Back to Journals » Clinical Ophthalmology » Volume 13
Verification and measurement of the side-cut angle of corneal flap in patients undergoing LASIK surgery using FS 200 kHz femtosecond laser system versus conventional mechanical microkeratome
Authors Taha S , Azzam S , Anis M , Zaazou C, Hosny M
Received 10 January 2019
Accepted for publication 8 April 2019
Published 10 June 2019 Volume 2019:13 Pages 985—992
DOI https://doi.org/10.2147/OPTH.S201150
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Sarah Taha, Sarah Azzam, Mohamed Anis, Cherif Zaazou, Mohamed Hosny
Department of Ophthalmology, Cairo University Hospital, Cairo, Egypt
Introduction: This is a prospective nonrandomized interventional clinical trial conducted to measure and verify the intended versus the achieved LASIK flap side-cut angle in two groups of patients, Femtosecond laser-assisted in-situ keratomileusis (FS-LASIK) using Wavelight FS200 (Alcon Laboratories Inc. Fort Worth, TX, USA) and the conventional mechanical microkeratme (Moria M2 90).
Methods: This prospective clinical trial was conducted on 40 eyes of 20 patients (20 eyes in each group) in the interval between December 2017 and August 2018. Heidelberg anterior segment OCT was done for the patients 2 weeks postoperatively to measure the corneal flap side cut angle.
Results: The achieved side-cut angles of all the patients in the first group (the femtosecond laser-assisted in-situ keratomileusis group) were equal to or more inverted than the intended angle (110–115°) in all the study candidates with a minimum angle (110°) and maximum angle (155°). Unlike the achieved side-cut angle in the second group (the mechanical microkeratome group) in which all the achieved side-cut angle were acute with a minimum angle (30°) and maximum angle (65°) which is more acute than the intended side-cut angle (70°).
Conclusion: In our study we found that the femtoLASIK technology was capable of making the flap side-cut angle more obtuse than the intended angle, unlike the achieved flap side-cut angle done using the mechanical microkeratome which was more acute than the intended angle in 100% of cases.
Keywords: FS-LASIK, mechanical microkeratome, corneal flap side-cut angle, >AS-OCT
Introduction
Lasik in Situ keratomileusis , (LASIK) is one of the most successful elective surgical procedures performed in the world for treatment of refractive error.1 Since the introduction of the FS laser in 2001, its technology has continued to evolve, making it the preferred method for LASIK flap creation for most cases. Dry eye is one of the most common side effects of LASIK surgery; symptoms may persist for 6 months after LASIK in up to 35% of patients.2 Variations in LASIK technique can improve or worsen the degree of dry eye symptoms.3 Lasik flaps made with a femtosecond laser have been correlated with longer tear break-up times and decreased dry eye compared with flaps made with a microkeratome. Advancements in laser technology enabled refractive surgeons to customize side-cut architecture, so the inverted side-cut flaps result in better wound healing and improved apposition of severed nerves because of the biomechanical superiority of the cut with femtosecond laser inverted side-cut flaps.4
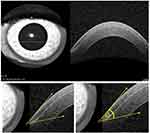 | Figure 5 Microkeratome LASIK flap with acute side-cut angle 43°.Abbreviation: LASIK, laser-assisted in situ keratomileusis. |
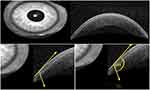 | Figure 6 FemtoLASIK flap side-cut angle 134°.Abbreviation: femtoLASIK, femtosecond laser-assisted in situ keratomileusis. |
Patients and methods
A prospective nonrandomized interventional clinical trial was conducted on 40 eyes (20 eyes per group) of 20 patients in the interval between December 2017 and August 2018. The study was approved by local ethical committee (Cairo University Hospitals Ethical Committee of research work) and followed the principles of Declaration of Helsinki. All patients were provided with a written informed consent. Subjects included were between 18 and 45 years of age, myopes up to −8.0 diopters without or with astigmatism up to −4.0 diopters; hypermetrope up to +4 diopters, with central corneal thickness of 500 microns or more; with normal corneal tomography, with a dioptre value of less than 1.6 in the Belin/Ambrosio Enhanced Ectasia Display of the Pentacam (Pentacam®, Oculus, Arlington, WA, USA) and an expected post-LASIK residual stromal bed of 300 microns or more. WaveLight® FS200 femtosecond laser (Alcon, Fort Worth, TX, USA) was used for the creation of the flap in the first group and Moria M2 90 mechanical microkeratome in the second group. The surgery was performed in both eyes and under topical anesthesia using three drops of topical benoxinate hydrochloride 0.4% applied 2–3 minutes before surgery (Benox; Eipico Inc., Cairo, Egypt). In the femtoLASIK group once appropriate centration was achieved the suction ring was applied to the sclera followed by corneal applanation. We used 200 kHz with pulse energy of 0.7 μJ, spot separation of 7.5 μm, and line separation of 7.5 μm for the flap bed, pulse energy of 0.85 µJ, spot separation of 5.5 µm and line separation of 3.5 µm for flap side cut and flap diameter was adjusted according to the intended treatment zone. The intended flap thickness was 120 μm with a side cut angle of 115°. After femtosecond laser flap creation, the bed moves to excimer laser Alcon WaveLight EX500 (Alcon) for laser ablation.
