Back to Journals » International Journal of General Medicine » Volume 9
Utilizing a medical questionnaire to predict anxiety and depression in outpatients
Authors Kajiwara H, Ohira Y , Ikegami A , Hanazawa N, Masuyama T, Yamashita T, Kondo T , Shikino K , Ikusaka M
Received 30 November 2015
Accepted for publication 21 March 2016
Published 11 June 2016 Volume 2016:9 Pages 199—204
DOI https://doi.org/10.2147/IJGM.S101556
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hideki Kajiwara,1 Yoshiyuki Ohira,1 Akiko Ikegami,1 Nao Hanazawa,1 Takako Masuyama,1,2 Tomoko Yamashita,1 Takeshi Kondo,1 Kiyoshi Shikino,1 Masatomi Ikusaka1
1Department of General Medicine, Chiba University Hospital, Chiba-shi, 2Department of General Medicine, Kimitsu Chuo Hospital, Kisarazu-shi, Chiba, Japan
Introduction: Anxiety and depressive symptoms are seen in patients with anxiety and mood disorders but are also common in those with organic disorders. However, since physical symptoms are predominant complaints from patients who visit nonpsychiatric outpatient clinics, anxiety and depressive symptoms are often unrecognized. It is important for physicians to be aware of these issues concurrent with the physical symptoms. We therefore examined whether a self-administered medical questionnaire could identify anxiety and depressive symptoms.
Patients and methods: A total of 453 patients on their first visit to the Department of General Medicine, Chiba University Hospital, Chiba, Japan, participated in this study. They were asked to complete a medical questionnaire and the Hospital Anxiety and Depression Scale questionnaire before examination. Data on age, sex, number of complaints, symptom duration, and number of previous physicians were extracted from the medical questionnaire. These data were used as independent variables in logistic regression analysis to develop a predictive model for the presence of anxiety and depressive symptoms.
Results: Data from 358 (79.0%) patients were included in the analyses. Logistic regression analysis identified the following predictors: “three or more complaints” (odds ratio [OR] 2.39; 95% confidence interval [CI] 1.48–3.88) and “four or more previous physicians” (OR 1.72; 95% CI 1.10–2.69). In the predictive model for the presence of symptoms of anxiety and depression, the likelihood ratio was 2.40 (95% CI 1.33–4.34) in patients reporting both conditions and 1.35 (95% CI 1.04–1.77) in those reporting either condition.
Conclusion: The presence of anxiety and depressive symptoms can be predicted from the items of a medical questionnaire in outpatients visiting a general medicine department of a university hospital. When patients report three or more complaints or four or more previous physicians on a medical questionnaire, physicians should consider the presence of anxiety or depression or both in differential diagnosis.
Keywords: anxiety, depression, Hospital Anxiety and Depression Scale, HADS, complaint numbers, number of previous physicians, medical questionnaire
Introduction
Representative diseases with anxiety and depressive symptoms are anxiety disorders and mood disorders. Both are considered as common diseases with high lifetime prevalence.1 Symptoms of anxiety and depression commonly develop in other psychiatric disorders2–7 and may also develop in physical disorders, including heart disease, central nervous system disease, diabetes mellitus, and cancer.8 When patients with such disorders visit primary care outpatient clinics or hospital outpatient departments of general medicine, physical, rather than anxiety and depressive, symptoms are the predominant complaints. However, ∼30% of patients visiting primary care physicians with chief physical complaints have depression or anxiety disorders.9
Anxiety and depressive symptoms are common in patients with various diseases; however, they are infrequently reported voluntarily by patients and typically unrecognized in nonpsychiatric outpatient clinics. For example, the diagnostic rates of anxiety and mood disorders are as low as 20%–30% in primary care outpatient clinics and hospital outpatient departments of general medicine.10,11 To avoid overlooking these disorders, physicians must be aware of anxiety and depressive symptoms concurrent with physical symptoms. Once suspicions are raised, it is not difficult for even nonpsychiatric physicians to detect the presence of anxiety and depressive symptoms; several convenient tools have been developed to readily evaluate anxiety and depressive symptoms, such as the Hospital Anxiety and Depression Scale (HADS).12–21
Anxiety disorder and depression are known to be predicted by age, sex, number of complaints, number of medical facilities the patients had visited for similar complaints (hereinafter referred to as “number of previous physicians”), education level, occupational history, familial history of psychiatric disorders, and others.22
Patients and methods
Patients and setting
A total of 453 patients on their first visit to the Department of General Medicine, Chiba University Hospital, Chiba, Japan (hereinafter “our department”) during the 6 months after October 2012 were included in the study. They were asked to complete the medical questionnaire and the HADS questionnaire before medical evaluation.
