Back to Journals » Drug Design, Development and Therapy » Volume 14
Validation of the Key Active Ingredients and Anti-Inflammatory and Analgesic Effects of Shenjin Huoxue Mixture Against Osteoarthritis by Integrating Network Pharmacology Approach and Thin-Layer Chromatography Analysis
Authors Yu MX , Ma XQ, Song X, Huang YM, Jiang HT, Wang J, Yang WH
Received 27 December 2019
Accepted for publication 25 February 2020
Published 16 March 2020 Volume 2020:14 Pages 1145—1156
DOI https://doi.org/10.2147/DDDT.S243951
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tuo Deng
Mei-Xiang Yu,1,* Xiao-Qin Ma,1,* Xin Song,2 Yong-Mei Huang,3 Hui-Ting Jiang,1 Jing Wang,1 Wan-Hua Yang1,4
1Department of Pharmacy, Ruijin Hospital, Shanghai Jiaotong University School of Medicine, Shanghai 200025, People’s Republic of China; 2South Campus, Renji Hospital, Shanghai Jiaotong University School of Medicine, Shanghai 201100, People’s Republic of China; 3Jinshan Hospital, Shanghai Fudan University School of Medicine, Shanghai 201508, People’s Republic of China; 4Department of Pharmacy, Ruijin Hospital North Affiliated to the Shanghai Jiao Tong University Medical School, Shanghai 201801, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Wan-Hua Yang Email [email protected]
Background: Shenjin Huoxue Mixture (SHM), a classic traditional herb mixture has shown significant clinical efficacy against osteoarthritis (OA). Our previous experimental study has confirmed its anti–inflammatory and analgesic effect on acute soft tissue injury in rats, with the compound of glycyrrhizinate in SHM identified and the content of paeoniflorin in SHM determined by high-performance liquid chromatography (HPLC). However, the components and its pharmacological mechanisms of SHM against OA have not been systematically elucidated yet. Thus this study aimed to predict the key active ingredients and potential pharmacological mechanisms of SHM in the treatment of OA by network pharmacology approach and thin-layer chromatography (TLC) validation.
Methods: The active ingredients of SHM and their targets, as well as OA-related targets, were identified from databases. The key active ingredients were defined and ranked by the number of articles retrieved in PubMed using the keyword “(the active ingredients [Title/Abstract]) AND Osteoarthritis[Title/Abstract] ”, and validated partially by TLC. The pharmacological mechanisms of SHM against OA were displayed by GO term and Reactome pathway enrichment analysis with Discovery Studio 3.0 software docking to testing the reliability.
Results: Finally, 16 key active ingredients were identified and ranked, including quercetin validated through TLC. Inflammatory response, IL-6 signaling pathway and toll-like receptor (TLR) cascades pathway were predicted as the main pharmacological mechanisms of SHM against OA. Especially, 12 out of 16 key active ingredients, including validated quercetin, were well docked to IL-6 proteins.
Conclusion: Our results confirmed the anti–inflammatory and analgesic effect of SHM against OA through multiple components, multiple targets and multiple pathways, which revealed the theoretical basis of SHM against OA and may provide a new drug option for treating OA.
