Back to Journals » Therapeutics and Clinical Risk Management » Volume 16
Validation of a 10-Point Scoring System for Treatment of Cesarean Scar Pregnancy
Authors Tan TT, Sun QL, Luo L , Chen Z, Xiong X, Xiang JH, Yan P, Gao CY, Chen ZQ
Received 28 December 2019
Accepted for publication 13 April 2020
Published 15 May 2020 Volume 2020:16 Pages 429—436
DOI https://doi.org/10.2147/TCRM.S243999
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Video abstract presented by Tingting Tan.
Views: 674
Ting-Ting Tan, Qiu-Lei Sun, Li Luo, Zhu Chen, Xi Xiong, Jin-Hong Xiang, Ping Yan, Chun-Yan Gao, Zheng-Qiong Chen
Department of Obstetrics and Gynecology, The Second Affiliated Hospital of Army Medical University, Chongqing 400037, People’s Republic of China
Correspondence: Zheng-Qiong Chen
Department of Obstetrics and Gynecology, The Second Affiliated Hospital of Army Medical University, Chongqing 400037, People’s Republic of China
Tel +86-23-6877-4012
Email [email protected]
Purpose: To validate a 10-point scoring system for the prediction of successful treatment modality in patients with cesarean scar pregnancy (CSP).
Patients and Methods: Data were collected from women seen between April 1, 2018, and June 30, 2019, at the Second Affiliated Hospital of Army Medical University of China who were diagnosed with CSP and underwent evacuation, followed by uterine artery embolization (UAE) and successive laparoscopic local resection as salvage treatment if necessary. A score was computed based on clinical and ultrasonographic parameters included in a previously developed scoring system. Treatment indicated by the scoring system was compared with actual treatment received. Receiver operating characteristic (ROC) curves were used to identify cut-off scores for salvage treatment.
Results: Of 183 women, 108 were successfully treated by evacuation, 57 required UAE, and 18 eventually underwent laparoscopic surgery. Among 97 women scoring 0– 4, 89 (91.8%) were treated by evacuation only. Of 69 women scoring between 5 and 7, 44 (63.8%) needed UAE following evacuation. Of 17 women scoring 8– 10, 10 women (58.8%) underwent laparoscopic surgery. A cut-off of 4.145 was obtained by ROC curve for prediction of any salvage treatment; this was comparable to the scale’s conventional cut-off of 4. The cut-off score for women requiring laparoscopic surgery was 6.580, which was lower than 8 obtained in the scale’s initial validation.
Conclusion: The overall performance of the 10-point scoring system was moderate for predicting successful treatment modalities of women with CSP, but the scale showed good predictive ability in recognizing women needing only evacuation before recovery.
Keywords: cesarean scar pregnancy, 10-point scoring system, validation, evacuation
Introduction
Cesarean scar pregnancy (CSP) is a special pregnancy in which the gestational sac is dislocated into the myometrium and fibrous tissue surrounding a previous cesarean section scar.1 CSP was first identified in 1978,2 and its reported incidence has increased dramatically since then, paralleling both the rising prevalence of cesarean delivery and advances in CSP diagnosis.3 The global incidence of CSP was recently estimated as between 1 in 3000 and 1 in 1800 pregnancies.4 In China, the rate of CSP is likely increasing with the “two-child policy” under which a large number of women with a prior cesarean section have become pregnant again.
Because of the particular site of gestational sac implantation in CSP, it is often accompanied by life-threatening complications such as uterine rupture and catastrophic hemorrhage in the absence of rapid diagnosis and treatment. Furthermore, because CSP is frequently asymptomatic or characterized by symptoms not specific to the condition in its early stages, diagnosis is based principally on sonography and magnetic resonance imaging.5 Although various treatments exist,6,7 there is no overall consensus for the management of CSP. It has been reported that optimal therapeutic effects are generally achieved through a surgical rather than a medication-based approach.8 Applying an identical management strategy for CSP regardless of its severity will inevitably lead to inadequate or excessive treatment of some cases. Individualized treatment should therefore be employed for different patients based on severity; however, no established guidelines exist for the selection of treatment modalities.
