Back to Journals » Research and Reports in Urology » Volume 8
Vasectomy and prostate cancer risk: a historical synopsis of undulating false causality
Authors Nutt M, Reed Z, Kohler T
Received 20 February 2016
Accepted for publication 19 April 2016
Published 18 July 2016 Volume 2016:8 Pages 85—93
DOI https://doi.org/10.2147/RRU.S71325
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Jan Colli
Max Nutt, Zachary Reed, Tobias S Köhler
Division of Urology, Southern Illinois University School of Medicine, Urology, Springfield, IL, USA
Abstract: The potential influence of vasectomy being a risk factor for the development of prostate cancer is not a new concept, with more than 30 publications addressing the topic. Given the global frequency of vasectomy and the prevalence of prostate cancer, this subject justifiably deserves scrutiny. Several articles have claimed that vasectomy puts men at risk for future development of prostate cancer. We explore articles that have shown the contrary (no link), explore the studies’ strengths and weaknesses, describe possible prostate cancer pathophysiologic mechanisms, and apply Bradford Hill criteria to help discern correlation with causation. The risk and interest of association of prostate cancer with vasectomy has waxed and waned over the last three decades. Based on our review, vasectomy remains a safe form of sterilization and does not increase prostate cancer risk.
Keywords: vasectomy, prostate cancer, pathophysiology
Introduction
It is important for couples to consider the use of contraception in order to optimize family size, allowing them to minimize the financial burdens of additional children. Contraception also plays a pivotal role in public health by decreasing the fertility rate, thus minimizing the ever increasing world population. Among the various forms of contraception, vasectomy is the fourth most widely used option,1 following oral contraceptives, tubal ligation, and condoms.
With a prevalence as high as 15% among US male population and with an estimated 175,000–354,000 vasectomies performed annually in the US,1 vasectomy remains an important medical intervention in the 21st century. When such a large portion of our population is undergoing a treatment/procedure, it is important to investigate the relationship between the agent and any potential risks to health. Application of the Bradford Hill criteria is an excellent method to help discern correlation with causation.
The potential influence of vasectomy on prostate cancer risk is not new with more than 30 publications addressing the topic. The design, specific strengths, and limitations of these studies are reviewed in this article. An article published in 2014 has spurred renewed interest into this debate, and its merits and limitations are thoroughly discussed. An understanding of the proposed mechanisms that could potentially link vasectomy to prostate cancer is important. We performed a thorough literature search using PubMed with the terms vasectomy and prostate cancer and found 29 original studies on the subject and several other review articles. Ultimately, after reviewing the literature, we agree with the overwhelming consensus adopted by the American Urologic Association. In 2015, the American Urologic Association stated in its guidelines on vasectomy that the procedure is not a risk factor for prostate cancer. In position 3 of the vasectomy guidelines “Clinicians do not need to routinely discuss prostate cancer, coronary heart disease, stroke, hypertension, dementia or testicular cancer in pre-vasectomy counseling of patients because vasectomy is not a risk factor for these conditions” (Standard [Evidence Strength Grade B]).
Lessons learned from other conditions linked to vasectomy
Vasectomy has been falsely indicted to cause various conditions from testicular cancer to heart disease, and even dementia. These accusations have largely been debunked and discredited and merit-reviewed to remind us of potential study design flaws.
An association between vasectomy and cardiovascular disease was first alluded to by Clarkson and Alexander. Their 19782 and 19803 studies on Macaca fascicularis and Macaca mulatta monkeys demonstrated that vasectomized male monkeys underwent more extensive atherosclerosis than did age-matched controls. Upon further studies on monkeys,4,5 investigators, including Clarkson and Alexander, were unable to reproduce concordant results and ultimately concluded that vasectomy did not lead to an increase in atherosclerosis. Studies on humans investigating an association between vasectomy and cardiovascular disease soon followed. The results of these studies failed to show any association between vasectomy and an increased incidence of cardiovascular disease,6–8 mortality from cardiovascular disease,9 myocardial infarction,10,11 coronary revascularization procedures,12 stroke,12 or high blood pressure.12
A 1988 case–control by Strader et al13 was the first study to find a relationship between vasectomy and testicular cancer. Upon further review, it was elicited that the link existed only among Catholic men within the study. The association is thought to be present due to an underreporting bias of Catholic controls who were less likely to report having undergone vasectomy than were Catholic men who had received a diagnosis of testicular cancer. A 1988 case–control study from Ireland by Thornhill et al14 and a 1990 study from Scotland by Cale et al15 found an association between vasectomy and testicular cancer. The studies reviewed cases of testicular cancer from their respective regions and found three and eight cases in men who had received a vasectomy. Due to the small power of these studies, further investigation of this association was necessary. In 1994, Moller et al16 performed a cohort study on 73,917 Danish men who had received a vasectomy. Ultimately, this study failed to demonstrate an increased incidence of testicular cancer among men who had received vasectomy. Another study was performed in 1994 by the UK Testicular Cancer Study Group,17 which looked at 794 men from England and Wales who had been diagnosed with testicular cancer. Once again, this study was unable to find any association between vasectomy and testicular cancer. The high power of the 1994 studies allows us to say with relative certainty that there is no association between vasectomy and testicular cancer.