Keywords: Shenjin Huoxue Mixture, osteoarthritis, active ingredients, pharmacological mechanisms, network pharmacology, thin-layer chromatography
Introduction
Osteoarthritis (OA) is one of the most common cause of pain and disability among the elderly and adults of working age around the world with a current prevalence of approximately 15% and a predicted prevalence of 35% in 2030.1,2 OA has long been considered as a “wear and tear” disease, characterized by losing articular cartilage and subchondral bone sclerosis. Today it has been generally accepted that inflammation-driven by innate immunological mechanisms plays a key role in tissue destruction in OA.3 Especially, the relationship between inflammation and pain in OA has been an area of investigation recently.4
Today prevention and therapy of OA focus on lifestyle modification, pain management, and joint replacement for the end-stage disease.5 However, the functional outcomes of joint replacement could be disappointed and the lifespan of prostheses is limited.5 The primary effective drugs for pain control are paracetamol and non-steroidal anti–inflammatory,6,7 but their prolonged use is associated with potential risks, such as dyspepsia and life-threatening ulcer perforations and bleeds.7 Considering that OA is a much more complex disease with inflammatory,8 the traditional Chinese medicine (TCM) has unique clinical advantages by modification of disease and symptoms in OA.9 According to a meta-analysis, TCM significantly improved knee OA pain (P < 0.004) and total effectiveness rates (p < 0.0003).10 The guidelines of OA diagnosis and treatment in China also affirmed the role of TCM against OA, despite more rigorous studies are needed to support their use.11
Shenjin Huoxue Mixture (SHM), a classic TCM rooted from “Wei’s traumatology” which has been known for hundred years of a certain clinical effect on joint injuries, or aching leg and waist.12 SHM has been approved to treat joint disease such as OA for decades in Ruijin hospital affiliated to Shanghai Jiao Tong University by the Shanghai Food and Drug Administration. It composed of 12 herbs, including Herba Lycopodii (HL), Herba Taxilli (HT), Cibot Rhizome (CR), Radix Dipsaci (RD), Myrrha (MH), Frankincense (FK), Radix Angelicae Sinensis (RAS), Radix Paeoniae Alba (RPA), Carica papaya L. (CPL), Radix Gentianae Macrophyllae (RGM), Radix Achyranthis Bidentatae (RAB) and Radix Glycyrrhizae (RG). We have identified paeoniflorin and glycyrrhizinate in SHM by thin-layer chromatography (TLC) method and the content of paeoniflorin by high-performance liquid chromatography (HPLC).13,14 Our previous experimental study showed significant effects of SHM in anti–inflammatory and alleviating pain to a various degree in acute soft tissue injury.15 What’s more, 9 out of 12 herbs in SHM have been used in treating OA,16 of which HL is of the highest use frequency for fuming-washing therapy against knee OA.16
However, the components and its pharmacological mechanisms of SHM against OA have not been systematically elucidated yet. Thus this study aimed to predict the key active ingredients and potential pharmacological mechanisms of SHM against OA by network pharmacology approach and TLC validation.
A flowchart of the network pharmacology approach is presented in Figure 1.
Materials and Methods
Active Ingredients of SHM Screening
The active ingredients of all herbs in SHM were screened from the Traditional Chinese Medicine Systems Pharmacology (TCMSP) Database ( http://tcmspw.com/tcmsp.php, download on January 18, 2019) as well as literature.17 According to the most common criteria by the TCMSP database, the active ingredients of oral bioavailability (OB) > 30% and drug-likeness (DL) ≥ 0.18 were selected for subsequent research. The key active ingredients were identified if articles were retrieved from PubMed (https://www.ncbi.nlm.nih.gov/pubmed) using “(the active ingredients[Title/Abstract]) AND Osteoarthritis[Title/Abstract]” as the keyword, and ranked by the number of articles retrieved. Besides, the specific structures of those ingredients were obtained from the PubChem database (https://pubchem.ncbi.nlm.nih.gov/).
TLC Validation the Key Active Ingredients in SHM
50mL of SHM (Ruijin hospital affiliated to Shanghai Jiao Tong University, Shanghai, China) was dissolved in 25% hydrochloric acid, vibrating extraction twice (ethyl acetate, 30 mL). Next, the ethyl acetate solution was washed (distilled water, 10 mL), discarding the aqueous solution. Finally, the dissolved residue (ethyl acetate, 1 mL) was prepared as an SHM sample.
The standard sample of quercetin (China National Institute for the Control of Pharmaceutical and Biological Products, Shanghai, China) was prepared by dissolving the solutes in ethyl acetate.
