Back to Journals » International Journal of General Medicine » Volume 13
Vertebrobasilar Dolichoectasia as a Rare Cause of Simultaneous Abducens and Vestibulocochlear Nerve Symptoms: A Case Report and Literature Review
Authors Zang X, Feng Z, Qiao H, Wang L, Fu C
Received 27 June 2020
Accepted for publication 4 August 2020
Published 20 August 2020 Volume 2020:13 Pages 523—527
DOI https://doi.org/10.2147/IJGM.S269649
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Xuege Zang,1,* Zheng Feng,2,* Hui Qiao,1 Libo Wang,1 Chao Fu3
1Department of Neurology, China-Japan Union Hospital of Jilin University, Changchun, People’s Republic of China; 2Department of Pediatrics, China-Japan Union Hospital of Jilin University, Changchun, People’s Republic of China; 3Department of Neurosurgery, China-Japan Union Hospital of Jilin University, Changchun, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Libo Wang; Chao Fu Email [email protected]; [email protected]
Abstract: Vertebrobasilar dolichoectasia (VBD) can lead to cranial nerve symptoms. However, multiple cranial nerve symptoms associated with VBD in one case remain extremely rare. We here present the case of a 33-year-old male with VBD diagnosed by multimodality imaging, who developed simultaneous abducens and vestibulocochlear nerve symptoms and subsequently improved after blood pressure control treatment. To our knowledge, this is the first report of such a vascular disorder resulting in simultaneous symptoms of the abducens and vestibulocochlear nerves. This study highlights that such a vascular anomaly should be considered when cranial nerve symptom is encountered, especially when multiple cranial nerves involved. Meanwhile, radiological evaluation of such neurovascular conflict using three-dimensional constructive interference in steady-state imaging is recommended.
Keywords: vertebrobasilar dolichoectasia, cranial nerve, abducent nerve, vestibulocochlear nerve, nerve compression syndrome
Introduction
Vertebrobasilar dolichoectasia (VBD) is a vascular anomaly characterized by marked ectasia, elongation, and tortuosity of the vertebrobasilar arteries, with a reported prevalence of 0.05–18%. Most often, it is associated with ischemic or hemorrhagic stroke, but this entity may also cause compressive symptoms of cranial nerves.1–5 In the majority of the reported cases, the facial and trigeminal nerves are more susceptible to be involved, resulting in hemifacial spasm and trigeminal neuralgia, respectively.6,7 In contrast, abducens, trochlear, vestibular, glossopharyngeal or vagus nerve impairment caused by neurovascular compression of VBD is uncommon.7–12 Notably, multiple cranial nerve involvement in patients with VBD is extremely rare.7–9
Herein, we present a case of a 33-year-old patient with symptoms of the abducens and vestibulocochlear cranial nerves which were relieved by antihypertensive therapy. To the best of our knowledge, simultaneous abducens and vestibulocochlear nerve symptoms precipitated by VBD compression have not yet been reported.
Case Presentation
A 33-year-old man with a history of hypertension was admitted with intermittent binocular horizontal double vision, vertigo and left-sided tinnitus. In recent two months, diplopia was gradually worsening during leftward gaze. His vertigo occurred 5–10 times a day in a paroxysmal manner, with each episode lasting less than 5 minutes. He described the tinnitus as similar to the sound made by a typewriter. Admission blood pressure was 156/82 mmHg. Ocular motility examination showed limitation abduction of his left eye. Visual acuity, color vision, pupil size and reactivity were normal. Vestibular function test was normal, and no specific vestibular disorders existed, such as migrainous vertigo, Menière’s disease and vestibular neuritis. He had no ptosis, nystagmus, facial palsy, hemifacial spasm and hearing loss.