In 2018, Sun et al9 developed a 10-point scoring system to evaluate the severity of CSP and to predict therapeutic outcomes. The scoring system considers six factors affecting severity: number of previous cesarean sections, maximum diameter of the gestational sac, grading of Doppler signals, appearance of fetal heartbeat, thickness of remnant myometrium, and type of gestational sac implantation. Among the six factors, the grading of Doppler signals was divided into three grades according to Adler et al,10 and the type of gestational sac implantation was classified as superficial type, partial type, and complete type.11 The remnant myometrial thickness was graded by 1 mm and 3 mm. The diameter of the gestational sac was graded by 25 mm. The number of previous cesarean deliveries included one, two, and three times. Each grade of the six factors was given a value (Table 1). An overall score ranging from 0 to 10 is assigned based on the different proportions of these six factors, as described in Table 1. Management decisions can then be based on the resulting score: a score of 0–4 (low risk) suggests suction evacuation – the simplest and most minimally invasive treatment for early pregnancy termination; a score ranging from 5 to 7 (moderate risk) suggests uterine artery embolization (UAE) – a treatment minimizing risk of heavy bleeding; and a score of 8–10 (high risk) indicates that surgical management such as laparoscopic lesion resection/hysterectomy will likely be necessary. However, the risk scoring system was validated in the same sample population in which it was developed, which may lead to an overestimation of the scale’s validity.9 Accordingly, we performed a validation of the 10-point scoring system using data from a different population in a different time period and further explored its value in clinical application.
 |
Table 1 10-Point Scoring System for Assessing the Severity of Cesarean Scar Pregnancya |
Patients and Methods
Data were collected retrospectively from all consecutive women diagnosed with CSP and treated in the Second Affiliated Hospital of Army Medical University of China between April 1, 2018 and June 30, 2019. Patients who had been transferred following unsuccessful treatment in local clinics or other hospitals were excluded, as were patients with serious diseases of vital organs. All patients were informed of the procedures and signed a consent form before surgery about the treatment modality and allowing use of their medical data. The study was approved by the Institutional Review Board of the Second Affiliated Hospital of Army Medical University of China (protocol number 2016-042-01, dated June 6, 2016).
Diagnosis of CSP in our center is based on characteristic ultrasound images: an empty uterine cavity and cervical canal, location of the gestational sac in the anterior wall of the uterine isthmus, with a diminished or absent myometrial layer between the gestational sac and the bladder, and a high-velocity/low-impedance perfusion surrounding the gestational sac.10,11
The treatment procedure used has been described previously.9 Briefly, suction evacuation was carried out in the outpatient department with blood products, uterine balloons, and emergency UAE available. The operations were ceased if vaginal bleeding exceeded 300 mL, in which case UAE was undertaken within 10 minutes with uterine balloons for temporary hemostasis. For women with a residual mass detected by transvaginal ultrasound the day following evacuation, 10 mg mifepristone per day was prescribed and followed up at intervals of 1–2 weeks until serum β-HCG levels dropped to normal and the residual mass disappeared completely. During the follow-up period, UAE and laparoscopic local resection (LLR) were successively undertaken as salvage treatments if there was severe vaginal bleeding jeopardizing the health of the patient, or if vaginal bleeding was accompanied by gradual enlargement of the residual mass. The criteria for recovery were defined as thorough clearance of retained products of conception and return of β-HCG levels to normal. “Successful treatment” referred to the treatment modality eventually required before recovery.
The following data were extracted from the medical record of each study participant: maternal age, gravidity, number of previous abortions (both spontaneous and induced abortions) and cesarean deliveries, gestational age, ultrasound characteristics (presence of fetal cardiac activity, maximum diameter of the gestational sac, minimum thickness of the remnant myometrium between the gestational sac and the bladder, type of gestational sac implantation and grading of Doppler signals12,13), time to negative β-HCG, and time until resolution of residue.
Each patient was classified based on the eventual treatment received (evacuation only, UAE, or LLR). We tested continuous variables for normality. Continuous variables were compared between treatment groups using the Kruskal–Wallis test, and distributions of categorical variables were compared using the Pearson chi-square test. A score was calculated for each patient based on clinical and ultrasonographic parameters included in the 10-point scoring system (Table 1). The appropriate management plan suggested by this score was then compared to the actual treatment approach employed. The association between actual and predicted treatment was evaluated with the contingency coefficient, and the consistency of actual vs predicted treatment was analyzed using the Kappa concordance test. Cut-off scores were then identified for any salvage treatment and for laparoscopic surgery using receiver operating characteristic (ROC) curves, with the maximum Youden index. All analyses were conducted with SPSS version 20.0 (IBM, Armonk, NY, USA); statistical significance was defined as P< 0.05.