In the mechanical microkeratome group, the patient was positioned supine was asked to fixate on an illuminated ring with a central target.
Once appropriate centration was achieved, a suction ring was applied to the sclera. The flap was done by Microkeratome Moria M2 90 (Moria, Antony, France) (disposable blade) with the hinge placed superiorly, flap diameter was adjusted according to the intended treatment zone with flap thickness 120 µm side-cut angle around 70° in average. After laser treatment a blunt spatula was inserted through the incision site to break the remaining tissue bridges and lift the flap. Ablation was done. The bed is flushed with saline and the flap replaced followed by drying.
All patients received a topical antibiotic moxifloxacin hydrochloride (Vigamox, Alcon), a topical steroid (prednisolone acetate) and artificial tears eye drops for 3 weeks and systemic steroids ( prednisolone 20 mg) for 5 days.
Two weeks postoperatively Heidelberg anterior segment OCT was done for the patients to measure the corneal flap side cut angle.
Statistical analysis
Data were coded and entered using the statistical package SPSS version 25 (IBM Corporation, Armonk, NY, USA). Data was summarized using mean, standard deviation, median, minimum and maximum in quantitative data and using frequency (count) and relative frequency (percentage) for categorical data. Comparisons between quantitative variables were done using the non-parametric Mann–Whitney test . For comparing categorical data, chi squared (χ2) test was performed. Exact test was used instead when the expected frequency is less than 5. Correlations between quantitative variables were done using Spearman's correlation coefficient . P-values less than 0.05 were considered as statistically significant.
Results
Our study included 40 eyes of 20 patients (20 eyes in each group) with age range of 18–45 years. Patients underwent LASIK surgery using Alcon Wavelight FS200 in the first group, Moria M2 90 mechanical microkeratome in the second group between December 2017 and August 2018. The study included 3 males (15%) and 17 females (85%) in FS-LASIK group and 12 males (60%) and 8 females (40%) in microkeratome group. Ninety percent of the first group study subjects were myopes, 10% were hyperopes, however, in the second group 80% were myopes and 20% hyperopes (Table 1).
 | Table 1 Distribution of gender and refractive error in both groups |
The study subjects had a mean preoperative manifest refraction spherical equivalent range from (−6.50 to +3.25) diopters in the femtoLASIK group and from (−4.35 to +3.00) diopters in the microkeratome group (Table 2).
 | Table 2 Deviation of the achieved side-cut angle angle from the intended angle in both groups |
After measuring the side-cut angle of both groups, femtoLASIK group intended side-cut angle was around 110–115° and the mean achieved side-cut angle result was 134.75° with a range of 110–155° with a standard deviation from the intended angle 12.56°. The microkeratome group intended side-cut angle was 70° and the mean achieved side-cut angle result is 44.35°, with a range of 30–65° with a standard deviation from the intended angle 10.31° (Table 2, Figures 1 and 2).
 | Figure 1 Statistically significant difference in achieving the intended side-cut angle with P-value <0.01 in both groups. Abbreviaton: femtoLASIK, femtosecond laser-assisted in situ keratomileusis. |
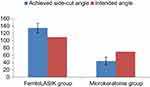 | Figure 2 Intended versus the achieved angle in both groups. Abbreviation: femtoLASIK, femtosecond laser-assisted in situ keratomileusis. |
In the femtoLASIK group the mean deviation from the intended angle 24.75°, minimum angle of deviation was (0°) and maximum angle was 45°, but in the microkeratome group the mean angle of deviation from the intended angle was −25.65°, minimum angle was (−40°) and maximum angle (−5°). (Figure 3)
 | Figure 3 Deviation of the achieved side-cut angle from the intended angle (P-value<0.01). Abbreviation: femtoLASIK, femtosecond laser-assisted in situ keratomileusis. |
The study correlation between the deviation of the side-cut angle from the intended angle with the degree of myopia in each group (myopic patients only) revealed no significant correlation between degree of myopia and deviation from intended angle (Table 3).