According to the TLC (General Rule 0502, Part IV, Chinese Pharmacopoeia) test, the SHM sample (10 μL) and quercetin standard sample (2 μL) were spotted manually on the chromatographic plate. The mixture of toluene - trichloromethane - acetone - formic acid (8: 5: 8.5: 0.6) was used as a mobile phase. The plate was developed vertically at room temperature (20°C) to a distance of 10 cm, then dried for 20 hours and examined under UV light (365nm).18
Putative Targets of the Active Ingredients and OA
The targets of the active ingredients were predicted by inputting their structure to Swiss Target Prediction (http://www.swisstargetprediction.ch, download on January 28, 2019), a freely accessed web server designed to accurately predict the targets of active ingredients based on 2D and 3D similarity measures with known ligands.19
Known targets for the treatment of OA were identified from four widely used databases using “osteoarthritis” as the keyword.20 Four databases were Online Mendelian Inheritance in Man Database OMIM (http://www.omim.org/,download on January 8, 2019), the Kyoto Encyclopedia of Genes and Genomes Pathway Database(KEGG, http://www.kegg.jp/,download on January 8, 2019), DisGeNET database(https://www.disgenet.org/search, download on January 8, 2019), DrugBank database (https://www.drugbank.ca/, download on January 8, 2019). Besides, the main differentially expressed genes (DEGs) between end-stage OA synovial biopsies and biopsies without a joint disease were extracted from microarray data GSE82107 in the Gene Expression Omnibus (GEO; http://www.ncbi.nlm.nih.gov/geo/) database with a cut-off value of P < 0.05 and fold change |FC| ≥ 2.20 Removal of duplicates, these known targets and DEGs were identified as genes related to OA.
Candidate Targets and Protein-Protein Interaction (PPI)
Candidate targets with therapeutic effects against OA were identified by mapping the targets of the active ingredients of SHM and OA.21 Those candidate targets were ranked by the number of articles retrieved in PubMed (https://www.ncbi.nlm.nih.gov/pubmed) using the keywords “(the candidate targets[Title/Abstract]) AND Osteoarthritis[Title/Abstract]”. Candidate targets with a larger number of recorded articles were determined as the key targets. Besides, the proteins that interacted with these candidate targets were obtained from STRING database (http://string-db.org/, download March 13, 2019), a database of known and predicted interactions of proteins with four categories of confidence score: highest(0.9), high (0.7), medium (0.4) and low (0.1).22 Base on these, the score ≥ 0.9 was set to identify proteins interacting with candidate targets.
Network Construction and Analysis
A network of “candidate targets - proteins” was constructed using the Cytoscape 3.61 software,23 and then parameters in the network such as degree were calculated by NetworkAnalyzer. Nodes with degree values exceeding twice the average value of all nodes in the network were considered to playing an important role in the network.24
Enrichment Analysis for Candidate Targets
The online GO term enrichment analysis was performed by inputting all the candidate targets into the DAVID server (https://david.ncifcrf.gov/, v6.8) and online Reactome pathway enrichment analysis were carried out by putting them into ClueGO 2.5.4 plugin.25 Then, the key proteins in the main pathways were identified.
Molecular Docking Validation of Key Active Ingredients–Target Interaction
After identifying the key active ingredients and the key proteins, Discovery Studio 3.0 was used to perform molecular docking analysis to test the reliability of the results above enrichment analysis.26
Results
16 Key Active Ingredients in SHM Identified
A total of 157 active ingredients (Supplementary Table 1) were identified in this study. The number of active ingredients in HL, RAS, RPA, CPL, RGM, MH, FK, HT, CR, RD, RAB, and RG were 5, 2, 13, 4, 2, 15, 8, 2, 2, 8, 4 and 92, respectively. Among them, 16 active ingredients (quercetin, boswellic acid, catechin, carotenoid, kaempferol, paeoniflorin, naringenin, isorhamnetin, formononetin, stigmasterol, licochalcone A, ellagic acid, beta-sitosterol, sitosterol and calycosin, liquiritin) were recorded related to OA in PubMed, which were identified as the key active ingredients of SHM against OA. The rank of those key active ingredients and the overlapped between herbs and other details are shown in Table 1.
 |
Table 1 The Information About 16 Key Active Ingredients |
Quercetin Validated by TLC
Among 16 key active ingredients, quercetin was validated through TLC, see Figure 2. In the TLC chromatogram, there were fluorescent spots in the chromatogram of the SHM sample corresponding with the quercetin standard sample both in position and color.
 |
Figure 2 Results of TLC validation of quercetin in SHM. The first and third chromatographic bands are samples of SHM, and the second chromatographic band is a sample of quercetin. |
Targets of the Active Ingredients and OA Identified
A total of 876 targets of the active ingredients in SHM (Supplementary Table 2) were identified in our study.
