Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Value of Serum Adiponectin Combined with ABCD2 in Predicting Cerebral Infarction Among Patients with Acute Isolated Vertigo
Authors Qian S, Zhang X, Wang Y
Received 22 April 2022
Accepted for publication 21 July 2022
Published 29 July 2022 Volume 2022:18 Pages 1553—1559
DOI https://doi.org/10.2147/NDT.S371812
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Shuxia Qian, Xiaoling Zhang, Yanping Wang
Department of Neurology, The Second Affiliated Hospital of Jiaxing University, Jiaxing, 314000, People’s Republic of China
Correspondence: Xiaoling Zhang; Yanping Wang, Department of Neurology, The Second Affiliated Hospital of Jiaxing University, No. 1518 the North Road Around the City, Jiaxing, 314000, People’s Republic of China, Email [email protected]; [email protected]
Introduction: Patients with acute isolated vertigo have a high risk for developing cerebral infarction (CI). Risk stratification for cerebral infarction in patients with acute isolated vertigo is critical for early treatment and preventative therapy. In the present study, we aim to characterize the diagnostic value of serum adiponectin (APN) combined with ABCD2 scoring in determining cerebral infarction risk.
Methods: Patients with acute isolated vertigo admitted to the emergency room were recruited. Diagnosis of cerebral infarction was performed using diffusion-weighted MRI (DWI-MRI) and T2WI and T2Flair imaging. Blood was collected for analysis of APN levels using enzyme-linked immunosorbent assay (ELISA). Multivariate analysis was used to analyze diabetes, hypertension, serum APN, and ABCD2 in association with CI.
Results: Compared to non-CI patients (n = 185), patients with CI (n = 68) demonstrated significantly lower serum APN levels (p < 0.001) and higher ABCD2 score (p < 0.001). A strong negative correlation was found between serum APN levels and ABCD2 scores. Multivariate analysis and ROC analysis suggested that low serum APN and high ABCD2 are strong predictors of CI in patients with acute isolated vertigo. Notably, the combination of APN and ABCD2 had a much stronger predictive sensitivity and specificity.
Conclusion: Our analysis suggests that the combination of serum APN and ABCD2 analyses offers a significantly improved prediction sensitivity and specificity for CI among patients with acute and isolated vertigo, which supports the potential use of this new marker in clinics.
Keywords: acute isolated vertigo, adiponectin, ABCD2, cerebral infarction
Introduction
Vertigo/dizziness is a common symptom of vertebrobasilar diseases, which account for about 20% of ischemic events.1 Isolated vertigo, caused predominantly by vestibular lesions and being one of the common types of vertigo, manifests as vegetative dysfunction such as vomiting, diarrhea, nausea, and neurological deficits such as compromised consciousness, motor and sensory functions.2 Isolated vertigo is considered a sign of circulatory ischemia in the brain and patients with acute vertigo (those who visited the emergency department) are two times more likely to develop cardiovascular events or stroke during a three-year follow-up than those without acute vertigo.2,3
Effectively stratifying the risk of cerebral infarction among patients with isolated vertigo is important for early detection of cerebral infarction, effective treatment, and improvement of patient prognosis. Unfortunately, management of vertigo in the emergency department is hindered by difficulties in diagnosis based on a constellation of signs and symptoms. While computed tomography (CT) is considered of little diagnostic value, brain magnetic resonance imaging (MRI) is now used as gold standard in differentiating patients with central or peripheral vertigo and detecting cerebral infarction.4 However, limited accessibility and the high cost of MRI make screening patients with uncertain diagnosis difficult, particularly in the emergency department. Previously, efforts have been devoted to developing novel diagnostic markers, such as neutrophil-to-lymphocyte ratio (NLR)5 and serum neuron-specific enolase and vertebral artery abnormality,6 to assess the risk of cerebral infarction among patients with isolated vertigo. These studies underlined the urgent need of a more clinically accessible and cost-effective tool for cerebral infarction diagnosis. ABCD2 scoring system has also demonstrated clinical utility in the emergency department settings for assessing the risk of stroke after ischemic attack among patients with vertigo.7,8 An ABCD2 score of 3 or less is found to indicate a lower risk of the cerebrovascular event compared with a score of 4 or more. Nonetheless, the utility of ABCD2 scoring in stratifying cerebral infarction risk is still unknown.