The medical questionnaire was the same as that previously used in our department before initiation of the present study. This questionnaire contained open-ended questions for symptoms and closed-ended questions for the other items (age, sex, symptom duration, past medical history, history of allergy, social history, smoking history, alcohol history, and pregnancy status). We extracted the following five items that are expected to predict anxiety and depressive symptoms based on previous studies: age, sex, number of complaints, symptom duration, and number of previous physicians.22,23 Complaints reported in the medical questionnaire were counted and other complaints that a physician elicited during examination were not counted. To count the number of complaints, the International Classification of Primary Care, Second Edition (ICPC-2) was used.24 For example, if the complaints were “sneezing, runny nose, nasal congestion, and sore throat”, sneezing, runny nose, and nasal congestion were counted together as one symptom because they are all nasal symptoms included in the same ICPC-2 code, R07. Sore throat was distinguished from these nasal symptoms because it develops in a site that is anatomically different from the nose and is included in another ICPC-2 code, R21. Therefore, the number of complaints for this patient was counted as two. If a patient had several complaints classified into “others” in the ICPC-2, each of the complaints was counted as one. For example, if the complaints were “ascites and bruxism”, which are both included in the code D29, the number of complaints was counted as two.
The HADS comprises 14 questions in total, each scored from 0 to 3. It has two subscales: A scores assess anxiety symptoms and D scores assess depressive symptoms. Scores for each subscale range from 0 to 21, with scores categorized as follows: normal (noncases; 0–7), doubtful cases (8–10), and definite cases (11–21). These cutoff scores were determined for outpatients who suffered from a wide variety of complaints and illnesses.12 In the present study, patients with ≥8 points on A or D scores or both were placed in the anxiety/depression group and the other patients were placed in the control group.
The present study was approved by the ethics committee of the Graduate School of Medicine, Chiba University, and was conducted with those who provided informed consent to participate in the study. Chiba City, where the Chiba University Hospital is located, is a major city in the metropolitan Tokyo area and is 40 minutes from Tokyo by train. Our department mainly accepts referral patients (where diagnosis is not established), and the patient referral rate was 88.6% in 2012 when the study was conducted.
Statistical analyses
Receiver operating characteristic curves were generated to identify the association of the number of complaints, symptom duration, and number of previous physicians with the anxiety/depression group. Youden’s index was used to select the optimal cutoff values of the receiver operating characteristic curves. Then, multiple logistic regression analyses with a forward selection (likelihood ratio [LR]) procedure were performed to identify predictors for the presence of anxiety and depressive symptoms with the dependent variables “anxiety/depression group” and “control group”, respectively. The following independent variables were included: age, sex, number of complaints, symptom duration, and number of previous physicians. Before regression analyses, variance inflation factors were calculated to test multicollinearity.
The performance of the predictive model was assessed with the use of discrimination and calibration for goodness of fit; discrimination was evaluated with the use of the concordance index (c-index), and calibration was assessed with the use of the Hosmer–Lemeshow test. The model was internally validated with 1,000 bootstrap samples. All statistical analyses were performed using SPSS Statistics for Windows 22.0 (IBM Corporation, Armonk, NY, USA) and a significance threshold of 0.05.
Results
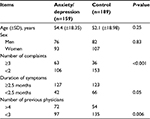
Of 453 patients, 83 who did not receive the HADS questionnaire, ten who did not complete the HADS questionnaire, one who did not complete the medical questionnaire, and one who did not consent to participate were excluded from this study. Thus, data from 358 (79.0%) patients (158 men and 200 women) were analyzed. For an exact statistical analysis, the rule of thumb is ten events per variable in the logistic regression.25 The minimum number of events required was 50 (5×10=50), and the actual number of events was 169 in this study; therefore, the sample size of this study followed the rule. The cutoff value for number of complaints was ≥3 (area under the curve [AUC] 0.60; 95% confidence interval [CI] 0.54–0.66). The cutoff value for symptom duration was ≥2.5 months (AUC 0.56; 95% CI 0.50–0.62). The cutoff value for number of previous physicians was ≥4 (AUC 0.57; 95% CI 0.51–0.63). Table 1 shows the comparison between the anxiety/depression and control groups. The anxiety/depression group had significantly greater proportions of patients who had three or more complaints (P<0.001) and those who had visited four or more physicians (P=0.006) compared with the control group.