A total of 908 known targets from the other four databases were collected. And 52 DEGs were extracted from microarray data GSE82107, including 26 up-regulated genes and 26 down-regulated genes, as shown in Figure 3. After a combination with known targets and DEGs and removing 13 duplicates, a total of 947 OA -related targets were identified (Supplementary Table 3).
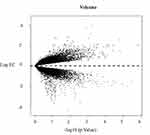 |
Figure 3 Volcano map of 52 DEGs. Red nodes represent up-regulated genes and green nodes represent down-regulated genes. |
153 Candidate Targets Identified and PPI Network Analysis
A total of 153 candidate targets were shown to have potential pharmacological effects against OA, including 10 key targets with the number of recorded articles exceeding 158. A network of “candidate targets - proteins” was constructed using the Cytoscape 3.61 software (Figure 4). There were 938 nodes and 4350 edges in the network, with an average degree value of 9.275, as calculated by using the Network Analyzer plugin. There were 50 nodes with degree values exceeding 19 (twice the average value of the degree). Details of those 10 key targets are listed in Table 2.
 |
Table 2 The Information About the Top 10 Key Targets |
Enrichment Analysis
GO term and Reactome pathway enrichment was performed to identify the mechanisms of SHM respectively. Results showed that the first GO term was related to the inflammatory response. Top 10 of GO terms of 153 candidate targets are listed in Figure 5. Reactome pathway enrichment was mainly related to the IL-6 signaling pathway and toll-like receptor cascades (TLR) (Figure 6).
Molecular Docking to IL-6 Protein
In our results of molecular docking, 12 out of 16 the key active ingredients, including validated quercetin, were well docked to proteins of IL-6, with several interactions with amino acid residues. 3D molecular docking model of the 12 key active ingredients with IL-6 protein, see Figure 7. While 2D molecular docking model is shown as Figure 8.
Discussion
OA is a complex disease associated with inflammatory, however, approved drugs that can prevent, slow or reverse the progression of OA are still limited.1 SHM was one of classic TCM with significant anti–inflammatory and analgesic effects on acute soft tissue injury.15 Our study identified 16 key active ingredients of SHM, of which quercetin were validated through TLC. And we predicted inflammatory response, IL-6 signaling pathway and TLR cascade pathway as the main pharmacological mechanisms of SHM against OA, which was validated by 12 key active ingredients well docking to IL-6 proteins.
Multi-Component in SHM Against OA in a Synergistic Way
In our study, 157 active ingredients in SHM were found, 16 of them were identified as the key active ingredients. The quercetin of the key active ingredients was validated through TLC and paeoniflorin was determined by HPLC in our previous study. According to several studies, quercetin had protective effects on anti–inflammation and relieved the accompanying symptoms such as pain related to OA.27,28 What’s more, paeoniflorin has been reported as protective effects against OA with anti-apoptosis and anti–inflammation effects on chondrocyte.29,30 As for other key active ingredients, formononetin existing in HL and RG has been proved the anti-catabolic effects on rat chondrocytes and articular cartilage,31 and it dose-dependently decreased IL-6 in OA subchondral osteoblasts.32 Stigmasterol existing in HL and RAS, was demonstrated to block cartilage degradation in the rabbit model of OA, showing potential anti- osteoarthritic properties.33,34 Another unique key active ingredients in FK, boswellic acid, was found significant synovial concentration and therapeutic efficacy in the mouse model.35 It could also improve physical and functional ability and reduce the pain and stiffness according to a pilot, randomized, double-blind, placebo-controlled trial.36
Thus, All those key active ingredients in SHM helped to cure the main disease of OA or treat the accompanying diseases or symptoms of pain synergistically.
The Anti-Inflammatory Effect Was the Pharmacological Mechanism of SHM Against OA
In our study, the GO term results showed the mechanisms of SHM against OA were mainly related to inflammatory response, and Reactome pathway enrichment showed inflammatory factor IL-6 signaling pathway and TLR cascade pathway were the main pathways of SHM against OA.