Results
A total of 199 women were admitted to the study hospital with CSP during the study period. Ten women who transferred from local clinics following unsuccessful treatment were excluded. Three women with incomplete data on the medical record and another three patients with serious disease of vital organs were excluded. Therefore, 183 patients were included in the analyses. Of these 183 patients, 108 (59.0%) were treated successfully by evacuation, 57 (31.1%) received UAE as a salvage therapy after evacuation, and 18 (9.8%) were treated with laparoscopic surgery as a further salvage measure before recovery (Figure 1). Table 2 shows the participant characteristics and univariate comparisons between the three treatment groups. Overall, patients who received UAE or LLR had significantly higher gestational age, fewer previous cesarean sections, larger gestational sac diameter, smaller remnant myometrial thickness, higher color Doppler signal grade, and longer time to negative β-HCG. Patients receiving more aggressive treatment were also significantly more likely to have a fetal heartbeat and less likely to have a superficial gestational sac location. Finally, patients who received LLR had significantly shorter time to resolution of residue.
 |
Table 2 Clinical and Ultrasonographic Characteristics of Patients by Treatment Group |
 |
Figure 1 Patient flowchart. Abbreviations: CSP, cesarean scar pregnancy; UAE, uterine artery embolization. |
Table 3 shows the scores obtained on the 10-point scoring system for the overall study sample and by treatment group (each whole number score X captures all truncated scores between X – 1 and X). Mean scores were 2.1 ± 1.6, 5.9 ± 1.7, and 7.7 ± 2.3 for the evacuation, UAE, and LLR groups, respectively, indicating that higher scores were generally associated with greater likelihood of salvage treatment. All women with a score of 2 or lower were treated with evacuation only, whereas all women with scores of 8 or higher required UAE or laparoscopic surgery as a salvage treatment.
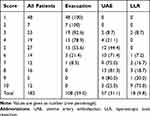 |
Table 3 Scores on the 10-Point Scoring System by Treatment Group |
Table 4 shows the consistency between actual and predicted treatment. Of 97 patients whose scores suggested treatment with evacuation only, 89 were actually treated with evacuation, 6 received UAE, and 2 women required laparoscopic surgery. The prediction accuracy was thus 91.8% (89/97). Of 69 women whose scores indicated UAE following evacuation, 44 received UAE, for a prediction accuracy of 63.8% (44/69). Finally, of 17 women whose scores indicated LLR, 10 women underwent this procedure, for a prediction accuracy of 58.8%. The contingency coefficient and Kappa values for agreement between predicted and actual treatment were 0.645 and 0.610, respectively.
 |
Table 4 Consistency Between Actual and Predicted Therapy |
The area under the ROC curve predicting any salvage treatment (UAE or LLR) after evacuation was 0.947 [95% confidence interval (CI) 0.918–0.976, P< 0.001] (Figure 2). The optimal score cut-off was 4.145, yielding a sensitivity of 0.839 and specificity of 0.824. The area under the curve for predicting laparoscopic surgery was 0.888 (95% CI 0.799–0.976, P< 0.001) (Figure 3). The optimal cut-off score for LLR was 6.580, with a sensitivity of 0.778 and specificity of 0.861.
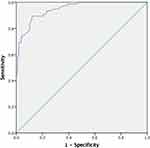 |
Figure 2 Receiver operating characteristic curve for any salvage treatment. |
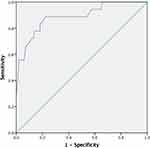 |
Figure 3 Receiver operating characteristic curve for laparoscopic surgery. |
Discussion
In the present study, we validated a previously developed 10-point scoring system for the prediction of treatment modality for CSP.9 To our knowledge, this was the first validation of a scoring system for CSP management. As there is no universal standard for the management of CSP,8 the aim of the 10-point scoring system is to provide a clinical decision-making aide to guide safe and effective individualized treatment. The original development of the scale suggested that women scoring below 4 could be treated successfully with evacuation only.9 This cut-off is similar to the result of 4.145 found in our study. The original cut-off for laparoscopic surgery was 8, somewhat higher than our cut-off of 6.580.
