Back to Journals » Orthopedic Research and Reviews » Volume 14
Usefulness of Trabecular Metal Cones in Revision Total Knee Arthroplasty in a Korean Population: A Case Series
Authors Baek JH, Lee SC, Ryu S, Ahn HS, Nam CH
Received 7 March 2022
Accepted for publication 31 May 2022
Published 9 June 2022 Volume 2022:14 Pages 199—206
DOI https://doi.org/10.2147/ORR.S365377
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Ji-Hoon Baek,1 Su Chan Lee,1 Suengryol Ryu,2 Hye Sun Ahn,1 Chang Hyun Nam1
1Joint & Arthritis Research, Department of Orthopaedic Surgery, Himchan Hospital, Seoul, Republic of Korea; 2Department of Orthopaedic Surgery, Himnaera Hospital, Busan, Republic of Korea
Correspondence: Chang Hyun Nam, Joint & Arthritis Research, Department of Orthopaedic Surgery, Himchan Hospital, 120, Sinmok-ro, Yangcheon-gu, Seoul, 07999, Republic of Korea, Tel +82-2-3219-9229, Fax +82-2-2061-8605, Email [email protected]
Purpose: The purpose of this study was to assess the medium-term results of trabecular metal cones for the reconstruction of large bone defects in revision TKA.
Methods: Thirteen patients who had undergone revision TKA using trabecular metal cones for femoral and/or tibial large bone defects were identified. We included patients who had a minimum of three years follow-up in the study. We evaluated their functional outcomes, implant survivorship, radiological findings, and complications.
Results: At a mean follow-up of 6.9 years (range of 3.5– 9.4 years), all trabecular metal cones and implants were well fixed and did not exhibit any radiographic evidence of migration or loosening. At the final follow-up, the mean Knee Society knee scores had improved from 37.2 to 78.1 (p < 0.05), and function scores had improved from 35.5 to 77.5 points (p < 0.05). One intraoperative fracture in the distal femur occurred in an 85-year-old woman during impaction of a single trabecular metal cone. The fracture was successfully affixed to the femoral cone and bone three months postoperatively.
Conclusion: The present study of trabecular metal cones demonstrates excellent clinical outcomes and survivorship in revision TKA during medium-term follow-up periods. However, longer-term follow-up studies are needed to further investigate these implants in revision TKA. Additionally, the necessity of metal cones in revision procedures should be carefully considered depending on patient needs and economic capabilities.
Keywords: total knee arthroplasty, trabecular metal cone, outcome, survivorship
Introduction
With the rapid increase in demand for primary total knee arthroplasty (TKA) in Korea, there is also an expected concomitant increase in the burden for revision TKA.1 The management of severe bone loss in revision TKA procedures is an enormous challenge. Based on the Anderson Orthopaedic Research Institute (AORI) classification,2 the largest bone defects (AORI type-2B or 3) can be managed with impaction grafting, structural allografts, porous trabecular metal cones, and tumor prostheses.3–6 The effectiveness of the different options for reconstructing large bone loss has yet to be established.
Trabecular metal cones are a relatively new implant strategy for the reconstruction of large bone defects during revision procedures. They have demonstrated promising short-term results.5,7,8 Trabecular metal cones have the potential advantage of being highly capable of biologic fixation because of their high porosity and low elastic modulus, allowing for immediate weight bearing.9,10 These cones also enable the surgeon to size and position the implant for specific defects.
Several studies in western countries have reported trabecular metal cones in revision TKA performed for severe bone defects. Even though these studies have demonstrated good short- and medium-term results,5,7–9,11 studies on the use of trabecular metal cones are rare in revision TKA, and it is difficult to perform prospective controlled studies due to specific patient criteria in the use of those implants. Especially, since revision TKA procedures using metal cones require a long learning curve, years of experience, advanced surgical techniques, and high cost, it is difficult to gather data on a large number of patients, and corresponding reports are rare in Korea.
Therefore, we designed a retrospective observational study. The purpose of the present study is to assess the medium-term results of trabecular metal cones for revision TKA of large bone defects.