A serum biomarker correlated with cerebral infarction risk is desirable for providing a quick and cost-effective test to identify patients for further brain MRI examinations. Previously, a number of studies have been devoted to characterizing several serum proteins, such as the calcium-binding protein S100B,9 as biomarkers for cerebrovascular events among patients with vertigo. The present work aimed to characterize the diagnostic value of serum adiponectin (APN), as a new serum biomarker, in predicting cerebral infarction among patients with acute isolated vertigo. APN is an endogenous bioactive protein abundantly expressed in adipose tissue, and studies have found that APN has various effects such as anti-inflammatory, anti-atherosclerotic, regulating glucose metabolism, lipid metabolism, and increasing insulin sensitivity.10 APN has been reported to have significant correlation to clinical outcome of patients after ischemic stroke,11 and a significant decrease in APN in serum of patients has substantial diagnostic value in terms of cognitive performance.12,13 Besides investigating the diagnostic performance of APN and ABCD2 individually, here we also evaluated the diagnostic sensitivity and specificity of APN combined with ABCD2 test for improved diagnostic efficiency among patients with acute isolated vertigo.
Subjects and Methods
Subjects
Our study was approved by the ethics committee of the Second Affiliated Hospital of Jiaxing University (#JXEY-2019JX103). The study was conducted in accordance with the Declaration of Helsinki, Ethical Principles for Medical Research Involving Human Subjects. Patients who visited our emergency department with complaints of acute persistent vertigo were recruited. Inclusion criteria were as follows: 1) patients should have no signs and symptoms of focal neurological deficits; 2) no history of stroke; 3) no disorders related to limb or somatic ataxia; and 4) provided informed written consent.
Exclusion criteria were as follows: 1) Patient with age less than 18 years; 2) onset of disease more than 14 days; 3) severe dementia, psychosis unable to cooperate; 4) impaired consciousness and unstable vital signs; 5) tumors, hemorrhage, previous intracranial lesions; 6) metal implants that preclude MRI scans. A total of 185 non-CI patients and 68 CI patients were included for analysis.
The flow chart of the study is shown in Figure S1.
ABCD2 Scoring
The patients were scored as follows: 1) 1 point for age greater than or equal to 60 years; 2) 1 point for systolic blood pressure greater than or equal to 140 mmHg or diastolic blood pressure greater than or equal to 90 mmHg; 3) 2 point for unilateral weakness; 4) 1 point for speech disorder; 4) 2 points for symptoms that last more than 60 minutes (1 point for symptoms that last between 10 and 59 minutes); 1 point for diabetes mellitus.
Brain MRI
Patients were diagnosed with cerebral infarction by brain MRI and images were evaluated by a specialized neurologist. In brief, the following criteria were used for diagnosis: CI in hyperacute phase: elevated diffusion-weighted imaging (DWI) signal with no significant changes in T2WI and T2Flair signal; CI in acute phase: slightly lower or equal T1WI signal and enhanced T2WI and T2Flair signal in the lesions; CI in the subacute phase: enhanced T2WI and T2Flair signal; CI in the chronic phase: low T1WI signal, high T2WI signal, high T2Flair signal in the brain but low T2Flair signal at the site of the lesion.
Blood Tests
Three to five milliliters of fasting venous blood were drawn in the early morning. Blood was tested for urea nitrogen, total cholesterol, HDL-C and LCL-C levels using routine clinical procedures and serum APN concentration was measured by an ELISA kit (Abcam, USA).
Data Analysis
SPSS version 16.0 was used for analysis. The comparisons between the two groups were conducted by Fisher’s exact test or Chi-square test or Mann–Whitney test. For a multivariate analysis, the factors in univariate analyses with p ≤ 0.25 were further selected to conduct a logistic regression analysis. The receiver operating characteristic (ROC) analysis was used to determine detection sensitivity and specificity. p < 0.05 was set as statistical significance.
