Nurs. 2014;40(4):305–310. doi:10.1016/j.jen.2013.11.006
27. Occupational Safety and Health Administration. Guidelines for Preventing Workplace Violence for Healthcare and Social Service Workers (OSHA Publication 3148–06R). Washington: Department of Labor; 2016.
28. Al‐Maskari S, Al‐Busaidi I, Al‐Maskari M. Workplace violence against emergency department nurses in Oman: a cross‐sectional multi‐institutional study. Int Nurs Rev. 2020;67(2):249–257. doi:10.1111/inr.12574
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