One case–control study and a single case report have been published in recent years concerning an association between vasectomy and primary progressive aphasia (PPA), a rare form of frontotemporal dementia. The case–control study from 2006 by Weintraub et al18 compared 47 men who had been diagnosed with PPA with 57 age-matched controls with no cognitive impairment. The age-adjusted rate of vasectomy in men with PPA (40%) was higher than that of the control group (16%), with a P-value of 0.02. Also, the vasectomized men with PPA had a younger age of onset than did the nonvasectomized men with PPA (58.8 years vs 62.9, P=0.03). The case study published in 2008 by Decker et al was about a man who had received a vasectomy 25 years previous to a diagnosis of PPA, which responded in 4 weeks to a brief therapy of prednisone.19 Because of the steroid-responsive nature of the disease, authors speculated on an autoimmune mechanism. In order to determine the validity of a possible association between vasectomy and the rare form of dementia, further studies with high power must be undertaken. A brief overview of many of the studies investigating relationships between vasectomy and cardiovascular disease, testicular cancer, and PPA are listed in Table 1.
Basic science: inflammation/hormonal changes as cause for the development of cancer of the prostate
Prostate cancer, the most common solid tumor diagnosed in adult men, will be diagnosed in an estimated 16% of adult men during their lifetime. It takes ∼30,000 US male lives each year.20 The etiology of prostate cancer is not entirely clear, but accepted risk factors include advanced age, family history, African American ancestry, and living in western civilization.21 Chronic prostatic inflammation has been implicated as another possible risk factor.
Past authors have speculated on pathophysiologic mechanisms that link vasectomy with prostate cancer. Altered hormone levels, immunologic processes, prostate size, and volume of secretions have been implicated as potential causes for a theorized increased risk of prostate cancer in vasectomized men.
The first study to find a link between vasectomy and prostate cancer by Honda et al24 hypothesized that the connection was a result of a change in circulating androgens secondary to vasectomy. A few studies since then have failed to prove that correlation. A 1995 Chinese study of 91 pairs of men found that men who received vasectomy in the past 10–19 years had higher serum concentration of dihydrotestosterone than age-matched controls. They had similar levels of serum testosterone, luteinizing hormone, and follicle-stimulating hormone. This study also found that those who received vasectomy >20 years ago had a higher serum testosterone than did men who had not.23 The authors of this study did not find an increased risk of prostate cancer in the men who underwent vasectomy, but they reported that their results “indirectly supported” the hypothesis. In a review of possible biological mechanisms linking vasectomy with prostate cancer, Howards24 wrote that the majority of the studies he reviewed showed no change in endocrine parameters following vasectomy.
It is obvious that some immunologic processes occur as a result of vasectomy, but their tie to the development of prostate cancer remains unclear. Past studies have assessed the development of antisperm antibodies as a result of vasectomy. One study found that 74% of vasectomized men developed serum antisperm antibody activity, while 0% of nonvasectomized men had serum antisperm antibody activity.25 A relationship between antisperm antibody activity and testicular histology changes was assessed in the same study, and any association was not statistically significant. Although speculation exists about further immune complex formation that could lead to the development of prostate dysplasia and prostate carcinoma, this review of the literature was unable to identify evidence of any such complex.
In a study on rats published in 1975, investigators discovered that unilateral rat vasectomy results in reduced volume, RNA polymerase activity, and DNA content of the ipsilateral prostate lobe.26 A study published in 1988 by Jakobson et al27 investigated the relationship between vasectomy, prostate size, and volume of prostatic secretions. They found that men who underwent vasectomy had a reduction in size of the peripheral zone of the prostate, as well as a permanently reduced volume of prostatic secretions. Isaacs28 hypothesized that a reduction in prostatic secretion volume may lead to a prolonged exposure of the prostate gland to certain carcinogenic factors present in the secretions. It has also been postulated that by decreasing the flow of testicular and epididymal fluids to the prostate, vasectomy could lead to a decreased flow of local immune factors, such as lymphocyte-activated killer cells to the prostate. Since lymphocyte-activated killer cells could be helpful in preventing prostate cancer, decreasing their access to the prostate could theoretically increase the risk of prostate cancer.25
Although they cannot be completely debunked, it is highly unlikely that any of the previously discussed biologic mechanisms have any merit as a pathophysiologic mechanism linking vasectomy and prostate cancer. Further investigation into a biologic association is necessary to warrant further studies on this topic.