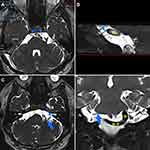
Admission non-contrasted computed tomography (CT) and magnetic resonance imaging (MRI) showed a markedly dilated and tortuous vessel, compressing the left dorsal pons (Figure 1A and B). Diffusion-weighted MRI revealed no infarct in the pons (Figure 1C). CT angiography confirmed that the basilar artery (BA) was dolichoectatic and curved to the left side, and the right vertebral artery (VA) was ectatic and tortuous (Figure 2). The maximum diameter of the BA was 5.9 mm. High-resolution MRI with 3D-constructive interference in steady-state (3D-CISS) revealed that a dolichoectatic BA was clearly compressed the abducent nerve and the vestibulocochlear nerve complex on the left side (Figure 3). Therefore, simultaneous compressive symptoms of the abducens and vestibulocochlear nerves associated with the VBD were diagnosed. Due to the surgical risk, the patient declined to undergo microvascular decompression, and conservative treatment with antihypertensive drugs (amlodipine, 5mg/day) was introduced. A target systolic blood pressure of <120 mm Hg was strictly maintained. His symptoms gradually improved, and he was discharged on day 10. During the 6-month follow-up period, his clinical condition remained stable, except mild diplopia, slight limitation of left abduction, and paroxysmal vertigo.
Discussion
Clinically, VBD is an uncommon vascular disease characterized by progressive ectasia, elongation, and tortuosity involving the vertebrobasilar system. The high frequency of risk factors associated with the occurrence of this entity includes old age, male sex, hypertension, and coronary artery disease.1,2,13,14 To date, the mechanism contributing to VBD has yet to be elucidated; several hypotheses such as trophic support depletion, reticular fiber deficiency, degeneration of the internal elastic lamina, and atrophy of the smooth muscle may be involved.15,16
Generally, VBD remains asymptomatic and is detected incidentally. Owing to the limited space within the posterior fossa, VBD is likely to lead to mechanical stress predominantly restricted to the cranial nerve and brainstem, which in turn can cause compressive symptom and vascular event, including cranial nerve palsy, and ischemic or hemorrhagic stroke.1,3,5,14 We conducted a thorough literature review of neurovascular compression associated with VBD, and found that the trigeminal and facial nerves are more prone to be commonly involved; abducens nerve palsy resulting from VBD-related compression is relatively rare.6,7,17,18 It is notable that multiple cranial nerve involvement in patients with VBD is rarely reported.7–9 Madhugiri et al8 described a patient with diplopia owing to a left abduction deficit, together with ipsilateral facial pain and facial muscle twitches, attributed to compression of the abducens, trigeminal and facial nerves caused by VBD, respectively. Pham et al7 reported a similar case, in which VBD resulting in both abducens and ipsilateral trigeminal nerve palsies. To the best of our knowledge, this is the first report of simultaneous abducens and vestibulocochlear nerve symptoms related to VBD in one case.
In the past, autopsy findings remained a main information source of this pathological condition; however, the increased application of multimodality diagnostic imaging has significantly improved our ability to identify VBD in living cases, such as CT/CT angiography, MRI/MR angiography, and catheter-based angiography.15,19 To date, the diagnostic criteria for BA dolichoectasia proposed by Smoker et al20 is widely used, in which BA diameter at the midpons > 4.5 mm was considered dolichoectasic. Passero and Rossi have suggested diameter cutoffs for the vertebral artery (≥4 mm) to indicate ectasia.3 We herein diagnosed the VBD on the basis of multimodality imaging in accordance with the above criteria. Neurovascular conflict is usually resulted from the responsible vessel compressing or indenting nerve roots as it traverses the basal cisterns close to the root entry zone. High-resolution 3D-CISS MR imaging has been reported useful in diagnosis and preoperative planning in patients with neurovascular conflict.21 Vestibulocochlear symptoms such as vertigo, nystagmus, sensorineural hearing loss, and tinnitus can be precipitated from a neurovascular compression of the vestibulocochlear nerve by VBD.9 In this study, the patient presented with symptoms of simultaneous abducens and vestibulocochlear nerves, which are presumed to be secondary to the VBD on the basis of the following remarks: (a) the patient presented with abducent and vestibulocochlear symptoms of intermittent left-sided diplopia, paroxysmal vertigo and left-sided typewriter tinnitus; (b) high-resolution images of 3D-CISS sequences has clearly showed that a dolichoectatic BA markedly conflicted with both abducens and vestibulocochlear nerve roots; (c) other pathologies such as vestibular disorder were absent.