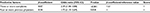
Logistic regression analysis was performed using age, sex, number of complaints, symptom duration, and number of previous physicians as independent variables. Variance inflation factor values were 1.03 for age, 1.02 for sex, 1.04 for number of complaints, 1.09 for symptom duration, and 1.09 for number of previous physicians; none of the variables showed a significant linear relationship, indicating the absence of multicollinearity. Logistic regression analysis revealed the following independent predictors of having anxiety and depressive symptoms: three or more complaints (odds ratio [OR] 2.39; 95% CI 1.48–3.88; P<0.001) and four or more previous physicians (OR 1.72; 95% CI 1.10–2.69; P=0.018; Table 2).
  | Table 2 Logistic regression analysis Notes: A P-value less than 0.05 was considered statistically significant. Abbreviation: 95% CI, 95% confidence interval. |
The Hosmer–Lemeshow goodness-of-fit test indicated good calibration (P=0.875). The discrimination was also excellent (c-index 0.628; 95% CI 0.571–0.686). The model was internally validated using a bootstrap method; the bootstrap-corrected c-index was 0.628 (95% CI 0.575–0.685). Based on the regression coefficient results, three or more complaints and four or more previous physicians were each given 1 point as a scoring method. Table 3 shows LRs in patients with different scores. Patients with 1 point (LR 1.35; 95% CI 1.04–1.77) or 2 points (LR 2.40; 95% CI 1.33–4.34) were likely to have anxiety and depressive symptoms, while patients with 0 point (LR 0.63; 95% CI 0.50–0.79) were unlikely to have anxiety and depressive symptoms.
  | Table 3 LRs in patients with different scores Abbreviations: LRs, likelihood ratios; 95% CI, 95% confidence interval. |
Discussion
We showed that patients reporting three or more complaints, four or more previous physicians, or both were likely to have anxiety and depressive symptoms. Additionally, patients reporting neither of these were unlikely to have anxiety and depressive symptoms. One feature of the present study is that this is the first study to report an association between information from medical questionnaires used in clinical settings and detection of anxiety and depressive symptoms.
One study in primary care patients using the Patient Health Questionnaire-15 (PHQ-15),26 which is a questionnaire used to assess physical symptoms, reported that the prevalence of anxiety disorder and depression increased with the increasing numbers of physical symptoms.27 However, it is difficult to apply the results of this study to medical questionnaires because open-ended questions are commonly used to assess outpatient complaints in medical questionnaires. No previous studies have investigated the association between the number of complaints in an open-ended medical questionnaire and detection of anxiety and depressive symptoms. One similar study was conducted with the use of the number of complaints reported by patients during medical interviews.28 The study reported that patients with three or more complaints were likely to have depressive symptoms, but did not mention the reason for setting the cutoff value at 3 or the association with anxiety symptoms. In the present study, when there were three or more complaints in the medical questionnaire, the patient was predicted to have anxiety and depressive symptoms; therefore, reporting three or more complaints was a relatively easy-to-use measure in outpatient practice.
Another noteworthy feature of the present study is that it was conducted in patients who visited a university hospital, while the abovementioned previous studies were conducted in primary care.27,28 Patients visiting a primary care outpatient clinic frequently present with chief physical complaints resulting from mental disorders, such as depression. In contrast, a general medicine outpatient department of a university hospital is a tertiary medical center to which many patients are referred for diagnostic purposes; therefore, such patients often have symptoms of anxiety and depression secondary to persistent symptoms caused by their undiagnosed diseases. Thus, the present study is of significance for indicating the association between the number of complaints and detection of anxiety and depressive symptoms in patients who visited a general medicine department of a university hospital.
We also showed that number of previous physicians was predictive for anxiety and depressive symptoms. This result was consistent with that of a previous study reporting that high utilizers of medical care (the so-called doctor-shopping patients, who visit multiple clinics for the same complaints without a referral) frequently had depression and generalized anxiety disorders.29 However, four or more previous physicians was identified as a predictor in the current study, whereas the definition of doctor shopping used in the previous studies in Japan was “visiting two or more medical facilities for the same medical complaints without a referral”.30,31 One of the reasons could be that in Japan, it is not unusual for patients to visit two or three medical facilities for the same complaints because the so-called free access medical system allows patients to choose their preferred medical providers with the cost covered by the public insurance. Since we found evidence that reporting three or less previous physicians did not predict anxiety and depressive symptoms in the patient, the definition of doctor shopping should be discussed further in Japan.