History of original articles discussing prostate cancer and vasectomy
The first association between prostate cancer and vasectomy was reported by Honda et al24 in a population-based case–control study in 1988. They found that the risk of prostate cancer was higher in men who had been vasectomized, and this risk increased with the number of years since vasectomy (the relative risk [RR] for prostate cancer 30 years after vasectomy was 4.4). They hypothesized that this increased risk could be due to hormonal changes in vasectomized men. The study found that vasectomized men had higher levels of testosterone than those who had not had a vasectomy, but this association was small. Of note, historically higher levels of testosterone were thought to be causes of prostate cancer. However, there is no evidence to support this notion. Furthermore, no evidence exists showing that vasectomy causes changes in hormonal profiles. One possibility is that men with higher levels of sexual activity could be more likely to choose to have a vasectomy, and their increased sexual activity could be related to increased levels of circulating androgens. The reported association between vasectomy and increased risk of prostate cancer in this study is likely to be noncausal, and it warrants further research.
The positive association between vasectomy and prostate cancer found by Honda et al triggered an increased interest in this area of research. In the 5 years following, nine studies were conducted that reported results on the relationship between vasectomy and prostate cancer. In 1989, Newell et al29 found no link between vasectomy and an increased risk of prostate cancer, contradicting the results of Honda et al. However, in 1990, Mettlin et al30 and Rosenberg et al31 reported positive associations between vasectomy and prostate cancer, supporting the initial study done by Honda et al. The correlation reported by Mettlin et al was small, and it was only reported for men who had a vasectomy 13–18 years before diagnosis. There was no such positive result for men who had a vasectomy 5–12 years or 19–44 years before the diagnosis of prostate cancer. In 1991, Sidney et al32 performed a large cohort study that reported no association between prostate cancer and vasectomy at all, while in the same year, Spitz et al33 found a slight positive association between the two in their case–control study. Two more studies in 1992 by Nienhuis et al34 and Peterson et al35 reported that vasectomy does not increase the risk of prostate cancer.
Giovannucci et al36 found a significant correlation between vasectomy and prostate cancer risk in 1993. They performed a prospective cohort study of US men, all health professionals, between 1986 and 1990. The study found that vasectomy was associated with an increased risk of prostate cancer (RR =1.56). The RR was even higher (1.85) for individuals who had a vasectomy >22 years back, though this relationship was weaker than the one reported in Honda et al’s study. This study controlled for the diet, level of physical activity, smoking, alcohol consumption, education level, body mass index (BMI), and geographic area of residence. It was suggested that a change in prostatic function following vasectomy is the major risk factor for the development of prostate cancer; however, this could not be proven. The possibility of confounding and bias cannot be eliminated in this study. The same year, Hayes et al37 performed a case–control study on two separate populations, US whites and US blacks. This study reported no increased risk of prostate cancer with vasectomy for either racial group.
In 1994, Hsing et al38 performed a case–control study of Chinese men that ultimately reported an increased risk of prostate cancer in men who had undergone vasectomy. They did report that detection bias was of concern. In the same year, three studies reported contradicting results. Moller et al,19 Hiatt et al,39 and Rosenberg et al40 reported no association between prostate cancer and vasectomy in their 1994 studies. Rosenberg et al had previously reported a positive correlation in 1990; however, they reassessed these results with new data that found no relationship between prostate cancer and vasectomy. This reversal of findings suggested that the results reported in the 1990 study were due to chance. A year later, in 1995, John et al41 also found no link between prostate cancer and vasectomy in their case–control study.