 | Table 3 Correlate degree of myopia with the deviation from the intended angle in both groups |
Discussion
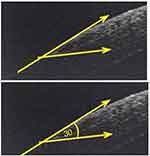
Advances in instrumentation of LASIK surgery, such as the introduction of femtosecond laser technology for flap creation, have improved the predictability of creating flaps and safety profile of LASIK surgery.5–7 Femtosecond lasers are capable of creating more predictable and desirable side-cut profiles. The side-cut angle range varies with different laser manufacturers, but vertical, near-vertical, or reverse beveled angles can be created.8
In our study, we measured and verified both the intended and the achieved LASIK flap side-cut angle in 40 eyes divided on two groups, first group (20 eyes) done by femtosecond LASIK with side-cut angle designed to be inverted, second group (20 eyes) done by conventional microkeratome with acute side-cut angle. Two weeks postoperatively LASIK flap side-cut angle was measured using the anterior segment OCT .
To our knowledge this is the first study to evaluate such outcomes.
In the femtoLASIK group, patients underwent FS-LASIK using Wavelight FS-200, we found that the measured flap side-cut angles were not only inverted in 100% of cases, with a minimum angle measure of 110° (the intended angle) and maximum measure of 155°, unlike the microkeratome group patients who underwent LASIK using the conventional microkeratome, we found that all flap side-cut angles were more acute than the intended angle (70°) in 100% of cases with a minimum angle 30° and maximum angle of 65° (Figures 4–7).
 | Figure 4 Microkeratome LASIK flap with acute side-cut angle 30°. Abbreviation: LASIK, laser-assisted in situ keratomileusis. |
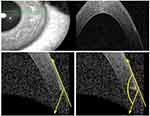 | Figure 7 FemtoLASIK flap with a very large inverted angle (155°). Abbreviation: femtoLASIK, femtosecond laser-assisted in situ keratomileusis. |
Knorz et al compared the adhesion and the strength of flaps created with a mechanical microkeratomes and IntraLase® (Johnson and Johnson surgical Vision, Irvine, CA, USA) femtosecond laser with a different side-cut angle. Flap adhesion strength was measured 75 days after surgery with a tension meter to dehisce the flap. They found that the differences between the microkeratome group and all IntraLase femtosecond laser groups were highly significant and the differences between the acute and inverted side-cut angles in femtoLASIK groups were statistically significant and the flap adhesion is significantly stronger in femtosecond laser group than the mechanical microketaome and an inverted side cut increases flap adhesions significantly compared with a standard side cut.4
In our study the mean side-cut angle measured in the femtoLASIK group was 134.75° with a mean positive deviation 24.75° from the intended angle, unlike the microkeratome group, the mean side cut-angle was 44.35° with a mean negative deviation of −25.65°.
Chen et al and his colleagues did a meta-analysis study of existing comparative studies supporting the outcome of the inverted side-cut angle done by the femtoLASIK, using IntraLase femtosecond laser and mechanical microkeratomes for flap creation in LASIK to evaluate the safety, efficacy, and predictability of IntraLase femtosecond laser-assisted compared to microkeratome-assisted LASIK. No significant differences were identified between the two groups in regard to a loss of two lines of best corrected visual acuity (BCVA), patients achieving uncorrected visual acuity (UCVA) 20/20 or better, final UCVA, final astigmatism, or changes in higher order aberrations (HOAs). The IntraLase group had more patients who were within 0.50 diopters of target refraction compared to the microkeratome group, and flap thickness was more predictable in the IntraLase group. The microkeratome group had more epithelial defects, whereas the IntraLase group had more cases of diffuse lamellar keratitis.9
Our study demonstrates well that all side-cut angles done by femtoLASIK were more obtuse than intended in almost all the patients done .