More than 30,000 people in Japan suicide each year, and suicide is a critical social issue which the government has been taking measures to address.32 Hirokawa et al33 reported that risk factors for suicide in Japan included depression, anxiety disorder, and alcohol dependence. One study reported that among people who committed suicide, 30% had mood disorder and 5% had anxiety disorder.34 In addition, Luoma et al35 reported that 45% of persons who committed suicide contacted primary care providers within 1 month before suicide, whereas 19% contacted mental health services; this indicates the important role of nonpsychiatric physicians in suicide prevention. A patient reporting more complaints or more previous physicians may have anxiety and depressive symptoms concurrent with their physical symptoms. With this in mind, nonpsychiatric physicians can appropriately recognize a patient with anxiety and mood disorders in outpatient settings and thereby may contribute to a reduction in suicide rates.
Limitations
First, this study was conducted in patients who visited a general medicine outpatient department of a university hospital. The results may not be applicable to outpatients visiting specialized departments, visited by many patients with organic disorders, including endocrine and collagen diseases, because these patients tend to have many complaints. Second, the number of complaints was counted using the ICPC-2 code system. Reference to the ICPC-2 codes may be impractical in a busy clinical setting. Counting the number of complaints may depend on physician’s skills, and considerable variation may be observed in the number of complaints. Third, we did not use a structured psychiatric interview for assessment and thus could not reveal the association between medical questionnaire data and final diagnosis. Finally, because of the small sample size, we could not exclude the possibility of beta error that age, sex, and symptom duration could be associated with anxiety and depressive symptoms in a larger sample size.
Conclusion
The presence of anxiety and depressive symptoms can be predicted by the information derived from a medical questionnaire in outpatients visiting a general medicine department of a university hospital. When patients report three or more complaints, four or more previous physicians, or both on a medical questionnaire, physicians should consider the presence of anxiety or depression.
Author contributions
All authors contributed toward data analysis, drafting, and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Ishikawa H, Kawakami N, Kessler RC; World Mental Health Japan Survey Collaborators. Lifetime and 12-month prevalence, severity and unmet need for treatment of common mental disorders in Japan: results from the final dataset of World Mental Health Japan Survey. Epidemiol Psychiatr Sci. 2015;7:1–13. | ||
Buckley PF, Miller BJ, Lehrer DS, Castle DJ. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009;35(2):383–402. | ||
Patra BN, Sarkar S. Adjustment disorder: current diagnostic status. Indian J Psychol Med. 2013;35(1):4–9. | ||
Amerio A, Stubbs B, Odone A, Tonna M, Marchesi C, Ghaemi SN. The prevalence and predictors of comorbid bipolar disorder and obsessive-compulsive disorder: a systematic review and meta-analysis. J Affect Disord. 2015;186:99–109. | ||
Pinto A, Mancebo MC, Eisen JL, Pagano ME, Rasmussen SA. The Brown Longitudinal Obsessive Compulsive Study: clinical features and symptoms of the sample at intake. J Clin Psychiatry. 2006;67(5):703–711. | ||
Moss HB, Chen CM, Yi HY. Prospective follow-up of empirically derived alcohol dependence subtypes in wave 2 of the national epidemiologic survey on alcohol and related conditions (NESARC): recovery status, alcohol use disorders and diagnostic criteria, alcohol consumption behavior, health status, and treatment seeking. Alcohol Clin Exp Res. 2010;34(6):1073–1083. | ||
Löwe B, Spitzer RL, Williams JB, Mussell M, Schellberg D, Kroenke K. Depression, anxiety and somatization in primary care: syndrome overlap and functional impairment. Gen Hosp Psychiatry. 2008;30(3):191–199. | ||
Evans DL, Charney DS, Lewis L, et al. Mood disorders in the medically ill: scientific review and recommendations. Biol Psychiatry. 2005;58(3):175–189. | ||