Although the 10-point scoring system obtained a moderate overall consistency between actual and predicted therapy in our study, prediction was very good for women needing only evacuation before recovery. Both in our study and in the original development of this scoring system, the majority of women had low scores, and the ability to identify women requiring only evacuation represents an important strength of the scoring system. Among the various treatment modalities, evacuation is the simplest and most minimally invasive. In the past, it was generally suggested that evacuation should not be regarded as the preferred approach for CSP because of severe complications that often ensued.14,15 However, in recent years, an increasing number of studies have reported that evacuation can be successfully applied in some cases for CSP.16–19 Hence, it is vital to identify those women for whom evacuation is the optimal treatment modality. Cheng et al16 reported that better therapeutic outcomes could be achieved with evacuation in CSP patients who had superficial implantation. By preoperative determination of CSP implantation depth, Cheng et al16 achieved a success rate of 88.5% (23/26) in women with superficial implantation. The depth of implantation represents an important component of the severity of CSP. However, severity cannot be assessed only in terms of implantation depth, especially in the presence of large gestational sac. In contrast, the 10-point scoring system considers multiple variables determining CSP severity and thus yields a more comprehensive evaluation. Wang et al17 developed a scoring system to predict bleeding during suction evacuation of CSP. Fang et al18 also established a scoring system for CSP to guide treatment decisions by retrospectively reviewing records of 82 CSP patients. Their scoring system included five vascularity categories and three pregnancy duration categories, all of which were assigned equal scores. In our 10-point scoring system, the different grades of each prognostic factor were given different weighted numerical values denoting the magnitude of their prediction of eventual treatment. More importantly, neither of the two previously developed scoring systems has been validated in relation to treatment patterns in external populations. Accordingly, the 10-point scoring system provides a relatively detailed and credible metric for predicting successful treatment with evacuation for CSP.
Compared to women who scored at the low end of the scale, prediction efficiency for women with high scores was comparatively poorer. It should be noted that most women scored 4 or below, with fewer than one-third scoring between 5 and 7, and fewer than one-fifth scoring above 7. Based on the principle of minimally invasive treatment, we use UAE (combined with mifepristone) as the first-line salvage treatment and laparoscopic surgery as a second-line treatment in our center. Alternative treatments exist for patients with CSP including hysteroscopy and local resection through a transvaginal approach. Different medical centers generally develop their own practice patterns based on available facilities and expertise, and further research is required to identify optimal treatment for CSP patients who have high-risk scores.
The strength of this study is that it is the first study to validate a score system for CSP management. This validation will contribute to the promotion and use of a 10-point scoring system. The 10-point scoring system could be used in the future as an aide for clinical decision-making in the management of CSP. If applied appropriately and judiciously, the scale could lead to improvements in safety, efficiency and medical resource allocation, and could alleviate some unnecessary burden placed on tertiary referral centers. The identification of an optimal cut-off score for women needing only evacuation is of substantial clinical significance, especially for suburban and community hospitals, which transfer almost all CSP cases to tertiary care centers because of safety concerns regarding complications from evacuation. In the present study, all women scoring below 3 were managed successfully by evacuation. Therefore, for suburban and community hospitals, a cut-off of 2 or lower can be safely applied as an indication for evacuation. In addition, expectant management should be explored as a possibility for women with low CSP severity scores who wish to continue their pregnancy.
However, several limitations to our study must be acknowledged. First, the study population came from a single medical center, and it is likely that treatment practice patterns would differ at other institutions (as discussed above). On a related note, the salvage treatment procedure at our institution is UAE followed by laparoscopic surgery, which would not be suitable at all medical centers. We recommend that future research explore the optimal salvage modality in relation to severity of CSP and in light of institutional characteristics and clinician expertise and experience. Finally, universal termination of CSP does not constitute optimal clinical practice, and a policy of “watch and wait” may be indicated in cases of CSP with low severity scores. Before wider application of the 10-point CSP severity scale, its efficacy for the prediction of optimal treatment and effects on pregnancy outcomes should undergo further validation.
In conclusion, although the performance of the 10-point scoring system was moderate overall for predicting successful treatment modalities of women with CSP, predictive ability was relatively good for identifying women who required only evacuation before recovery. Women who scored 4 or lower were most effectively treated by evacuation without further salvage treatment. The ascertainment of this cut-off score adds to the evidence base supporting evacuation as a first-line treatment for low-risk CSP. Nevertheless, before the 10-point scoring system is more widely applied in clinical practice, further validation is required in larger samples across multiple clinical centers.
Data Sharing Statement
The data used during this study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The procedures in this study involving human were consistent with the 1964 Helsinki Declaration and its amendments, comparable ethical standard. All patients signed a consent form before surgery about the treatment modality and allowing the use of their medical data. Ethical approval was obtained from the Institutional Review Board of the Second Affiliated Hospital of Army Medical University of China.
Author Contributions
All authors contributed to data analysis and drafting and revising this article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This study was funded by the Science and Hygiene Joint Medical Research Project of Chongqing (grant No.2018ZDXM034, 2018QNXM033) and by the Second Affiliated Hospital of Army Medical University (2019JSLC011).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Rotas MA, Haberman S, Levgur M. Cesarean scar ectopic pregnancies: etiology, diagnosis, and management. Obstet Gynecol. 2006;107:1373–1381. doi:10.1097/01.AOG.0000218690.24494.ce
2. Larsen JV, Solomon MH. Pregnancy in a uterine scar sacculus: an unusual cause of postabortal haemorrhage. A case report. S Afr Med J. 1978;53:142–143.