Zhu et al42 performed a population-based case–control study of men in the Group Health Cooperative of Puget Sound in 1996. They used mailed questionnaires and medical records to collect data on vasectomy status, potential confounding variables, and factors related to detection of prostate cancer, such as hospitalization, routine physical examination, digital rectal exam, and prostate ultrasound. Potential confounding variables analyzed were marital status, race, religion, occupation, education, income, children, tobacco use, alcohol use, physical activity, BMI, and history of genitourinary diseases, sexually transmitted infection, and cancers (specifically prostate cancer). Overall, they reported no association between prostate cancer and vasectomy, age at vasectomy, or time since vasectomy. There did seem to be a positive association between risk of prostate cancer and vasectomized men with a positive family history of prostate cancer. This could be due to detection bias, that is, an increase in screening for prostate cancer in vasectomized men with a family history. In the same year, Ewings and Bowie43 and Andersson et al44 performed case–control studies of several risk factors for prostate cancer, one being vasectomy. While Andersson et al did find a positive association between the two, it was not the main factor tested, and the group tested was small, making these results weaker. Ewings and Bowie found no link between vasectomy and prostate cancer, but again, this study was small, and vasectomy was not the only risk factor tested.
In 1997, Platz et al45 performed a case–control study of Indian men to determine if there was an association between vasectomy and prostate cancer. Their results suggested a slightly increased risk of prostate cancer in men who had had a vasectomy; however, the data were not statistically significant, and the relationship was determined to be noncausal. The same year, DeAntoni et al46 performed a large cohort study that ultimately found no association between prostate cancer and vasectomy. These results were supported by a study of Lesko et al47 in 1999, who performed a case–control study that reported no correlation at all between prostate cancer and vasectomy.
Also in 1999, Stanford et al48 performed a population-based case–control study of men aged 40–64 years in King County, Washington. Information was collected from 753 men with prostate cancer and 703 controls without prostate cancer. Variables examined in this study include age at reference date, race, family history of prostate cancer, marital status, income, education, religious preference, smoking history, alcohol use, BMI, sexual history, history of benign prostatic hyperplasia >2 years before reference date, detailed screening measures for prostate cancer, and dietary intake of total fat, saturated fat, lycopene, and beta-carotene. The study suggests that vasectomized men are more likely to present earlier in the course of the disease indicating a higher intensity of screening in vasectomized men. However, no evidence was found that linked vasectomy status, age at vasectomy, or time since vasectomy to the development of prostate cancer.
In 2001, Emard et al49 reported an increased risk of prostate cancer in men who had undergone vasectomy. However, this study was limited to birth cohorts between the years of 1925 and 1939. The authors also report a possibility of detection bias within the study. A year later, in 2002, Lynge50 performed a cohort study of Danish men in which all data were collected from a registry to minimize the reporting bias. They found no significant data suggesting an increased risk of prostate cancer in vasectomized men. In the same year, Cox et al51 performed a population-based case–control study of New Zealand men to determine the RR of prostate cancer in men who had had a vasectomy vs those who had not. New Zealand has the highest prevalence of vasectomy of any country at 23% of men. A total of 923 cases and 1,224 controls were selected for the study. Because of New Zealand’s high prevalence of vasectomy and the large number of cases and controls, this would be one of the strongest studies to date. The results reported no correlation between prostate cancer and vasectomy (RR =0.92, P>0.05). Time since vasectomy also did not correlate with prostate cancer. Overall, this study concluded that vasectomy does not increase the risk of prostate cancer, even after >25 years.
Rohrmann et al52 performed a prospective cohort study of Maryland men in 2005. The results of their study showed a statistically significant positive association between prostate cancer and vasectomy. This association was only found with low-grade disease, and men who had a vasectomy after 40 years were at a higher risk overall. However, it was also found that men who had had a vasectomy were more likely to have been screened for prostate cancer, introducing potential selection bias.
Holt et al53 analyzed a population-based case–control study addressing this issue in 2008. Cases of confirmed prostate cancer between January 1, 2002, and December 31, 2005, were used as well as a control group. This study found that the prevalence of vasectomy was similar in both cases of prostate cancer and the control group (36.2% and 36.1%, respectively), indicating no association between prostate cancer and vasectomy status. They also reported no association between prostate cancer and age at vasectomy or time since vasectomy. Because only 14.4% of the controls had not had prostate specific antigen or DRE screening in the past 5 years, misclassification bias was unlikely. Similarly, in 2012, Romero et al54 found no association between prostate cancer and vasectomy in their cohort study of Brazilian men. The study was small, and it focused on other factors, but no data that support a relationship between vasectomy and prostate cancer were reported.