Inflammation has been increasingly recognized to serve as an important central orchestrator in OA pathophysiology.3 On the one hand, signs of inflammation such as inflammatory cytokines can be identified in knee OA patients.37 One of the inflammatory cytokines IL-6 does show an almost unequivocal elevation in keen or wrist OA synovial fluid compared to healthy controls.38–40 And IL-6 mediates IL-6 pathway has been demonstrated to play a key role in driving the progression of arthritis.41 On the other hand, the existence of a persistent inflammatory status in OA is facilitated by the large repertoire of innate immune receptors in joint cells, of which toll-like receptors (TLRs) are the best-characterized group.42,43 TLRs intracellular signaling precedes the activation of the nuclear factor kappa B (NF-kB) with subsequent production and release of different cytokines such as IL-6, IL-1 and TNF-α.41 By that, those TLR cascades result in initiating and amplifying inflammatory destruction.44 Thus a vicious circle in OA pathogenesis gets started.
Given the important role of inflammation in OA, targeting inflammatory has proposed the potential therapeutic effect in the setting of OA.45,46 Encouragingly, anti–inflammatory effects have been demonstrated by many herbs of SHM in treating OA. For example, reducing serum levels of inflammatory mediators such as IL-6 in the rat OA model was the result of the action of HL, RPA and RD,29,30,47,48 showing a therapeutic agent for the treatment of human OA. Especially, acute inflammation and chronic inflammatory conditions in the collagen-induced arthritis model would also benefit from RG therapy.49 Recently its anti–inflammatory potential has been considered to involve the TLR-4 pathway.50
Thus, combined with our docking results that 12 out of 16 the key active ingredients were well docked to proteins of IL-6 (Figure 7), we speculated that anti–inflammatory effects of SHM against OA mainly through the synergistic actions of regulation of IL-6 and TLR. Although, a meta-analysis that examined the effects of IL-1 inhibitors through the subgroups analysis showed no significant effects on OA.51 However, the subgroups analysis based on relatively smaller numbers of trials. Therefore, more high-quality studies will be needed to affirm the mechanism of SHM against OA is related to inflammatory response, IL-6 pathway or TLR pathway.
Analgesic Effects of SHM Against OA May Be Related to Its Anti-Inflammation Action
In addition to inflammation playing an important role in OA pathophysiology, the link between inflammation and pain in OA has also been a hot spot of investigation.4 Yuangui Lin studied that inhibition of IL-6 function could attenuate the central sensitization and pain behavior induced by OA, and proved that synovitis and pain in OA patients were associated with pro-inflammatory cytokine IL-6. Which proposed the potential therapeutic effects of anti- IL-6 on the chronic pain of OA.45 Interestingly, the IL-6 level reduced by HL, RPA and RD of SHM has been well examined in the rat OA model.29,30,47,48 Of important, Miller also wondered whether TLR-4 could provide a direct link between tissue damage and pain sensitization.52 Recently anti-acute and chronic inflammatory potential of RG in SHM was considered to involve in the TLR-4 pathway.50
These findings supported our previous study that SHM showed a certain effect on anti–inflammation and alleviating the pain in the rat model.15 Thus we explained the analgesia mechanisms of SHM were mainly related to its anti–inflammation effects by inhibition of IL-6 and TLR. However, further Vivo or Vitro experimental models and clinical trials will be needed to affirm these mechanisms of SHM.
Conclusion
In conclusion, the multi-component and multi-mechanism of SHM against OA were effectively elucidated through the network pharmacology approach. A total of 16 key active ingredients were identified and ranked, including quercetin validated through TLC. Inflammatory response, IL-6 signaling pathway and TLR cascade pathway were predicted as the main pharmacological mechanisms of SHM against OA. Especially, 12 out of 16 key active ingredients, including validated quercetin, were well docked to IL-6 proteins. These results supported SHM against OA through its anti–inflammatory and analgesic effects, which provided a reliable basis for the clinical application of SHM.