3. Timor-Tritsch IE, Monteagudo A. Unforeseen consequences of the increasing rate of cesarean deliveries: early placenta accreta and cesarean scar pregnancy. A review. Am J Obstet Gynecol. 2012;207:14–29. doi:10.1016/j.ajog.2012.03.007
4. Kanat-Pektas M, Bodur S, Dundar O, Bakır VL. Systematic review: what is the best first-line approach for cesarean section ectopic pregnancy? Taiwanese J Obstet Gynecol. 2016;55:263–269. doi:10.1016/j.tjog.2015.03.009
5. Gonzalez N, Tulandi T. Cesarean scar pregnancy: a systematic review. J Minim Invasive Gynecol. 2017;24:731–738. doi:10.1016/j.jmig.2017.02.020
6. Litwicka K, Greco E. Caesarean scar pregnancy: a review of management options. Curr Opin Obstet Gynecol. 2013;25:456–461. doi:10.1097/GCO.0000000000000023
7. Timor-Tritsch IE, Monteagudo A, Santos R, Tsymbal T, Pineda G, Arslan AA. The diagnosis, treatment, and follow-up of cesarean scar pregnancy. Am J Obstet Gynecol. 2012;207:
8. Birch Petersen K, Hoffmann E, Rifbjerg Larsen C, Svarre Nielsen H. Cesarean scar pregnancy: a systematic review of treatment studies. Fertil Steril. 2016;105:958–967. doi:10.1016/j.fertnstert.2015.12.130
9. Sun QL, Luo L, Gao CY, Yan P, Yang Y, Chen ZQ. Scoring system for the prediction of the successful treatment modality in women with cesarean scar pregnancy. Int J Gynaecol Obstet. 2019;146:1–7. doi:10.1002/ijgo.12881
10. Sun QL, Wu XH, Luo L, Ying DM, Yang Y, Chen ZQ. Characteristics of women with mixed mass formation after evacuation following uterine artery chemoembolization for cesarean scar pregnancy. Arch Gynecol Obstet. 2018;297:1059–1066. doi:10.1007/s00404-018-4716-6
11. Adler DD, Carson PL, Rubin JM, Quinn-Reid D. Doppler ultrasound color flow imaging in the study of breast cancer: preliminary findings. Ultrasound Med Biol. 1990;16:553–559. doi:10.1016/0301-5629(90)90020-D
12. Jurkovic D, Hillaby K, Woelfer B, Lawrence A, Salim R, Elson C. First-trimester diagnosis and management of pregnancies implanted into the lower uterine segment Cesarean section scar. Ultrasound Obstet Gynecol. 2003;21:220–227. doi:10.1002/uog.56
13. Pascual MA, Hereter L, Graupera B, Tresserra F, Fernandez-Cid M, Simon M. Three-dimensional power Doppler ultrasound diagnosis and conservative treatment of ectopic pregnancy in a cesarean section scar. Fertil Steril. 2007;88:
14. Seow KM, Huang LW, Lin YH, Lin MY, Tsai YL, Hwang JL. Cesarean scar pregnancy: issues in management. Ultrasound Obstet Gynecol. 2004;23:247–253. doi:10.1002/uog.974
15. Shih JC. Cesarean scar pregnancy: diagnosis with three-dimensional (3D) ultrasound and 3D power Doppler. Ultrasound Obstet Gynecol. 2004;23:306–307. doi:10.1002/uog.1000
16. Cheng LY, Wang CB, Chu LC, Tseng CW, Kung FT. Outcomes of primary surgical evacuation during the first trimester in different types of cesarean scar pregnancy. Fertil Steril. 2014;102:1085–90.e2. doi:10.1016/j.fertnstert.2014.07.003
17. Wang Q, Ma H, Peng H, He L, Bian C, Zhao X. Risk factors for intra-operative haemorrhage and bleeding risk scoring system for caesarean scar pregnancy: a case-control study. Eur J Obstet Gynecol Reprod Biol. 2015;195:141–145. doi:10.1016/j.ejogrb.2015.06.023
18. Fang QX, Sun L, Tang YH, Qian CF, Yao XY. Quantitative risk assessment to guide the treatment of cesarean scar pregnancy. Int J Gynaecol Obstet. 2017;139:78–83. doi:10.1002/ijgo.12240
19. Le AW, Li MX, Xu YH, et al. Different surgical approaches to 313 cesarean scar pregnancies. J Minim Invasive Gynecol. 2019;26:148–152. doi:10.1016/j.jmig.2018.03.035
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