In patients with dolichoectasia, BA diameter >4.3 mm may be a predictor of fatal stroke, highlighting the importance of this disease and necessitate proper and prompt treatment.22 Currently, no effective treatment for VBD itself exists due to the location and course of the anomaly and the important major and perforating arteries supplying the brainstem.2,15 For symptomatic neurovascular conflict, no specific treatment is available. Some studies reported that microvascular decompression has successfully treated vascular compression of the oculomotor, trochlear, trigeminal, abducent and facial nerves.23,24 However, most of reported cases, including the present case, received conservative management such as a strict blood pressure control because the surgical risk outweighed the benefits.25,26
Conclusion
When cranial nerve palsy is encountered, especially multiple cranial nerve involvement, VBD should be considered in the differential diagnosis. As far as we know, this is the first report of such a vascular disorder leading to simultaneous abducens and vestibulocochlear nerve symptoms. Moreover, high-resolution 3D-CISS MRI is useful to identify the neurovascular conflict.
Data Sharing Statement
The authors declare that they had full access to all of the data in this study, and the authors take complete responsibility for the integrity of the data. All original data are available in the China-Japan Union Hospital of Jilin University, Changchun, China. Data used to support the findings of this study are available from the corresponding author upon request.
Ethics and Consent Statement
Ethical approval was obtained by the ethics committee of the Ethics Review Board of the China-Japan Union Hospital of Jilin University.
Consent for Publication
A written permission for the use of patient data for publication was obtained.
Author Contributions
All authors made substantial contributions to acquisition of data, or analysis, conception and design, and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests for this work.
References
1. Gutierrez J, Sacco RL, Wright CB. Dolichoectasia-an evolving arterial disease. Nat Rev Neurol. 2011;7(1):41–50. doi:10.1038/nrneurol.2010.181
2. Pico F, Labreuche J, Amarenco P. Pathophysiology, presentation, prognosis, and management of intracranial arterial dolichoectasia. Lancet Neurol. 2015;14(8):833–845. doi:10.1016/S1474-4422(15)00089-7
3. Passero SG, Rossi S. Natural history of vertebrobasilar dolichoectasia. Neurology. 2008;70(1):66–72. doi:10.1212/01.wnl.0000286947.89193.f3
4. Shapiro M, Becske T, Riina HA, Raz E, Zumofen D, Nelson PK. Non-saccular vertebrobasilar aneurysms and dolichoectasia: a systematic literature review. J Neurointerv Surg. 2014;6(5):389–393. doi:10.1136/neurintsurg-2013-010793
5. Zhu Y, Thulborn K, Curnyn K, Goodwin J. Sixth cranial nerve palsy caused by compression from a dolichoectatic vertebral artery. J Neuroophthalmol. 2005;25(2):134–135. doi:10.1097/01.wno.0000165319.75310.5a
6. Fu C, Zhao C, Li D, Sun L, Hu Z, Yu W. Primitive trigeminal artery as a rare cause of trigeminal neuralgia. Vasa. 2015;44(2):140–144. doi:10.1024/0301-1526/a000420
7. Pham T, Wesolowski J, Trobe JD. Sixth cranial nerve palsy and ipsilateral trigeminal neuralgia caused by vertebrobasilar dolichoectasia. Am J Ophthalmol Case Rep. 2018;10:229–232. doi:10.1016/j.ajoc.2018.02.029
8. Madhugiri VS, Roopesh Kumar VR, Gopalakrishnan MS, Shankar Ganesh CV, Sudheer Kumar G. Cranial polyneuropathy associated with vertebrobasilar dolichoectasia. Clin Neurol Neurosurg. 2012;114(7):1059–1061. doi:10.1016/j.clineuro.2012.02.002
9. Huh G, Bae YJ, Woo HJ, Park JH, Koo JW, Song JJ. Vestibulocochlear symptoms caused by vertebrobasilar dolichoectasia. Clin Exp Otorhinolaryngol. 2020;13(2):123–132. doi:10.21053/ceo.2019.00780