Renewed interest in the vasectomy and prostate cancer link
More recently, in 2014, Siddiqui et al55 examined the relationship between vasectomy and prostate cancer through a 24-year follow-up study, which renewed the interest in this issue. This was the largest cohort study with the longest follow-up time to date. The study suggested that there was a small increased risk of prostate cancer in vasectomized men. Vasectomy was associated with an increased risk of high-grade or lethal disease, and there was no association between vasectomy and low-grade or localized disease. This study focused on advanced and lethal prostate cancer to reduce the potential for detection (screening) bias. The authors considered several variables, including race, height, BMI, physical activity, smoking, diabetes, family history of prostate cancer, PSA testing, multivitamin use/vitamin E supplementation, and alcohol use. They found that vasectomized men were more likely to be white, drink alcohol, and take multivitamins, and they also reported more PSA testing than men without vasectomy. The authors also measured the serum levels of sex hormones in 663 men without prostate cancer, and there were no significant hormone level differences between men with and men without a vasectomy.
A year later, in 2015, Sokal et al56 wrote a response to the 2014 Siddiqui et al study pointing out several flaws. In comparison to another report using the Health Professions Follow-Up Study,36 the authors found inconsistencies. First, the updated 2014 study did not report loss to follow-up among the 49,405 men over the 24-year period. This missing data that were not discussed may have biased the results. The 2014 study also only met one of the nine Bradford Hill criteria for a causal relationship: temporality. Possible confounding variables, such as finasteride use, which is associated with an increased detection of high-grade prostate cancer, and lycopene intake, which has shown a protective effect against prostate cancer, were not analyzed or discussed. Finally, the unadjusted data of the 2014 study suggest that vasectomized men are not at a higher risk but at a lower risk of developing lethal or high-grade prostate cancer.
Review articles discussing vasectomy and prostate cancer
In 1997, McDonald57 wrote a review article that discusses the potential health risks of vasectomy. He states that although studies have been done suggesting that vasectomy is linked to an increased risk of cardiovascular disease, testicular cancer, and prostate cancer, it is not proven, and more recent studies have indicated that there is no association between vasectomy and these diseases. McDonald suggests that the only negative side effects of vasectomy are sterility (due to the limited reversibility of the procedure) and mild scrotal pain that may persist. Patients should be advised that it is frequently not possible to reverse a vasectomy. The author states that any other health scares involving vasectomy are without foundation.
In 2002, Dennis et al58 performed a quantitative review of 22 prostate cancer studies to determine the estimated RR between prostate cancer and vasectomy status. In this analysis of five cohort studies and 17 case–control studies between the years of 1983 and 2001, a small but statistically significant association between vasectomy status and prostate cancer was found. This analysis also found that the risk for prostate cancer increases by 10% for each additional 10 years since vasectomy with an RR of 1.32 for 30 years post-vasectomy. Overall, the study suggests that men with a prior vasectomy may be at an increased risk of prostate cancer, but vasectomy is most likely not causal because potential bias was not ruled out in this analysis.
Most recently, in 2015, Shang et al59 performed a meta-analysis of ten cohort studies involving 7,027 cases and 429,914 participants to determine if there was a positive association between prostate cancer and vasectomy. They used only cohort studies to avoid the selection and recall bias as well as the smaller sample sizes of case–control studies. Overall, the study suggested that vasectomy is not associated with an increased risk of prostate cancer. Of the ten studies, three studies showed a positive association, all of which were in American men. In these three studies, the men who underwent a vasectomy may have been more likely to return for prostate cancer screening, leading to a detection bias; this variable must be considered. Unmeasured factors and residual confounders, such as long-term aspirin use, must be considered as this could decrease risk for prostate cancer. Due to the lack of numerous studies with strong evidence of an association between vasectomy and prostate cancer, it is highly unlikely that any causal association exists. Table 2 summarizes all prostate cancer studies.
  | Table 2 Summary of the associations between vasectomy and prostate cancer over the years Abbreviations: OR, odds ratio; RR, relative risk. |
Putting it all together
Over the years, conflicting data on the relationship between prostate cancer and vasectomy have caused much concern as well as interest in this area of research. It is interesting to note the waxing and waning nature of anxiety and published literature on this topic (Figure 1). While most studies showed no association between prostate cancer and vasectomy, there were several years of increased concern due to studies that reported positive results. Ultimately all relevant literature was pooled in the review article by Shang et al63 including an N of 429,914 that showed no association between prostate cancer and vasectomy.