Kroenke K, Jackson JL, Chamberlin J. Depressive and anxiety disorders in patients presenting with physical complaints: clinical predictors and outcome. Am J Med. 1997;103(5):339–347. | ||
Vermani M, Marcus M, Katzman MA. Rates of detection of mood and anxiety disorders in primary care: a descriptive, cross-sectional study. Prim Care Companion CNS Disord. 2011;13(2):e1–e10. | ||
Nakane Y, Michijutsi S. Results from the Nagasaki Centre. In: Üstün TB, Sartorius N, editors. Mental Illness in General Health Care: An International Study. Chichester: John Wiley and Sons; 1995:193–210. | ||
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. | ||
Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. | ||
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. | ||
Arroll B, Khin N, Kerse N. Screening for depression in primary care with two verbally asked questions: cross sectional study. BMJ. 2003;327(7424):1144–1146. | ||
Skapinakis P. The 2-item generalized anxiety disorder scale had high sensitivity and specificity for detecting GAD in primary care. Evid Based Med. 2007;12(5):149. | ||
Zigmond AS, Snaith RP, Kitamura T. Hospital Anxiety and Depression Scale (HAD-Shakudo). Arch Psychiatr Diagn Clin Eval. 1993;4:371–372. [translation; in Japanese]. | ||
Hatta H, Higashi A, Yashiro H, et al. A validation of the Hospital Anxiety and Depression Scale. Jpn J Psychosom Med. 1998;38(5):309–315. [in Japanese with English abstract]. | ||
Higashi A, Yashiro H, Kiyota K. Validation of the Hospital Anxiety and Depression scale in a gastro-intestinal clinic. Nihon Shokakibyo Gakkai Zasshi. 1996;93(12):884–892. [in Japanese with English abstract]. | ||
Muramatsu K, Miyaoka H, Kamijima K, et al. The patient health questionnaire, Japanese version: validity according to the mini-international neuropsychiatric interview-plus. Psychol Rep. 2007;101(3 Pt 1):952–960. | ||
Inagaki M, Ohtsuki T, Yonemoto N, et al. Validity of the Patient Health Questionnaire (PHQ)-9 and PHQ-2 in general internal medicine primary care at a Japanese rural hospital: a cross-sectional study. Gen Hosp Psychiatry. 2013;35(6):592–597. | ||
King M, Walker C, Levy G, et al. Development and validation of an international risk prediction algorithm for episodes of major depression in general practice attendees: the PredictD Study. Arch Gen Psychiatry. 2008;65(12):1368–1376. | ||
Hinz A, Kittel J, Karoff M, Schwarz R. Age and sex dependencies of anxiety and depression in cardiologic patients compared with the general population. Psychosoc Med. 2004;1:1–7. | ||
World Health Organization. International Classification of Primary Care (ICPC-2). WONCA International Classification Committee. Oxford: Oxford University Press; 1998. | ||
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–1379. | ||
Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64(2):258–266. | ||
Kroenke K, Spitzer RL, Williams JB, et al. Physical symptoms in primary care. Predictors of psychiatric disorders and functional impairment. Arch Fam Med. 1994;3(9):774–779. | ||
Gerber PD, Barrett JE, Barrett JA, et al. The relationship of presenting physical complaints to depressive symptoms in primary care patients. J Gen Intern Med. 1992;7(2):170–173. | ||
Pilowsky I, Smith QP, Katsikitis M. Illness behaviour and general practice utilisation: a prospective study. J Psychosom Res. 1987;31(2):177–183. | ||
Yamada M, Soejima S, Emura S, Koizumi S. Doctor shopping behavior with psychological distress: a survey using ICPC-2 and COOP/WONCA Charts in Japan. Jpn J Prim Care. 2006;29(2):85–90. | ||
Ohira Y, Ikusaka M, Noda K, et al. Consultation behaviour of doctor-shopping patients and factors that reduce shopping. J Eval Clin Pract. 2012;18(2):433–440. | ||
Cabinet Office, Government of Japan [webpage on the Internet]. White paper on suicide prevention in Japan. In: Cabinet Office. Government of Japan; 2013. Available from: http://www8.cao.go.jp/jisatsutaisaku/whitepaper/en/w-2013/summary.html. Accessed October 1, 2015. | ||
Hirokawa S, Kawakami N, Matsumoto T, et al. Mental disorders and suicide in Japan: a nation-wide psychological autopsy case-control study. J Affect Disord. 2012;140(2):168–175. | ||
Bertolote JM, Fleischmann A. Suicide and psychiatric diagnosis: a worldwide perspective. World Psychiatry. 2002;1(3):181–185. | ||
Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159(6):909–916. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.