10. Sunwoo W, Jeon YJ, Bae YJ, Jang JH, Koo JW, Song JJ. Typewriter tinnitus revisited: the typical symptoms and the initial response to carbamazepine are the most reliable diagnostic clues. Sci Rep. 2017;7(1):10615. doi:10.1038/s41598-017-10798-w
11. Nuti D, Passero S, Di Girolamo S. Bilateral vestibular loss in vertebrobasilar dolichoectasia. J Vestib Res. 1996;6(2):85–91. doi:10.3233/VES-1996-6203
12. Arishima H, Kikuta KI. Magnetic resonance imaging findings of isolated abducent nerve palsy induced by vascular compression of vertebrobasilar dolichoectasia. J Neurosci Rural Pract. 2017;8(1):124–127. doi:10.4103/0976-3147.193529
13. Yuan YJ, Xu K, Luo Q, Yu JL. Research progress on vertebrobasilar dolichoectasia. Int J Med Sci. 2014;11(10):1039–1048. doi:10.7150/ijms.8566
14. Del Brutto VJ, Ortiz JG, Biller J. Intracranial arterial dolichoectasia. Front Neurol. 2017;8:344. doi:10.3389/fneur.2017.00344
15. Samim M, Goldstein A, Schindler J, Johnson MH. Multimodality imaging of vertebrobasilar dolichoectasia: clinical presentations and imaging spectrum. Radiographics. 2016;36(4):1129–1146. doi:10.1148/rg.2016150032
16. Diekouadio F, Bakkari AE, Ayouche O, Mohamed DA, Chaoui B. Alternating hemiplegia revealing a vertebrobasilar dolichoectasia: a case report and review of the literature. Edorium J Radiol. 2019;5:100013R02FD2019. doi:10.5348/100013R02FD2019CR
17. Sadashiva N, Shukla D. Neurovascular conflict of abducent nerve. J Neurosci Rural Pract. 2017;8(1):3–4. doi:10.4103/0976-3147.193564
18. Narai H, Manabe Y, Deguchi K, Iwatsuki K, Sakai K, Abe K. Isolated abducens nerve palsy caused by vascular compression. Neurology. 2000;55(3):453–454. doi:10.1212/wnl.55.3.453
19. Bae YJ, Jeon YJ, Choi BS, Koo JW, Song JJ. The role of MRI in diagnosing neurovascular compression of the cochlear nerve resulting in typewriter tinnitus. AJNR Am J Neuroradiol. 2017;38(6):1212–1217. doi:10.3174/ajnr.A5156
20. Smoker WR, Corbett JJ, Gentry LR, Keyes WD, Price MJ, McKusker S. High-resolution computed tomography of the basilar artery: 2. Vertebrobasilar dolichoectasia: clinical-pathologic correlation and review. AJNR Am J Neuroradiol. 1986;7(1):61–72.
21. Garcia M, Naraghi R, Zumbrunn T, Rösch J, Hastreiter P, Dörfler A. High-resolution 3D-constructive interference in steady-state MR imaging and 3D time-of-flight MR angiography in neurovascular compression: a comparison between 3T and 1.5T. AJNR Am J Neuroradiol. 2012;33(7):1251–1256. doi:10.3174/ajnr.A2974
22. Pico F, Labreuche J, Gourfinkel-An I, Amarencox I; GENIC Investigators. Basilar artery diameter and 5-year mortality in patients with stroke. Stroke. 2006;37(9):2342–2347. doi:10.1161/01.STR.0000236058.57880.03
23. De Ridder D, Menovsky T. Neurovascular compression of the abducent nerve causing abducent palsy treated by microvascular decompression. Case report. J Neurosurg. 2007;107(6):1231–1234. doi:10.3171/JNS-07/12/1231
24. Yamazaki T, Yamamoto T, Hatayama T, et al. Abducent nerve palsy treated by microvascular decompression: a case report and review of the literature. Acta Neurochir (Wien). 2015;157(10):1801–1805. doi:10.1007/s00701-015-2530-5
25. Lin JY, Lin SY, Wu JI, Wang IH. Optic neuropathy and sixth cranial nerve palsy caused by compression from a dolichoectatic basilar artery. J Neuroophthalmol. 2006;26(3):190–191. doi:10.1097/01.wno.0000235579.57180.ae
26. Giray S, Pelit A, Kizilkilic O, Karatas M. Isolated abducens nerve palsy caused by contralateral vertebral artery dolichoectasia. Neurol India. 2005;53(2):246–247. doi:10.4103/0028-3886.16433
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.