Results
Study Design and Baseline Characteristics
Our study recruited 290 patients admitted due to acute isolated vertigo, among which 37 were excluded due to history of stroke (n=37), impaired consciousness (n=13), MRI abnormalities (n=7), and symptoms of focal neurological deficits (n=9). A total of 253 patients were included in data analysis (n=185 for non-CI for n=68 for CI). Table 1 shows the comparison of baseline data between the two groups of patients. Those with age >60 constitute the majority of both non-CI and CI groups. We found that age, gender and other factors did not affect whether acute isolated vertigo was correlated with cerebral infarction. However, diabetes mellitus (p<0.001) and hypertension (p<0.001) among the underlying diseases were significantly different between the two groups. The patent characteristics regarding different ischemic stroke subtypes and topology of cerebral ischemia in the study population are shown in Table S1.
 |
Table 1 Baseline Characteristics of Acute, Isolated Vertigo Complicated with Cerebral Infarction (CI) and without Cerebral Infarction (Non-CI) |
Downregulation of Serum APN and Higher ABCD2 Scores are Characteristics of Patients with Acute Isolated Vertigo and Cerebral Infarction
Serum APN levels and ABCD2 scores of non-CI and CI groups were acquired to evaluate their diagnostic values. As shown in Figure 1, a significantly lower level of serum APN (Figure 1A) and higher ABCD2 score (Figure 1B) were seen in the CI group compared to the non-CI group. Further, there was a significant negative correlation between the serum APN levels and ABCD2 score (Figure 1C).
Diagnostic Values of the Serum APN Level, ABCD2 Score and Their Combination
We next performed multivariate logistic analysis on how diabetes, hypertension, low serum APN and high ABCD2 correlate with CI among patients with acute isolated vertigo. We show that all the above factors can serve as significant risk factors for CI (Table 2, p=0.003 for diabetes, p=0.007 for hypertension, p<0.001 for low serum APN, and p<0.001 for high ABCD2).
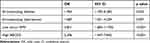 |
Table 2 Multivariate Logistic Analysis for Acute, Isolated Vertigo Complicated with Cerebral Infarction |
ROC analysis of serum APN (Figure 2A), ABCD2 score (Figure 2B) further showed that high AUC values could be achieved for both diagnostic markers (AUC=0.6911, 0.6995 for serum APN and ABCD2 respectively). Using a cut-off value of 3.74 mg/mL and 4, ROC analysis suggested a relatively high sensitivity (54.41% for serum APN and 58.82 for ABCD2) and specificity (77.3% for serum APN and 72.97% for ABCD2). Notably, the combination of serum APN and ABCD2 score outperformed either diagnostic marker alone (AUC=0.8168, sensitivity=75% and specificity=78.92%) (Figure 2C and Table 3). We also performed analysis of the subgroups with age >60 years. As shown in Table 1, the numbers of the elderly subgroups were N = 97 for Non-CI and N = 41 for CI. The analyses of serum APN levels and ABCD2 scores are shown in Figure S2. The ROC analysis (shown in Figure S3 and Table S2) suggested strong predictive values of the combined APN level and ABCD2 score in diagnosing cerebral infarction among patients with acute isolated vertigo in the elderly subgroups. In addition, the diagnostic values of positive predictive value and negative predictive value were shown in Table S3.
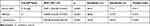 |
Table 3 Diagnostic Values in ROC Analysis |
Discussion
Here we strive to develop a new diagnostic tool for CI risk for patients with acute isolated vertigo, which is a common complication among patients who visit the emergency department. It was estimated that CI accounts for about 0.7–10% of the patients with isolated vertigo.14,15 We found that 68/253 (26.9%) of our patients with acute isolated vertigo had confirmed CI, a higher percentage that might be attributed to different selection criteria.
We assessed the diagnostic values of serum APN, ABCD2 and the combination of both in detecting CI in patients, with MRI being used as the standard to identify CI patients.16 The purpose of our study is to provide a cost-effective and rapid diagnostic tool, that may be used either for initial screening of patients susceptible for CI or to identify high-risk patients for MRI confirmation. This is particularly critical in emergency care settings, where MRI is less accessible. While the use of serum APN alone achieved similar diagnostic sensitivity and specificity compared to ABCD2 scoring, which is the mainstay evaluation for the patients with vertigo based on clinical symptoms, we showed that by combining serum APN and the ABCD2 scoring, a significantly higher diagnostic sensitivity and specificity can be achieved. Therefore, the addition of serum APN as another biomarker can potentially greatly improve efficiency in identifying patients with a high risk for CI.
