Back to Journals » Open Access Emergency Medicine » Volume 10
Using initial serum lactate level in the emergency department to predict the sustained return of spontaneous circulation in nontraumatic out-of-hospital cardiac arrest patients
Authors Dadeh A , Nuanjaroan B
Received 9 February 2018
Accepted for publication 3 July 2018
Published 26 September 2018 Volume 2018:10 Pages 105—111
DOI https://doi.org/10.2147/OAEM.S165154
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Ar-aishah Dadeh, Banjaparat Nuanjaroan
Department of Emergency Medicine, Songklanagarind Hospital, Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, Thailand
Objective: To examine the initial level of lactate to predict sustained return of spontaneous circulation (ROSC) in nontraumatic out-of-hospital cardiac arrest (OHCA) patients.
Materials and methods: This was a 30-month retrospective cohort study in an emergency department (ED) of a tertiary care hospital. The inclusion criteria were adult nontraumatic OHCA patients who came to the ED with ongoing chest compression. The primary outcome was initial serum lactate level at the ED to predict sustained ROSC in nontraumatic OHCA. Logistic regression was used to determine any association between sustained ROSC and significant variables.
Results: There were 207 patients who met the inclusion criteria. Forty one percent of nontraumatic OHCA patients achieved sustained ROSC. The mean ± SD initial serum lactate in the ROSC group was lower than the non-ROSC group (12.0±4.8 vs 12.6±5), but without statistical significance. The significant factors to predict sustained ROSC were no underlying disease (adjusted odds ratio [aOR] 1.71, 95% CI 0.51–5.71, P=0.014), cardiac arrest in a public area (aOR 2.40, 95% CI 1.2–4.79, P=0.013), and witnessed arrest (aOR 2.39, 95% CI 1.26–4.52, P=0.008). The cut-off points of initial serum lactate to predict mortality at 24 and 48 hours after cardiopulmonary resuscitation were 9.1 (P=0.031) and 9.4 (P=0.049) mmol/L, respectively. Eleven survived to hospital discharge, and 54.5% had good neurological outcome without statistical significance (P=0.553). The significant variables and initial lactate levels were used to develop a scoring system which ranged from –4 to 11. The receiver operating characters curve indicated a cut-off point of 3.6 to predict ROSC with an area under the curve of 0.715.
Conclusion: The initial serum lactate had no association with sustained ROSC and hospital discharge with good neurological outcome but can be used to predict 24- and 48-hour postresuscitation mortality in nontraumatic OHCA patients with initial serum lactate cut-off points of 9.1 and 9.4 mmol/L, respectively.
Keywords: out-of-hospital cardiac arrest, initial serum lactate, sustained return of spontaneous circulation
Background
Cardiac arrest is a major public health problem in many countries. The incidence of cardiac arrest varies from 0.5 to 1.5/1,000 people/year.1 The survival rates for cardiopulmonary resuscitation (CPR) generally depend on the location of cardiac arrest.2 The survival rates remain low (10.4%) in adult patients who suffer from out-of-hospital cardiac arrest (OHCA) and received resuscitative procedures from an emergency medical system.3
When sudden cardiac arrest occurs, it means sudden cessation of cardiac function with hemodynamic collapse leading to anaerobic metabolism. Lactate is the end product of anaerobic metabolism4 that can be used as a marker of cellular hypoxia in several shock states and can use to predict mortality in many critical diseases such as sepsis, burns, and trauma.5–11 In cardiac arrest patients who survive from CPR, post-cardiac arrest, the serum lactate can be used as a surrogate marker for tissue perfusion and evidence of utility of lactate to predict survival to hospital discharge.12,13 High serum lactate or slow serum lactate clearance rate after return of spontaneous circulation (ROSC) was correlated with poor outcomes. The serum lactate level within 10 minutes after CPR is a good indicator of prognosis, but the cut-off points to use for determining outcome in OHCA patients vary from study to study.13–16
The present study aimed to determine the serum lactate level as a predictor for sustained ROSC in OHCA in emergency department (ED) patients.
Materials and methods
Study design and setting
This was an observational, retrospective study. The data were collect from January 1, 2015, to June 30, 2017. The inclusion criteria were 18-year-old patients or older who suffered from OHCA and received CPR until they achieved sustained ROSC. Sustained ROSC was defined as the presence of palpable pulses for at least 20 minutes.17 The exclusion criteria were traumatic cardiac arrest, ROSC prior to arrival, and pregnancy.