Materials and Methods
The design and protocol of this retrospective study were approved by the Institutional Review Board of Himchan Hospital. The privacy and personal identity information of all participants were protected in accordance with the Declaration of Helsinki. The requirement for informed consent was waived due to its retrospective nature. Fifteen patients (15 knees) underwent revision TKA (Scorpio Total Stabilizer Revision Knee System; Stryker, Mahwah, New Jersey, USA) at a single center using trabecular metal cones (Trabecular Metal; Zimmer, Warsaw, Indiana, USA) for femoral and/or tibial large bone defects between January 2012 and December 2017. The indication for revision TKA using trabecular metal cones in all patients was aseptic loosening after primary TKA. We included patients with a minimum of three years follow-up, and there were no exclusion criteria. Of these 15 patients, one died two years postoperatively from causes unrelated to the in situ revision TKA, and one patient was lost to follow-up. The study group was composed of 1 man and 12 women with an average age of 73.2 years (range, 62 to 85 years) at the time of surgery. Six patients had femoral cone implants, five patients had tibial cones, and two patients had both. The mean clinical follow-up period was 6.9 years (range, 3.5 to 9.4 years). The reason for the revision TKA in our study was aseptic loosening in all 13 cases. There were no cases of septic loosening or fracture as a cause for revision. The intraoperative assessments of femoral and/or tibial bone defects were AORI type IIB in eight patients and type III in five patients.
Demographic data included age, gender, body mass index, AORI type, and pre- and post-operative Knee Society Scores (Table 1). The primary endpoint was trabecular metal cone survivorship. The secondary endpoints were all-cause implant survivorship, patient-reported outcome measurements with KSS scores, and radiographic analyses.
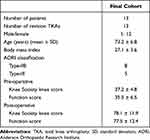 |
Table 1 Demographic Characteristics of the Patients |
Surgical Technique
All the surgical procedures were performed by a senior surgeon using the standard medial parapatellar approach and tourniquet. The surgical procedure of the revision TKA using metal cones was identical with the conventional revision TKA procedure, except for the implantation of the metal cone. Failed prosthetic components were removed, and all osteolytic lesions were carefully debrided. The bone loss of the proximal tibia and distal femur was assessed and classified using the AORI classification system. Femoral and tibial metal cones (Trabecular Metal; Zimmer, Warsaw, Indiana, USA) were only used for management of type-2B or 3 bone loss defects. Tibial and femoral intramedullary guides were then utilized to allow for proper alignment and placement of the cones. Trial sizes for the appropriate metal cones were used to press-fit the cones into their final positions. The cones were matched to the size and shape of the osseous defects. Through press-fit, the metal cones were implanted in the bone defects and rotational stability was manually assessed (Figure 1). Residual voids between the host bone and metal cone were reconstituted with autologous bone from the cuts and allograft or artificial bone. The stemmed tibial and femoral components were cemented in place. Simplex P bone cement (Stryker, Mahwah, New Jersey, USA) was used in all cases.
The patients were immediately mobilized with weight-bearing as tolerated. Active exercises were initiated under the supervision of a physiotherapist. The patients underwent clinical and radiographic follow-ups postoperatively at 2 weeks, 6 weeks, 3, 6, 9, and 12 months, and 1 year thereafter. Clinical evaluations were performed using the Knee Society rating system.12 The results were classified as excellent (80–100), good (70–79), fair (60–69), or poor (<60). Radiographic analysis included long leg standing radiography from the pelvis to the ankle joint for evaluating the axis, a weight-bearing anteroposterior view, a non-weight-bearing anteroposterior view, a lateral view at 30° flexion, and a skyline view of the patella. We considered the 6-week anteroposterior and lateral radiographs as the baseline study for radiographic comparison. Each radiograph was assessed for osseointegration, signs of migration, fracture, and loosening. Each radiograph was objectively examined for radiolucent lines and osteolytic defects using Knee Society Roentgenographic Evaluation and Scoring System (KSRESS).13 Preoperative radiographs and intraoperative assessments identified the type of bone defect according to the AORI classification system.2 Mortality status and implant survival analyses were determined using hospital records and/or interviews with family members. During the follow-up evaluations, we made sure to interview the same caretaker that we had interviewed during the patient’s hospitalization.
The Chi square test was used to analyze Knee Society knee and function scores. The analyses were carried out using SPSS version 18.0 (Chicago, IL, USA). All the reported p-values were two-sided, and a p<0.05 was considered statistically significant.