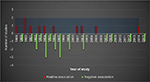  | Figure 1 Summary of the associations between vasectomy and prostate cancer over the years. |
The Bradford Hill criteria for causation are a group of criteria that are necessary to suggest evidence of causal relationship between an incidence and a consequence, in this case the incidence being vasectomy and the consequence being prostate cancer. These nine criteria are widely accepted as a method in determining causality between two variables. In the studies that report a positive correlation between vasectomy and prostate cancer, the only criterion that is met is temporality. In other words, the fact that vasectomy preceded the diagnosis of prostate cancer in these studies means that they meet the requirement for temporality. However, these studies fail to meet any of the eight other criteria for causality. These other criteria include strength of association, consistency, theoretical plausibility, coherence, specificity in the causes, dose–response relationship, experimental evidence, and analogy. The association reported between vasectomy and prostate cancer is not strong, nor is it consistent. There are many studies that contradict the results, reporting no association between the two. In the studies that do show a positive association between vasectomy and prostate cancer, the exact physiologic mechanism is unclear, and there is no theory that is widely accepted to explain how vasectomy would cause prostate cancer. Therefore, using the Bradford Hill criteria, one cannot conclude that vasectomy causes prostate cancer based on the presented research.
Conclusion
Vasectomy is a popular birth control procedure among men, and with prostate cancer being one of the most prevalent cancers in males, it is important to identify any causal relationship between vasectomy and prostate cancer. Although some researchers have reported a link between vasectomy and prostate cancer in the past, there is not enough supporting evidence to indicate a causal relationship between the two. Analysis of the methods used in these studies shows a potential for bias and confounding, which could explain some of the positive associations reported. More recent studies, which control for additional variables and contain larger sample sizes, report no association between vasectomy and prostate cancer. The research on this issue has been a topic of interest for years now, yet there remains no consistent evidence linking vasectomy to prostate cancer, nor are there any widely accepted theories as to how vasectomy would cause prostate cancer. Overall, the lack of sufficient evidence over the years allows us to come to the conclusion that vasectomy is not a risk factor in the development of prostate cancer. It remains a safe and effective form of birth control with minimal side effects, and any man who is considering having vasectomy should not be discouraged by reports of its association with prostate cancer. We still deem vasectomy as the safest form of surgical sterilization.
Disclosure
The authors report no conflicts of interest in this work.
References
Eisenberg ML, Lipshultz LI. Estimating the number of vasectomies performed annually in the United States: data from the National Survey of Family Growth. Urology. 2010;184(5):2068–2072. | ||
Alexander NJ, Clarkson TB. Vasectomy increases the severity of diet-induced atherosclerosis in Macaca fascicularis. Science. 1978;201(4355):538–541. | ||
Clarkson TB, Alexander NJ. Long-term vasectomy: effects on the occurrence and extent of atherosclerosis in rhesus monkeys. J Clin Invest. 1980;65(1):15–25. | ||
Lauersen NH, Muchmore E, Shulman S, et al. Vasectomy and atherosclerosis in Macaca fascicularis: new findings in a controversial issue. J Reprod Med. 1983;28(11):750–758. | ||
Clarkson TB, Alexander NJ, Morgan TM. Atherosclerosis of cynomolgus monkeys hyper- and hyporesponsive to dietary cholesterol, lack of effect of vasectomy. Arteriosclerosis. 1988;8(5):488–498. | ||
Goldacre MJ, Holford TR, Vessey MP. Cardiovascular disease and vasectomy: findings from two epidemiologic studies. N Engl J Med. 1983;308(14):805–808. | ||