Songklanagarind Hospital is a tertiary university hospital. The ED volume is over 45,000 patients/year. The number of cardiac arrest patients who received CPR at the ED is 170 patients/year. One hundred and forty-three had OHCA and 27 patients had cardiac arrest at the ED. The hospital CPR team consists of an internal medicine physician, surgeon, anesthesiologist, and emergency physician. Our hospital uses the practice guidelines of the American Heart Association. Blood samples were drawn for the initial lactate level using the enzymatic method. The study was approved by the institutional ethics committee board of Prince of Songkla University.
Outcome measurements
The primary outcome measure was the initial serum lactate level which was used at the ED to predict sustained ROSC in nontraumatic OHCA. The secondary outcome was the association between initial serum lactate level and 24- and 48-hour mortality and hospital discharge with good neurological outcome. Good neurological outcome was defined as Glasgow–Pittsburgh cerebral performance category (CPC) score category 1 or 2.18
Statistical analysis
The statistical analysis was done using R Software version 3.2.2 (The R Foundation, Vienna, Austria). The continuous variables were analyzed and reported as mean and median, while categorical variable were reported as percentage. The Student’s t-test was used for continuous and ordinal variables and the Pearson’s χ2 test was used for categorical variables. Multivariate logistic regression model was used to predict factors for sustained ROSC. We determined the predicting factors for ROSC by backward stepwise logistic regression. Adjustment was made for potential confounding variables that were significant (P<0.05) or tended toward significance (P<0.02) on univariate analysis. The coefficiency from the model was multiplied by 4 and all factors were summed to calculate a predicting score of sustained ROSC. The number was then rounded up or down to the nearest 0.5 integer. The optimal cut-off point to predict the score were calculated from best sensitivity and specificity. The cut-off point value of initial lactate level to predict of sustained ROSC and mortality was calculated using receiver operating characteristic (ROC) curves and area under the ROC (AUROC) curve. Model discrimination was considered to be acceptable discrimination if AUROC =0.7–0.8 and excellent if AUROC =0.8–0.9.19 A P-value <0.05 was considered statistically significant.
Compliance with ethical requirements
The ethics committee of Prince of Songkla University approved this study. The institutional review board of Prince of Songkla University is affiliated with the International Conference on Harmonization in Good Clinical Practice or ICH-GCP protocol. According to our institutional review board protocol for waiver of informed consent, the requirement for consent was waived because the participants had no more than minimal risk and the standard treatment procedure was provided. All research information were kept as confidential data in an encrypted file with password and limited data access by only the researcher and assistant.
Results
Demographic data
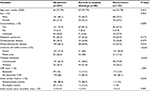
Two hundred and seven nontraumatic OHCA patients were enrolled in this study. The median age was 66 years old. Of the 207 patients, 68.1% were men, 72.9% had comorbidities, 73.4% experienced cardiac arrest at home, 36.7% were witnessed arrest, 14% received CPR by a bystander, and initial shockable rhythms were reported in 11.6%. The mean initial lactate level was 12.4 mmol/L (Table 1). Sustained ROSC following CPR was seen in 41% (Figure 1).
  | Figure 1 The study flow diagram. Note: The result of CPR was sustained ROSC. Abbreviations: CPR, cardiopulmonary resuscitation; ROSC, return of spontaneous circulation. |
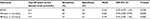
The mean ± SD initial serum lactate level in patients who had sustained ROSC was lower than that of patients who did not sustain ROSC (12.0±4.8 vs 12.6±5, P=0.381). However, the mean ± SD initial serum lactate level had statistical significance to predict 24- and 48-hour mortality (Table 2). The cut-off points of initial serum lactate to predict mortality at 24 and 48 hours after CPR were 9.1 mmol/L (P=0.031) and 9.4 mmol/L (P=0.049), respectively (Table 3).
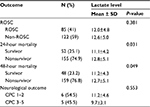  | Table 2 Serum lactate level and outcome Abbreviations: CPC, cerebral performance category; ROSC, return of spontaneous circulation. |
Factors associated with sustained ROSC were no comorbidity (adjusted odds ratio [aOR] 1.71, 95% CI 0.51–5.71, P=0.014), cardiac arrest in a public area (aOR 2.4, 95% CI 1.2–4.79, P=0.013), witness arrest (aOR 2.39, 95% CI 1.26–4.52, P=0.008) (Table 4).
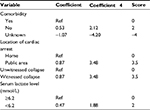
The scoring system to predict sustained ROSC was developed by transforming the coefficients of significant variables and the initial serum lactate level cut-off point of 6.2 mmol/L into the item score (Table 5). The scores range from –4 to 11. The AUROC curve was 0.715, and the best cut-off point score was 3.6. If the score is >3.5, it can predict sustained ROSC (Figure 2).