Results
In radiological assessment using KSRESS of the 13 knees (13 patients) seen at follow-up, a total of 4 (30.8%) knees were noted to have evidence of radiolucent lines. A total of 4 radiolucent lines were detected an average of 1.8 years following surgery (range, 0.6 to 3 years) that were all isolated tibial lucencies without the knee showing femoral lucency. Of these knees, 3 had medial (zone 1 or 2) and 1 had lateral (zone 3 or 4) baseplate radiolucent lines. Radiological assessment did not reveal any evidence of component migration at final follow-up.
At the latest follow-up evaluations, all trabecular metal cones were well fixed with no radiographic evidence of migration or loosening. Serial postoperative imaging showed evidence of osseointegration of the trabecular metal cones, and there was no evidence of implant loosening or progressive radiolucent lines in any of the 13 cases.
The mean Knee Society knee scores improved from 37.2 points preoperatively to 78.1 points at the final follow-up (p<0.05). Clinical outcomes were classified as excellent or good for 10 patients (76.9%), fair for 2 patients (15.4%), and poor for 1 patient (7.7%). Mean preoperative function scores improved from 35.5 points to 77.5 points at the final follow-up (p<0.05). Functional outcomes were classified as excellent or good for 11 patients (84.6%), fair for 1 patient (7.7%), and poor for 1 patient (7.7%).
No significant complications associated with the use of trabecular metal cones were identified in this study. One minor intraoperative fracture in the distal femur occurred in an 85-year-old woman during impaction of one trabecular metal cone. The fracture was affixed successfully to the femoral cone and bone using a suture and bone cement. The patient was allowed to walk a month after the surgery. Radiographic follow-up showed osteointegration and no evidence of migration three months postoperatively (Figure 2).
Discussion
This study demonstrates excellent medium-term outcomes for trabecular metal cones in revision TKAs with large bone defects. All femoral and tibial metal cones were found to be well fixated at a mean follow-up of 6.9 years. There were no mechanical failures associated with using the trabecular metal cones, and all radiographic findings showed signs of osseointegration.
Several studies have reported trabecular metal cones in revision TKA for large bone defects both in the United States and internationally. These studies have demonstrated promising short- and medium-term outcomes (Table 2).5,7,11,14–18 Meneghini et al5 reviewed 15 cones in 15 patients undergoing revision TKA. At a mean follow-up of 2.8 years, none of the implanted cones exhibited evidence of loosening. Long and Scuderi7 reported on a series of 16 revision TKAs with cones. On a mean follow-up of 2.6 years, no loose trabecular metal cones were observed. Howard et al14 reported that on a mean follow-up of 2.8 years, there were no failures in 24 revision TKAs with femoral metal cones. They concluded that femoral metal cones can provide effective structural support for femoral revision implants. Sandiford et al11 reported on the implantation of 14 cones in 14 patients at a mean follow-up of 7.2 years. They observed loosening of the implant in one case, which therefore required a new revision procedure. Our results are consistent with these studies and support previous findings in western countries. One patient with poor Knee Society knee score was associated with progression of Parkinson’s disease rather than revision surgery. We did not find any evidence of loosening or migration of the cones and implants in any cases (Figure 3).
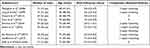 |
Table 2 Previous Literature of Trabecular Metal Cones in Western Countries |
With respect to radiolucent lines, we were able to identify prostheses using the Knee Society Roentgenographic Evaluation and Scoring System (KSRESS). Areas of lucency were confined to medial and lateral aspects of the tibial base plate (zones 1–4), with no femoral lucency. None of these radiolucent lines had progressed at a mean follow-up of 6.9 years. It was not clear why radiolucent lines were present only in the tibial component, but it might be due to the small cohort.
Revision TKAs have shown a rapid increase between 2001 and 2010 by 267% in Korea.19 The gradual increase in revision TKA can be explained by the increase in the aging population and improved accessibility to the healthcare system.20 It is reasonable to expect that many surgeons will encounter severe bone defects presenting as one of the major challenging issues in revision surgery. Our study shows evidence that trabecular metal cones are an effective option for obtaining stable implants of large bone defects in revision TKAs. Additionally, surgery costs using trabecular metal cones in revision arthroplasties are expensive and therefore cannot be recommended to all patients. The necessity of metal cones in revision procedures should be considered carefully depending on patient needs and economic capabilities.