Perrin EB, Woods JS, Namekata T, Yagi J, Bruce RA, Hofer V. Long-term effect of vasectomy on coronary heart disease. Am J Public Health. 1984;74(2):128–132. | ||
Goldacre MJ, Wotton CJ, Seagroatt V, Yeates D. Cancer and cardiovascular disease after vasectomy: an epidemiological database study. Fertil Steril. 2005;84(5):1438–1443. | ||
Giovannucci E, Tosteson TD, Speizer FE, Vessey MP, Colditz GA. A long-term study of mortality in men who have undergone vasectomy. N Engl J Med. 1992;326(21):1392–1398. | ||
Rosenberg L, Schwingl PJ, Kaufman DW, Helmrich SP, Palmer JR, Shapiro S. The risk of myocardial infarction 10 or more years after vasectomy in men under 55 years of age. Am J Epidemiology. 1986;123(6):1049–1056. | ||
Manson JE, Ridker PM, Spelsberg A, Ajani U, Lotufo PA, Hennekens CH. Vasectomy and subsequent cardiovascular disease in US physicians. Contraception. 1999;59(3):181–186. | ||
Alexander NJ, Senner JW, Hoch EJ. Evaluation of blood pressure in vasectomized and nonvasectomized men. Int J Epidemiol. 1981;10(3):217–222. | ||
Strader CH, Weiss NS, Daling JR. Vasectomy and the incidence of testicular cancer. Am J Epidemiol. 1988;128(1):56–63. | ||
Thornhill JA, Conroy RM, Kelly DG, Walsh A, Fennelly JJ, Fitzpatrick JM. An evaluation of predisposing factors for testis cancer in Ireland. Eur Urol. 1988;14(6):429–433. | ||
Cale AR, Farouk M, Prescott RJ, et al. Does vasectomy accelerate testicular tumour? Importance of testicular examinations before and after vasectomy. BMJ. 1990;300(6721):370. | ||
Moller H, Knudsen LB, Lynge E. Risk of testicular cancer after vasectomy: cohort study of over 73,000 men. BMJ. 1994;309(6950):295–299. | ||
Aetiology of testicular cancer. Association with congenital abnormalities, age at puberty, infertility, and exercise. United Kingdom Testicular Cancer Study Group. BMJ. 1994;308(6941):1393–1399. | ||
Weintraub S, Fahey C, Johnson N, et al. Vasectomy in men with primary progressive aphasia. Cogn Behav Neurol. 2006;19(4):190–193. | ||
Decker DA, Heilman KM. Steroid treatment of primary progressive aphasia. Arch Neurol. 2008;65(11):1533–1535. | ||
Siegel R, Miller KD, Jemal A. Cancer statistics 2016. CA Cancer J Clin. 2016;66(1):7–30. | ||
Sfanos KS, De Marzo AM. Prostate cancer and inflammation: the evidence. Histopathology. 2012;60(1):199–215. | ||
Honda G, Bernstein L, Ross R, Greenland S, Gerkins V, Henderson B. Vasectomy, cigarette smoking, and age at first sexual intercourse as risk factors for prostate cancer in middle- aged men. Br J Cancer. 1988;57(3):326–331. | ||
Mo ZN, Huang X, Zhang SC, Yang JR. Early and late long-term effects of vasectomy on serum testosterone, dihydrotestosterone, luteinizing hormone and follicle-stimulating hormone levels. J Urol. 1995;154(6):2065–2069. | ||
Honda G, Bernstein L, Ross R, Greenland S, Gerkins V, Henderson B. Vasectomy, cigarette smoking, and age at first sexual intercourse as risk factors for prostate cancer in middle- aged men. Br J Cancer. 1988;57(3):326–331. | ||
Jarow JP, Goluboff ET, Chang TS, Marshall FF. Relationship between antisperm antibodies and testicular histologic changes in humans after vasectomy. Urology. 1994;43(4):521–524. | ||
Pierrepoint CG, Davies P, Lewis NH, Moffat DB. Examination of the hypothesis that a direct control system exists for the prostate and seminal vesicles. J Reprod Fertil. 1975;44(2):395–409. | ||
Jakobson H, Torp-Pederson S, Juul N, Hald T. The long-term influence of vasectomy on prostatic volume and morphology in man. Prostate. 1988;13(1):57–67. | ||
Isaacs JT. Prostatic structure and function in relation to the etiology of prostatic cancer. Prostate. 1983;4(4):351–366. | ||
Newell GR, Fueger JJ, Spitz MR, Babaian RJ. A case control study of prostate cancer. Am J Epidemiol. 1989;130(2):395–398. | ||
Mettlin C, Natarajan N, Huben R. Vasectomy and prostate cancer risk. Am J Epidemiol. 1990;132(6):1056–1061. | ||
Rosenberg L, Palmer JR, Zauber AG, Warshauer ME, Stolley PD, Shapiro S. Vasectomy and risk of prostate cancer. Am J Epidemiol. 1990;132(6):1051–1055. | ||
Sidney S, Quesenberry CP Jr, Sadler MC, Guess HA, Lydick EG, Cattolica EV. Vasectomy and the risk of prostate cancer in a cohort of multiethnic health-checkup examinees: second report. Cancer Causes Control. 1991;2(2):113–116. | ||