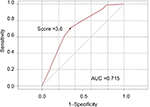  | Figure 2 ROC curve of cut off point score for predicted sustained ROSC. Abbreviations: AUC, area under the curve; ROC, receiver operating characteristic; ROSC, return of spontaneous circulation. |
Discussion
Previous research has shown serum lactate to be an independent prognostic factor of mortality and neurological outcome in severe sepsis.10 However, Shinozaki et al13 found that serum lactate levels combined with ammonia levels were statistically more significant in predicting survival when compared with initial serum lactate alone. Lee et al20 found an association of increased serum lactate clearance with neurological outcomes in OHCA patients after therapeutic hypothermia but did not find an association with the initial serum lactate level. In the present study, the association between sustained ROSC and neurological outcome had no statistical significance, but the serum lactate levels were statistically significant in predicting 24- and 48-hour mortality. The cut-off point for blood lactate levels to predict a poor prognosis in OHCA patients varies from study to study. Wang et al21 reported a lactate level <9 mmol/L was positively associated with a 10-minute ROSC but not significantly associated with the neurological outcome. Shinozaki et al13 also studied lactate levels on admission in 98 OHCA patients, of whom only 10 had a favorable outcome. According to an ROC curve analysis, the optimal cut-off level to predict a favorable outcome (CPC 1, 2) was 12.0 mmol/L. However, it was reported by Grimaldi et al16 that lactate levels <5.1 mmol/L in 225 OHCA patients were associated with favorable outcomes at discharge from the intensive care unit in 225 OHCA patients. Seeger et al14 found that poor neurological outcomes were associated with serum lactate levels >6.94 mmol/L, but serum lactate levels <5 mmol/L correlated with favorable neurological outcomes in a study by Kaji et al.22 In addition, 1 multicenter prospective observational study conducted by Donnino et al23 concluded that lower lactate levels at different measurement times during the first 24 hours as well as a greater percent decrease in lactate over the first 12 hours of post-cardiac arrest were associated with survival and good neurological outcome.
In this current study, the optimal cut-off points, sensitivity, and specificity of the initial lactate level to predict 24- and 48-hour mortality were identified as 9.1 and 9.4 mmol/L, 63% and 57%, and 54% and 61%, respectively. The different time points of serum lactate measurement and outcome selection caused a difference in the threshold values. Serum lactate levels would be higher when measurements are taken during CPR because of blood flow recovery to ameliorate systemic hypoxia and hypoperfusion. An explanation for the cause of elevated serum lactate is its role as a surrogate marker for the status of low-flow or no-flow after cardiac arrest.24,25 However, Müllner et al26 suggested that serum lactate levels may be a weak surrogate marker during cardiac arrest.
Conclusions
The initial serum lactate level was not associated with sustained ROSC and good neurological outcome. However, there was an association with 24- and 48-hour mortality in OHCA and the cut-off points of initial serum lactate levels were 9.1 and 9.4 mmol/L, respectively. The factors related to sustained ROSC in OHCA were comorbidity, witnessed arrest, and location of cardiac arrest. The prediction score of >3.5 indicated sustained ROSC (area under the curve =0.715).
What is already known on this topic
Several studies showed that initial serum lactate predicts sustained ROSC.
What this study adds
The study shows other factors that predict sustained ROSC, good neurological outcome, and mortality.
Acknowledgments
The authors thank Kingkarn Waiyanak for article searches and retrieval, Glenn K Shingledecker for his help in editing the manuscript, and the Epidemiology Unit and the Faculty of Medicine of Prince of Songkla University Hat Yai for funding this research.