Abbreviations
SHM, Shenjin Huoxue mixture; OA, osteoarthritis; TCM, traditional Chinese medicine; TLC, thin-layer chromatography; OB, oral bioavailability; DL, drug-likeness; HPLC, high-performance liquid chromatography; FC, fold change; DEGs, differentially expressed genes; PPI, protein-protein interaction; TLR, toll-like receptor; HL, Herba Lycopodii; HT, Herba Taxilli; CR, Cibot Rhizome; RD, Radix Dipsaci; MH, Myrrha; FK, Frankincense; RAS, Radix Angelicae Sinensis; RPA, Radix Paeoniae Alba; CPL, Carica papaya L.; RGM, Radix Gentianae Macrophyllae; RAB, Radix Achyranthis Bidentatae; RG, Radix Glycyrrhizae.
Acknowledgments
This project was supported by the Shanghai Health and Wellness Committee (2016ZB0304-01) and (ZYKC201701007).
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Oo WM, Yu SP, Daniel MS, Hunter DJ. Disease-modifying drugs in osteoarthritis: current understanding and future therapeutics. Expert Opin Emerg Drugs. 2018;23(4):331–347.
2. Vina ER, Kwoh CK. Epidemiology of osteoarthritis: literature update. Curr Opin Rheumatol. 2018;30(2):160–167.
3. Geyer M, Schonfeld C. Novel insights into the pathogenesis of osteoarthritis. Curr Rheumatol Rev. 2018;14(2):98–107.
4. Scanzello CR. Role of low-grade inflammation in osteoarthritis. Curr Opin Rheumatol. 2017;29(1):79–85.
5. Glyn-jones S, Palmer AJ, Agricola R, et al. Osteoarthritis. Lancet. 2015;386(9991):376–387.
6. National, Clinical Guideline Centre UK. Osteoarthritis: Care and Management in Adults. London; 2014.
7. Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). 2012;64(4):465–474.
8. Karsdal MA, Michaelis M, Ladel C, et al. Disease-modifying treatments for osteoarthritis (DMOADs) of the knee and hip: lessons learned from failures and opportunities for the future. Osteoarthritis Cartilage. 2016;24(12):2013–2021.
9. Li L, Liu H, Shi W, et al. Insights into the action mechanisms of traditional Chinese medicine in osteoarthritis. Evid Based Complement Alternat Med. 2017;2017:5190986.
10. Chen B, Zhan H, Marszalek J, et al. Traditional Chinese medications for knee osteoarthritis pain: a meta-analysis of randomized controlled trials. Am J Chin Med. 2016;44(4):677–703.
11. Wang KZ. [The guidelines for diagnosis and treatment of osteoarthritis in 2018 edition]. Chin J Orthop. 2018;38(12):705–715. Chinese.
12. Liu T, Li FY, Zhang H. [Clinicalobservation of being treated lumber discherniation byShenjin Huoxue Mixture WhichRooted from ProvedPrescription of Wei’s Traumatology]. JSichuan Tradit Chin Med. 2014;11:59–61.Chinese.
13. Yang WH, Chen B, Xu JN. [TLC Identification of Shenjin Huoxue Mixture]. China Pharmacy. 2009. 20(15):50–52. Chinese.
14. Li J, Yang WH, Chen B, et al. [Determination of paeoniflorin in Shenjin Huoxue mixture by HPLC method]. Pract Pharma Clin Remedies. 2010;13(1):27–29. Chinese.
15. Jiang HT, Yang WH, Chen B, Li J, Shen LH. [Study on the anti-inflammatory, analgesic and treatment of soft tissue injury of Shenjin Huoxue Mixture]. Chin J Exp Formulas. 2013;19(10):269–272. Chinese.
16. Liu J, Pan J, Wang Y, et al. Component analysis of Chinese medicine and advances in fuming-washing therapy for knee osteoarthritis via unsupervised data mining methods. J Tradit Chin Med. 2013;33(5):686–691.
17. Ru J, Li P, Wang J, et al. TCMSP: a database of systems pharmacology for drug discovery from herbal medicines. J Cheminform. 2014;6:13.