Spitz MR, Fueger JJ, Babaian JR. Vasectomy and the risk of prostate cancer (letter). Am J Epidemiol. 1991;134:108–109. | ||
Nienhuis H, Goldacre M, Seagroatt V, Gill L, Vessey M. Incidence of disease after vasectomy: a record linkage retrospective cohort study. Br Med J. 1992;304(6829):743–746. | ||
Peterson DE, Remington PL, Anderson HA. Re: vasectomy and the risk of prostate cancer (letter). Am J Epidemiol. 1992;135(3):324–325. | ||
Giovannucci E, Ascherio A, Rimm E, Colditz G, Stampfer M, Willett W. A prospective cohort study of vasectomy and prostate cancer in US men. JAMA. 1993;269(7):873–877. | ||
Hayes RB, Pottern LM, Greenberg R, et al. Vasectomy and prostate cancer in the US blacks and whites. Am J Epidemiol. 1993;137(3):263–269. | ||
Hsing AW, Wang RT, Gu FL, et al. Vasectomy and prostate cancer risk in China. Cancer Epidemiol Biomarkers Prev. 1994;3(4):285–288. | ||
Hiatt RA, Armstrong MA, Klatsky AL, Sidney S. Alcohol consumption, smoking, and other risk factors and prostate cancer in a large health plan cohort in California (United States). Cancer Causes Control. 1994;5(1):66–72. | ||
Rosenberg L, Palmer JR, Zauber AG, et al. The relation of vasectomy to the risk of cancer. Am J Epidemiol. 1994;140(5):431–438. | ||
John EM, Whittemore AS, Wu AH, et al. Vasectomy and prostate cancer: results from a multiethnic case-control study. J Natl Cancer Inst. 1995;87(9):662–669. | ||
Zhu K, Stanford J, Daling J, et al. Vasectomy and prostate cancer: a case-control study in a health maintenance organization. Am J Epidemiol. 1996;144(8):717–722. | ||
Ewings P, Bowie C. A case-control study of cancer of the prostate in Somerset and east Devon. Br J Cancer. 1996;74(4):661–666. | ||
Andersson SO, Baron J, Bergström R, Lindgren C, Wolk A, Adami HO. Lifestyle factors and prostate cancer risk: a case-control study in Sweden. Cancer Epidemiol. 1996;5(7):509–513. | ||
Platz EA, Yeole BB, Cho E, Jussawalla DJ, Giovannucci E, Ascherio A. Vasectomy and prostate cancer: a case-control study in India. Int J Epidemiol. 1997;26(5):933–938. | ||
DeAntoni EP, Göktas S, Stenner J, O’Donnell C, Crawford ED. A cross-sectional study of vasectomy, time since vasectomy and prostate cancer. Prostate Cancer Prostatic Dis. 1997;1(2):73–78. | ||
Lesko SM, Louik C, Vezina R, Rosenberg L, Shapiro S. Vasectomy and prostate cancer. J Urol. 1999;161(6):1848–1853. | ||
Stanford J, Wicklund K, McKnight B, Daling J, Brawer M. Vasectomy and risk of prostate cancer. Cancer Epidemiol Biomarkers Prev. 1999;8(10):881–886. | ||
Emard JF, Drouin G, Thouez JP, Ghadirian P. Vasectomy and prostate cancer in Quebec, Canada. Health Place. 2001;7(2):131–139. | ||
Lynge E. Prostate cancer is not increased in men with vasectomy in Denmark. J Urol. 2002;168(2):488–490. | ||
Cox B, Sneyd M, Paul C, Delahunt B, Skegg D. Vasectomy and risk of prostate cancer. JAMA. 2002;287(23):3110–3115. | ||
Rohrmann S, Paltoo D, Platz E, Hoffman S, Comstock G, Helzlsouer K. Association of vasectomy and prostate cancer among men in a Maryland cohort. Cancer Causes Control. 2005;16(10):1189–1194. | ||
Holt S, Salinas C, Stanford J. Vasectomy and risk of prostate cancer. J Urol. 2008;180(6):2565–2568. | ||
Romero FR, Romero AW, Almeida RM, Oliveira FC Jr, Tambara Filho R. The significance of biological, environmental, and social risk factors for prostate cancer in a cohort study in Brazil. Int Braz J Urol. 2012;38(6):769–778. | ||
Siddiqui M, Wilson K, Epstein M, et al. Vasectomy and risk of aggressive prostate cancer: a 24-year follow-up study. J Clin Oncol. 2014;32(27):3033–3038. | ||
Sokal D, Labrecque M, Belker A, et al. Prostate cancer and vasectomy: déjà vu! J Clin Oncol. 2015;33(6):669–670. | ||
McDonald S. Is vasectomy harmful to health? Br J Gen Pract. 1997;47(419):381–386. | ||
Dennis L, Dawson D, Resnick M. Vasectomy and the risk of prostate cancer: a meta-analysis examining vasectomy status, age at vasectomy, and time since vasectomy. Prostate Cancer Prostatic Dis. 2002;5(3):193–203. | ||
Shang Y, Han G, Li J, et al. Vasectomy and prostate cancer risk: a meta-analysis of cohort studies. Sci Rep. 2015;5:9920. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