Trabecular metal cones have several distinct advantages. First and foremost, because several sizes and shapes of cones are available, the surgical technique required for implants is relatively simple. Therefore, cones may reduce the operative time and infection risk. Second, the cones allow for adequate structural support to the implants and offer the opportunity for early weight bearing.21 The third advantage is the low potential risk of disease transmission that is associated with structural allografts.21 Last, trabecular metal cones are suitable for a larger number of indications, such as augmentations in tumor prostheses or after periprosthetic fractures.
Complications in the present study include a case of an intraoperative distal femoral fracture that occurred in an 85-year-old woman during impaction of one trabecular metal cone. At the time of the revision procedure, the distal medial condyle fragment was not unstable and was limited in fixation with a plate and screws. It was affixed to the femoral cone and bone using a suture and bone cement. Complications with metal cones are rare but do include the risk of intraoperative fracture during revision surgery.22,23 This case emphasizes the importance of adequate impaction power and the appropriate size of the metal cone.
There are inevitable limitations to this study. First, this study is retrospectively designed and is performed on a small number of patients. Surgery using trabecular metal cones is expensive and cannot be recommended to all patients. Second, because this study has no comparative group and a small sample size, it has no external validity. Third, because there were only few patient cases with trabecular metal cones at a single center, generalization about these outcomes may be limited. Fourth, although the follow-up period had a mean of 6.9 years, a medium-term follow-up period may not be enough to confirm the long-term effects and may not be a guarantee of good outcomes on long-term follow-ups. Last, this study only included a trabecular metal cone group, lacking the usefulness of a comparison with other treatment options such as impaction grafting, structural allografts, and nontrabecular implants. However, this study could not be prospectively randomized because the outcomes associated with impaction grafting and structural allografts were not promising.24,25
The present study of trabecular metal cones exhibits excellent clinical outcomes and survivorship in revision TKA during medium-term follow-up. Trabecular metal cones have been increasingly used for large bone defects in revision TKA. The necessity of metal cones in revision procedures should be carefully considered depending on patient needs and economic capabilities. In addition, longer-term follow-up studies are needed to further investigate these implants in revision TKA.
Ethics Statement
This study was approved by the Institutional Review Board of Himchan Hospital.
Funding
There is no funding to report.
Disclosure
Each author certifies that he or she has no commercial association (eg consultancies, stock ownership, equity interest, patent, licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
References
1. Kim TW, Kang SB, Chang CB, Moon SY, Lee YK, Koo KH. Current trends and projected burden of primary and revision total knee arthroplasty in Korea between 2010 and 2030. J Arthroplasty. 2021;36(1):93–101. doi:10.1016/j.arth.2020.06.064
2. Engh GA, Ammeen DJ. Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect. 1999;48:167–175.
3. Lotke PA, Carolan GF, Puri N. Impaction grafting for bone defects in revision total knee arthroplasty. Clin Orthop Relat Res. 2006;446:99–103. doi:10.1097/01.blo.0000214414.06464.00
4. Engh GA, Ammeen DJ. Use of structural allograft in revision total knee arthroplasty in knees with severe tibial bone loss. J Bone Joint Surg Am. 2007;89(12):2640–2647. doi:10.2106/JBJS.F.00865
5. Meneghini RM, Lewallen DG, Hanssen AD. Use of porous tantalum metaphyseal cones for severe tibial bone loss during revision total knee replacement. J Bone Joint Surg Am. 2008;90(1):78–84. doi:10.2106/JBJS.F.01495