18. Ma X, Yu M, Hao C, Yang W. Identifying synergistic mechanisms of multiple ingredients in Shuangbai tablets against proteinuria by virtual screening and a network pharmacology approach. Evid Based Complement Alternat Med. 2020;2020:1027271.
19. Gfeller D, Grosdidier A, Wirth M, Daina A, Michielin O, Zoete V. SwissTargetPrediction: a web server for target prediction of bioactive small molecules. Nucleic Acids Res. 2014;42(WebServer issue):W32–W38.
20. Yu M, Song X, Yang W, Li Z, Ma X, Hao C. Identify the key active ingredients and pharmacological mechanisms of compound XiongShao capsule in treating diabetic peripheral neuropathy by network pharmacology approach. Evid Based Complement Alternat Med. 2019;2019:5801591.
21. Gao L, Wang KX, Zhou YZ, Fang JS, Qin XM, Du GH. Uncovering the anticancer mechanism of Compound Kushen Injection against HCC by integrating quantitative analysis, network analysis and experimental validation. Sci Rep. 2018;8(1):624.
22. Franceschini A, Szklarczyk D, Frankild S, et al. STRING v9.1: protein-protein interaction networks, with increased coverage and integration. Nucleic Acids Res. 2013;41(Database issue):D808–D815.
23. Smoot ME, Ono K, Ruscheinski J, Wang PL, Cytoscape IT. 2.8: new features for data integration and network visualization. Bioinformatics. 2011;27(3):431–432.
24. Li S, Zhang ZQ, Wu LJ, Zhang XG, Li YD, Wang YY. Understanding ZHENG in traditional Chinese medicine in the context of neuro-endocrine-immune network. IET Syst Biol. 2007;1(1):51–60.
25. Alack K, Weiss A, Kruger K, et al. Profiling of human lymphocytes reveals a specific network of protein kinases modulated by endurance training status. Sci Rep. 2020;10(1):888.
26. Zhang J, Zhang Q, Chen X, et al. Revealing synergistic mechanism of multiple components in gandi capsule for diabetic nephropathy therapeutics by network pharmacology. Evid Based Complement Alternat Med. 2018;2018:6503126.
27. Sherif IO. Uroprotective mechanism of quercetin against cyclophosphamide-induced urotoxicity: effect on oxidative stress and inflammatory markers. J Cell Biochem. 2018;119(9):7441–7448.
28. Britti D, Crupi R, Impellizzeri D, et al. A novel composite formulation of palmitoylethanolamide and quercetin decreases inflammation and relieves pain in inflammatory and osteoarthritic pain models. BMC Vet Res. 2017;13(1):229.
29. Hu PF, Chen WP, Bao JP, Wu LD. Paeoniflorin inhibits IL-1beta-induced chondrocyte apoptosis by regulating the Bax/Bcl-2/caspase-3 signaling pathway. Mol Med Rep. 2018;17(4):6194–6200.
30. Zhao L, Chang Q, Huang T, Huang C. Paeoniflorin inhibits IL1betainduced expression of inflammatory mediators in human osteoarthritic chondrocyte. Mol Med Rep. 2018;17(2):3306–3311.
31. Cho IA, Kim TH, Lim H, et al. Formononetin antagonizes the interleukin-1beta-induced catabolic effects through suppressing inflammation in primary rat chondrocytes. Inflammation. 2019;42(4):1426–1440.
32. Huh JE, Seo DM, Baek YH, Choi DY, Park DS, Lee JD. Biphasic positive effect of formononetin on metabolic activity of human normal and osteoarthritic subchondral osteoblasts. Int Immunopharmacol. 2010;10(4):500–507.
33. Gabay O, Sanchez C, Salvat C, et al. Stigmasterol: a phytosterol with potential anti-osteoarthritic properties. Osteoarthritis Cartilage. 2010;18(1):106–116.
34. Chen WP, Yu C, Hu PF, Bao JP, Tang JL, Wu LD. Stigmasterol blocks cartilage degradation in rabbit model of osteoarthritis. Acta Biochim Pol. 2012;59(4):537–541.
35. Wang Q, Pan X, Wong HH, et al. Oral and topical boswellic acid attenuates mouse osteoarthritis. Osteoarthritis Cartilage. 2014;22(1):128–132.