Kung et al did a prospective, comparative, fellow-eye study of 120 eyes in 60 participants who underwent femtosecond-assisted myopic LASIK to evaluate the effect of inverted side-cut LASIK flap architecture on corneal sensation and self-reported dry eye symptoms compared with a conventional side cut. LASIK flaps were created with a 70° side cut using the 60 kHz IntraLase FS or a 130° inverted side cut using the 150 kHz IntraLase IFS. Programmed flap parameters were a 9 mm diameter with a superior hinge and a 105 mm flap depth. Cochet–Bonnet was used to quantitatively measure corneal sensation before LASIK and at postoperative months 1, 3, 6, and 12, they found that corneal sensations are better in the inverted side-cut group compared with the conventional group at postoperative months 3, 6, and 12. The study subjects completed a dry eye survey modeled after the validated, linear-scaled quality of vision questionnaire. The survey was administered preoperatively and at postoperative months 1, 3, 6, and 12. Regarding light sensitivity, dryness, foreign body sensation, pain and discomfort at 12 months were equal or better in eyes with an inverted side cut compared with eyes with a conventional side cut, but these differences were not statistically significant.10
Another study done by Knox et al proved that the side-cut angle affected the corneal biomechanics after flap creation. The study was done to evaluate the corneal biomechanical effects of varying LASIK flap depth and side cut angulations and the relative contribution of the lamellar and side cuts using a femtosecond laser and radial shearing speckle pattern interferometry (RSSPI). They found that angulated side cuts improved the structural integrity of the flap; mechanical strain on the wound decreased from 12% in a 30° side cut to 5% in a 90° conventional side cut and to only 2% in a 150° inverted side cut. Light microscopy of these corneas 1 week after femtosecond flap creation revealed less wound gape and fewer activated keratocytes with an inverted 135° compared with a 90° side cut. with a conclusion that vertical side cuts through corneal lamellae rather than horizontal delamination incisions contribute to the loss of structural integrity during LASIK flap creation. Angulating side cuts such that the stromal diameter of the flap exceeds its epithelial diameter can decrease this effect.11
Conclusion
In conclusion, we found that The femtoLASIK technology capable of making the flap side-cut angle more obtuse than the intended angle, unlike the achieved flap side-cut angle done using the mechanical microkeratome which will provide a greater flap strength and adherence. We recommend a larger sample size with comparison of side-cut angle among different refractive errors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Moshirfar M, Gardiner JP, Schliesser JA, et al. Laser in situ keratomileusis flap complications using mechanical microkeratome versus femtosecond laser: retrospective comparison. J Cataract Refract Surg. 2010;36(11):1925–1933. doi:10.1016/j.jcrs.2010.05.027
2. Chao C, Golebiowski B, Stapleton F. The role of corneal innervation in lasik-induced neuropathic dry eye. Ocul Surf. 2014;12(1):32–45. doi:10.1016/j.jtos.2013.09.001
3. De Paiva CS, Chen Z, Koch DD, et al. The incidence and risk factors for developing dry eye after myopic LASIK. Am J Ophthalmol. 2006;141(3):438–445. doi:10.1016/j.ajo.2005.10.006
4. Knorz MC, Vossmerbaeumer U. Comparison of flap adhesion strength using the Amadeus microkeratome and the IntraLase iFS femtosecond laser in rabbits. J Refract Surg. 2008;24(9):875–878.
5. Kezirian GM, Stonecipher KG. Comparison of the IntraLase femtosecond laser and mechanical keratomes for laser in situ keratomileusis. J Cataract Refract Surg. 2004;30(4):804–811. doi:10.1016/j.jcrs.2003.10.026
6. Letko E, Price MO, Price FW. Influence of original flap creation method on incidence of epithelial ingrowth after LASIK retreatment. J Refract Surg. 2009;25(11):1039–1041. doi:10.3928/1081597X-20090617-13
7. Santhiago MR, Kara-Junior N, Waring GO. Microkeratome versus femtosecond flaps: accuracy and complications. Curr Opin Ophthalmol. 2014;25(4):270–274. doi:10.1097/ICU.0000000000000070
8. Feder RS. The LASIK Handbook a case-based approach. Lippincott Williams & Wilkins, a Wolters Kluwer busniness; Philadelphia, PA, USA: 2013:56–57.
9. Chen S, Feng Y, Stojanovic A, Jankov MR, Wang Q. IntraLase Femtosecond Laser vs Mechanical Microkeratomes in LASIK for Myopia: a Systematic Review and Meta-analysis. J Refract Surg. 2012;28(1):15–24. doi:10.3928/1081597X-20111228-02
10. Kung JS, Sáles CS, Manche EE. Corneal sensation and dry eye symptoms after conventional versus inverted side-cut femtosecond LASIK: a prospective randomized study. Ophthalmology. 2014;121(12):2311–2316. doi:10.1016/j.ophtha.2014.07.015
11. Knox Cartwright NE, Tyrer JR, Jaycock PD, Marshall J. Effects of variation in depth and side cut angulations in lasik and thin-flap LASIK using a femtosecond laser: a biomechanical study. J Refract Surg. 2012;28(6):419–425. doi:10.3928/1081597X-20120518-07
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