Author contributions
Banjaparat Nuanjaroan performed the literature search, study design, data collection, data analysis, data interpretation, and writing. Ar-aishah Dadeh did the study design, critical revision, and manuscript preparation. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Clawson J, Olola C, Scott G, Heward A, Patterson B. Effect of a Medical Priority Dispatch System key question addition in the seizure/convulsion/fitting protocol to improve recognition of ineffective (agonal) breathing. Resuscitation. 2008;79(2):257–264. | ||
Sittichanbuncha Y, Prachanukool T, Sawanyawisuth K. A 6-year experience of CPR outcomes in an emergency department in Thailand. Ther Clin Risk Manag. 2013;9:377–381. | ||
Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics – 2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. | ||
Mizock BA, Falk JL. Lactic acidosis in critical illness. Crit Care Med. 1992;20(1):80–93. | ||
Jeng JC, Jablonski K, Bridgeman A, Jordan MH. Serum lactate, not base deficit, rapidly predicts survival after major burns. Burns. 2002;28(2):161–166. | ||
Kamolz LP, Andel H, Schramm W, Meissl G, Herndon DN, Frey M. Lactate: early predictor of morbidity and mortality in patients with severe burns. Burns. 2005;31(8):986–990. | ||
Callaway DW, Shapiro NI, Donnino MW, Baker C, Rosen CL. Serum lactate and base deficit as predictors of mortality in normotensive elderly blunt trauma patients. J Trauma. 2009;66(4):1040–1044. | ||
Donnino MW, Miller J, Goyal N, et al. Effective lactate clearance is associated with improved outcome in post-cardiac arrest patients. Resuscitation. 2007;75(2):229–234. | ||
Husain FA, Martin MJ, Mullenix PS, Steele SR, Elliott DC. Serum lactate and base deficit as predictors of mortality and morbidity. Am J Surg. 2003;185(5):485–491. | ||
Mikkelsen ME, Miltiades AN, Gaieski DF, et al. Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med. 2009;37(5):1670–1677. | ||
Deakin CD, Morrison LJ, Morley PT, et al. Part 8: advanced life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation. 2010;81(Suppl 1):e93–e174. | ||
Cocchi MN, Miller J, Hunziker S, et al. The association of lactate and vasopressor need for mortality prediction in survivors of cardiac arrest. Minerva Anestesiol. 2011;77(11):1063–1071. | ||
Shinozaki K, Oda S, Sadahiro T, et al. Blood ammonia and lactate levels on hospital arrival as a predictive biomarker in patients with out-of-hospital cardiac arrest. Resuscitation. 2011;82(4):404–409. | ||
Seeger FH, Toenne M, Lehmann R, Ehrlich JR. Simplistic approach to prognosis after cardiopulmonary resuscitation-value of pH and lactate. J Crit Care. 2013;28(3):317.e13–320.e13. | ||
Takaki S, Kamiya Y, Tahara Y, Tou M, Shimoyama A, Iwashita M. Blood pH is a useful indicator for initiation of therapeutic hypothermia in the early phase of resuscitation after comatose cardiac arrest: a retrospective study. J Emerg Med. 2013;45(1):57–64. | ||
Grimaldi D, Dumas F, Perier MC, et al. Short- and long-term outcome in elderly patients after out-of-hospital cardiac arrest: a cohort study. Crit Care Med. 2014;42(11):2350–2357. | ||
Li CJ, Kung CT, Liu BM, et al. Factors associated with sustained return of spontaneous circulation in children after out-of-hospital cardiac arrest of noncardiac origin. Am J Emerg Med. 2010;28(3):310–317. | ||
Cummins RO, Chamberlain DA, Abramson NS, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation. 1991;84(2):960–975. | ||
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29–36. | ||
Lee TR, Kang MJ, Cha WC, et al. Better lactate clearance associated with good neurologic outcome in survivors who treated with therapeutic hypothermia after out-of-hospital cardiac arrest. Crit Care. 2013;17(5):R260. | ||
Wang CH, Huang CH, Chang WT, et al. Monitoring of serum lactate level during cardiopulmonary resuscitation in adult in-hospital cardiac arrest. Crit Care. 2015;19:344. | ||
Kaji AH, Hanif AM, Bosson N, Ostermayer D, Niemann JT. Predictors of neurologic outcome in patients resuscitated from out-of-hospital cardiac arrest using classification and regression tree analysis. Am J Cardiol. 2014;114(7):1024–1028. | ||
Donnino MW, Andersen LW, Giberson T, et al. Initial lactate and lactate change in post-cardiac arrest: a multicenter validation study. Crit Care Med. 2014;42(8):1804–1811. | ||
Ralston SH, Voorhees WD, Showen L, Schmitz P, Kougias C, Tacker WA. Venous and arterial blood gases during and after cardiopulmonary resuscitation in dogs. Am J Emerg Med. 1985;3(2):132–136. | ||
Carden DL, Martin GB, Nowak RM, Foreback CC, Tomlanovich MC. Lactic acidosis during closed-chest CPR in dogs. Ann Emerg Med. 1987;16(12):1317–1320. | ||
Müllner M, Sterz F, Domanovits H, Behringer W, Binder M, Laggner AN. The association between blood lactate concentration on admission, duration of cardiac arrest, and functional neurological recovery in patients resuscitated from ventricular fibrillation. Intensive Care Med. 1997;23(11):1138–1143. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.