36. Haroyan A, Mukuchyan V, Mkrtchyan N, et al. Efficacy and safety of curcumin and its combination with boswellic acid in osteoarthritis: a comparative, randomized, double-blind, placebo-controlled study. BMC Complement Altern Med. 2018;18(1):7.
37. Riis RG, Gudbergsen H, Henriksen M, et al. Synovitis assessed on static and dynamic contrast-enhanced magnetic resonance imaging and its association with pain in knee osteoarthritis: a cross-sectional study. Eur J Radiol. 2016;85(6):1099–1108.
38. Beekhuizen M, Bastiaansen-jenniskens YM, Koevoet W, et al. Osteoarthritic synovial tissue inhibition of proteoglycan production in human osteoarthritic knee cartilage: establishment and characterization of a long-term cartilage-synovium coculture. Arthritis Rheum. 2011;63(7):1918–1927.
39. Heard BJ, Fritzler MJ, Wiley JP, et al. Intraarticular and systemic inflammatory profiles may identify patients with osteoarthritis. J Rheumatol. 2013;40(8):1379–1387.
40. Teunis T, Beekhuizen M, Kon M, Creemers LB, Schuurman AH, van Minnen LP. Inflammatory mediators in posttraumatic radiocarpal osteoarthritis. J Hand Surg Am. 2013;38(9):1735–1740.
41. Scanzello CR, Goldring SR. The role of synovitis in osteoarthritis pathogenesis. Bone. 2012;51(2):249–257.
42. Rock KL, Latz E, Ontiveros F, Kono H. The sterile inflammatory response. Annu Rev Immunol. 2010;28:321–342.
43. Scanzello CR, Plaas A, Crow MK. Innate immune system activation in osteoarthritis: is osteoarthritis a chronic wound? Curr Opin Rheumatol. 2008;20(5):565–572.
44. Kim HA, Cho ML, Choi HY, et al. The catabolic pathway mediated by Toll-like receptors in human osteoarthritic chondrocytes. Arthritis Rheum. 2006;54(7):2152–2163.
45. Lin Y, Liu L, Jiang H, Zhou J, Tang Y. Inhibition of interleukin-6 function attenuates the central sensitization and pain behavior induced by osteoarthritis. Eur J Pharmacol. 2017;811:260–267.
46. Miller RE, Ishihara S, Tran PB, et al. An aggrecan fragment drives osteoarthritis pain through Toll-like receptor 2. JCI Insight. 2018;3(6).
47. Ao P, Zhou ZG, Han YS, Yin LY, Bian XY. [Effect of chloroform extracts from lycopodium clavatum on RF, TNF-α, IL-1β, IL-6 of rats with adjuvant arthritis]. J Inf Tradit Chin Med. 2013;30(3):121–131. Chinese.
48. Jung HW, Jung JK, Son KH, et al. Inhibitory effects of the root extract of dipsacus asperoides C.Y. Cheng et al T.M.Ai on collagen-induced arthritis in mice. J Ethnopharmacol. 2012;139(1):98–103.
49. Kim KR, Jeong CK, Park KK, et al. Anti-inflammatory effects of licorice and roasted licorice extracts on TPA-induced acute inflammation and collagen-induced arthritis in mice. J Biomed Biotechnol. 2010;2010:709378.
50. Honda H, Nagai Y, Matsunaga T, et al. Glycyrrhizin and isoliquiritigenin suppress the LPS sensor toll-like receptor 4/MD-2 complex signaling in a different manner. J Leukoc Biol. 2012;91(6):967–976.
51. Persson MSM, Sarmanova A, Doherty M, Zhang W. Conventional and biologic disease-modifying anti-rheumatic drugs for osteoarthritis: a meta-analysis of randomized controlled trials. Rheumatology (Oxford). 2018;57(10):1830–1837.
52. Miller RE, Belmadani A, Ishihara S, et al. Damage-associated molecular patterns generated in osteoarthritis directly excite murine nociceptive neurons through Toll-like receptor 4. Arthritis Rheum. 2015;67(11):2933–2943.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.