Our results suggested a novel use of serum APN measurement in CI diagnosis. As previously reported, serum APN measurement is being developed as a clinical test in applications such as identifying patients with hearing impairment due to the protective anti-apoptotic role of APN in hair cells.17 Owing to the significant metabolite-regulating function through sensitizing body to insulin, measurement of serum APN has been found to have clinical implications in metabolic syndromes, insulin resistance, etc. Hence, it is envisioned that measurement of serum APN as a clinical test could facilitate clinical management of CI among patients with isolated vertigo. Yet, how APN is related to CI pathogenesis is not addressed in our study. It is previously proven that low adiponectin levels have a strong correlation with cerebrovascular and neurodegenerative diseases.18–20 Recent studies have suggested that adiponectin adopts a neuroprotective role against ischemic attack through the cAMP/PKA-CREB-BDNF signaling21 and the AdipoR1/AMPK pathways.22 High levels of adiponectin have also been reported to associate with major cerebral vascular events and mortality risk in ischemic stroke.23 Further studies are needed to elucidate the molecular basis of APN in CI among patients with acute isolated vertigo.
Our study is limited by a relatively small number of patients, but the potential value of serum APN demonstrated in our study supports further larger study to systemically evaluate serum APN as a new diagnostic tool, and potentially determine optimal cut-off values for higher diagnostic sensitivity and specificity. We restricted our study to patients with isolated vertigo patients in the acute phase without obvious neurologic deficits, and therefore our conclusions may not hold for isolated vertigo patients with less acute symptoms. In addition, our approach could also be used during the one-year follow-up period to monitor treatment responses, as isolated vertigo occurs as an early sign of cerebral infarction, which is important for early detection of cerebral infarction, early treatment and improvement of patient prognosis. Compared to cranial DWI-MRI, which is costly and time consuming, our study offers a new diagnostic marker to screen patients with potential cerebral infarction based on isolated vertigo. Further studies that establish the diagnostic utility of APN and ABCD2 tests in identifying high-risk patients for cerebral infraction in a larger clinical trial and among more diverse population would help translate these two new diagnostic markers into clinics.
Conclusions
In this study, we explored the diagnostic value of serum APN in identifying CI among patients with acute isolated vertigo. We found that downregulation of APN, along with higher ABCD2 scores, are characteristics of CI patients with acute isolated vertigo. Combining measurement of serum APN and ABCD2 scores, a significantly improved diagnostic sensitivity and specificity for CI can be achieved, suggesting the high clinical potential of serum APN measurement in the clinical management of patients with acute isolated vertigo.
Data Sharing Statement
All data generated or analyzed during this study are included in the manuscript.
Funding
The study was supported by public welfare research plan of Jiaxing Science and Technology Bureau (2019AD32168).
Disclosure
No competing financial interests exist.
References
1. Savitz SI, Caplan LR. Vertebrobasilar disease. N Engl J Med. 2005;352(25):2618–2626. doi:10.1056/NEJMra041544
2. Lee CC, Su YC, Ho HC, et al. Risk of stroke in patients hospitalized for isolated vertigo: a four-year follow-up study. Stroke. 2011;42(1):48–52. doi:10.1161/STROKEAHA.110.597070
3. Lee SH, Kim JS. Acute diagnosis and management of stroke presenting dizziness or vertigo. Neurol Clin. 2015;33(3):687–98, xi. doi:10.1016/j.ncl.2015.04.006
4. Kabra R, Robbie H, Connor SEJ. Diagnostic yield and impact of MRI for acute ischaemic stroke in patients presenting with dizziness and vertigo. Clin Radiol. 2015;70(7):736–742. doi:10.1016/j.crad.2015.01.016