6. Springer BD, Hanssen AD, Sim FH, Lewallen DG. The kinematic rotating hinge prosthesis for complex knee arthroplasty. Clin Orthop Relat Res. 2001;392:283–291. doi:10.1097/00003086-200111000-00037
7. Long WJ, Scuderi GR. Porous tantalum cones for large metaphyseal tibial defects in revision total knee arthroplasty: a minimum 2-year follow-up. J Arthroplasty. 2009;24(7):1086–1092. doi:10.1016/j.arth.2008.08.011
8. Rao BM, Kamal TT, Vafaye J, Moss M. Tantalum cones for major osteolysis in revision knee replacement. Bone Joint J. 2013;95-B(8):1069–1074. doi:10.1302/0301-620X.95B8.29194
9. Potter GD, Abdel MP, Lewallen DG, Hanssen AD. Midterm results of porous tantalum femoral cones in revision total knee arthroplasty. J Bone Joint Surg Am. 2016;98(15):1286–1291. doi:10.2106/JBJS.15.00874
10. Maslaris A, Layher F, Bungartz M, et al. Sagittal profile has a significant impact on the explantability of well-fixed cemented stems in revision knee arthroplasty: a biomechanical comparison study of five established knee implant models. Arch Orthop Trauma Surg. 2019;139(7):991–998. doi:10.1007/s00402-019-03160-4
11. Sandiford NA, Misur P, Garbuz DS, Greidanus NV, Masri BA. Difference between trabecular metal cones and femoral head allografts in revision TKA: minimum 5-year followup. Clin Orthop Relat Res. 2017;475(1):118–124. doi:10.1007/s11999-016-4898-9
12. Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the knee society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. doi:10.1097/00003086-198911000-00004
13. Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. doi:10.1097/00003086-198911000-00003
14. Howard JL, Kudera J, Lewallen DG, Hanssen AD. Early results of the use of tantalum femoral cones for revision total knee arthroplasty. J Bone Joint Surg Am. 2011;93(5):478–484. doi:10.2106/JBJS.I.01322
15. Panni AS, Vasso M, Cerciello S. Modular augmentation in revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2013;21(12):2837–2843. doi:10.1007/s00167-012-2258-1
16. Derome P, Sternheim A, Backstein D, Malo M. Treatment of large bone defects with trabecular metal cones in revision total knee arthroplasty: short term clinical and radiographic outcomes. J Arthroplasty. 2014;29(1):122–126. doi:10.1016/j.arth.2013.04.033
17. Jensen CL, Winther N, Schroder HM, Petersen MM. Outcome of revision total knee arthroplasty with the use of trabecular metal cone for reconstruction of severe bone loss at the proximal tibia. Knee. 2014;21(6):1233–1237. doi:10.1016/j.knee.2014.08.017
18. De Martino I, De Santis V, Sculco PK, D’Apolito R, Assini JB, Gasparini G. Tantalum cones provide durable midterm fixation in revision TKA. Clin Orthop Relat Res. 2015;473(10):3176–3182. doi:10.1007/s11999-015-4338-2
19. Koh IJ, Kim TK, Chang CB, Cho HJ, In Y. Trends in use of total knee arthroplasty in Korea from 2001 to 2010. Clin Orthop Relat Res. 2013;471(5):1441–1450. doi:10.1007/s11999-012-2622-y
20. Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94(3):201–207. doi:10.2106/JBJS.J.01958
21. Mancuso F, Beltrame A, Colombo E, Miani E, Bassini F. Management of metaphyseal bone loss in revision knee arthroplasty. Acta Biomed. 2017;88(2S):98–111. doi:10.23750/abm.v88i2-S.6520
22. Zanirato A, Cavagnaro L, Basso M, Divano S, Felli L, Formica M. Metaphyseal sleeves in total knee arthroplasty revision: complications, clinical and radiological results. A systematic review of the literature. Arch Orthop Trauma Surg. 2018;138:993–1001. doi:10.1007/s00402-018-2967-0
23. Barnett SL, Mayer RR, Gondusky JS, Choi L, Patel JJ, Gorab RS. Use of stepped porous titanium metaphyseal sleeves for tibial defects in revision total knee arthroplasty: short term results. J Arthroplasty. 2014;29(6):1219–1224. doi:10.1016/j.arth.2013.12.026
24. Backstein D, Safir O, Gross A. Management of bone loss: structural grafts in revision total knee arthroplasty. Clin Orthop Relat Res. 2006;446:104–112. doi:10.1097/01.blo.0000214426.52206.2c
25. Hilgen V, Citak M, Vettorazzi E, et al. 10-year results following impaction bone grafting of major bone defects in 29 rotational and hinged knee revision arthroplasties: a follow-up of a previous report. Acta Orthop. 2013;84(4):387–391. doi:10.3109/17453674.2013.814012
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