5. Lee SH, Yun SJ, Ryu S, et al. Utility of Neutrophil-to-lymphocyte ratio (NLR) as a predictor of acute infarction in new-onset acute vertigo patients without neurologic and computed tomography abnormalities. J Emerg Med. 2018;54(5):607–614. doi:10.1016/j.jemermed.2017.12.058
6. Zuo L, Zhan YQ, Liu FF, et al. Clinical and laboratory factors related to acute isolated vertigo or dizziness and cerebral infarction. Brain Behav. 2018;8(9):e01092. doi:10.1002/brb3.1092
7. Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet. 2007;369(9558):283–292. doi:10.1016/S0140-6736(07)60150-0
8. Navi BB, Kamel H, Shah MP, et al. Application of the ABCD2 score to identify cerebrovascular causes of dizziness in the emergency department. Stroke. 2012;43(6):1484–1489. doi:10.1161/STROKEAHA.111.646414
9. Kartal AG, Yilmaz S, Yaka E, et al. Diagnostic value of S100B protein in the differential diagnosis of acute vertigo in the emergency department. Acad Emerg Med. 2014;21(7):736–741. doi:10.1111/acem.12420
10. Yanai H, Yoshida H. Beneficial effects of adiponectin on glucose and lipid metabolism and atherosclerotic progression: mechanisms and perspectives. Int J Mol Sci. 2019;20(5):1190. doi:10.3390/ijms20051190
11. Wang ZL, Li B, Wang YX, et al. The association between serum adiponectin and 3-month outcome after ischemic stroke. Cardiovasc Diabetol. 2019;18(1). doi:10.1186/s12933-019-0908-z
12. Rizzo MR, Fasano R, Paolisso G. Adiponectin and cognitive decline. Int J Mol Sci. 2020;21(6):2010. doi:10.3390/ijms21062010
13. van Andel M, van Schoor NM, Korten NC, Comijs HC, Heijboer AC, Drent ML. The association between high-molecular-weight adiponectin, ghrelin and leptin and age-related cognitive decline: results from longitudinal aging study Amsterdam. J Gerontol Ser A. 2021;76(1):131–140. doi:10.1093/gerona/glaa126
14. Neuhauser HK, von Brevern M, Radtke A, et al. Epidemiology of vestibular vertigo - A neurotologic survey of the general population. Neurology. 2005;65(6):898–904. doi:10.1212/01.wnl.0000175987.59991.3d
15. Doijiri R, Uno H, Miyashita K, Ihara M, Nagatsuka K. How commonly is stroke found in patients with isolated vertigo or dizziness attack? J Stroke Cerebrovasc Dis. 2016;25(10):2549–2552. doi:10.1016/j.jstrokecerebrovasdis.2016.06.038
16. Marzo SJ, Leonetti JP. The importance of magnetic resonance imaging in the evaluation of vertigo and imbalance. Skull Base Surg. 2000;10(4):171–172. doi:10.1055/s-2000-9334
17. Wu CC, Tsai CH, Lu YC, et al. Contribution of adiponectin and its type 1 receptor to age-related hearing impairment. Neurobiol Aging. 2015;36(6):2085–2093. doi:10.1016/j.neurobiolaging.2015.02.030
18. Matsumoto M, Ishikawa S, Kajii E. Association of adiponectin with cerebrovascular disease: a nested case-control study. Stroke. 2008;39(2):323–328. doi:10.1161/STROKEAHA.107.497552
19. Yang Y, Hu W, Jiang S, et al. The emerging role of adiponectin in cerebrovascular and neurodegenerative diseases. Biochim Biophys Acta. 2015;1852(9):1887–1894. doi:10.1016/j.bbadis.2015.06.019
20. Chen MP, Tsai JCR, Chung FM, et al. Hypoadiponectinemia is associated with ischemic cerebrovascular disease. Arterioscler Thromb Vasc Biol. 2005;25(4):821–826. doi:10.1161/01.ATV.0000157784.25920.a7
21. Bai H, Zhao L, Liu HX, et al. Adiponectin confers neuroprotection against cerebral ischemia-reperfusion injury through activating the cAMP/PKA-CREB-BDNF signaling. Brain Res Bull. 2018;143:145–154. doi:10.1016/j.brainresbull.2018.10.013
22. Liu B, Liu J, Wang JG, et al. Adiponectin protects against cerebral ischemic injury through AdipoR1/AMPK pathways. Front Pharmacol. 2019;10:597.
23. Tu WJ, Qiu HC, Liu YK, Liu Q, Zeng XW, Zhao JZ. Elevated levels of adiponectin associated with major adverse cardiovascular and cerebrovascular events and mortality risk in ischemic stroke. Cardiovasc Diabetol. 2020;19(1). doi:10.1186/s12933-020-01096-3
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


