Back to Journals » Research and Reports in Urology » Volume 10
Use of venous-thrombotic-embolic prophylaxis in patients undergoing surgery for renal tumors: a questionnaire survey in the Nordic countries (The NORENCA -2 study)
Authors Lund L , Nisen H, Järvinen P , Fovaeus M , Gudmundsson E, Kromann-Andersen B, Ljungberg B, Nilsen F, Sundqvist P , Clark PE, Beisland C
Received 21 June 2018
Accepted for publication 17 September 2018
Published 25 October 2018 Volume 2018:10 Pages 181—187
DOI https://doi.org/10.2147/RRU.S177774
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jan Colli
Lars Lund,1,2 Harry Nisen,3 Petrus Järvinen,3 Magnus Fovaeus,4 Eirikur Gudmundsson,5 Bjarne Kromann-Andersen,6 Börje Ljungberg,7 Frode Nilsen,8 Pernilla Sundqvist,9 Peter E Clark,10 Christian Beisland11,12
1Department of Urology, Odense University Hospital, 2Clinical Institute, Southern University of Denmark, Odense, Denmark; 3Department of Urology, Helsinki University Hospital, Helsinki, Finland; 4Department of Urology, Sahlgrenska University Hospital, Gothenburg, Sweden; 5Department of Urology, Landspitali University Hospital, Reykjavik, Iceland; 6Department of Urology, Herlev University Hospital, Copenhagen, Denmark; 7Department of Surgical and Perioperative Sciences, Urology and Andrology, Umeå University, Umeå, Sweden; 8Department of Urology, Akershus University Hospital, Lörenskog, Norway; 9Department of Urology, Faculty of Medicine and Health, Örebro University, Örebro, Sweden; 10Department of Urology, Atrium Health, Charlotte, NC, USA; 11Department of Urology, Haukeland University Hospital, 12Department of Clinical Medicine, University of Bergen, Bergen, Norway
Purpose: To examine the variation in venous thromboembolism prophylactic treatment (VTEP) among renal cancer patients undergoing surgery.
Materials and methods: An Internet-based questionnaire on renal tumor management before and after surgery was mailed to all Nordic departments of urology. The questions focused on the use of VTEP and were subdivided into different surgical modalities.
Results: Questionnaires were mailed to 91 institutions (response rate 53%). None of the centers used VTEP before surgery, unless the patient had a vena caval tumor thrombus. Overall, the VTEP utilized during hospitalization for patients undergoing renal surgery included early mobilization (45%), compression stockings (52%) and low-molecular-weight heparin (89%). In patients undergoing open radical Nx, 80% of institutions used VTEP during their hospitalization (23% compression stockings and 94% low-molecular-weight heparin). After leaving the hospital, the proportion and type of VTEP received varied considerably across institutions. The most common interval, used in 60% of the institutions, was for a period of 4 weeks. The restriction to the Nordic countries was a limitation and, therefore, may not reflect the practice patterns elsewhere. It is a survey study and, therefore, cannot measure the behaviors of those institutions that did not participate.
Conclusion: We found variation in the type and duration of VTEP use for each type of local intervention for renal cancer. These widely disparate variations in care strongly argue for the establishment of national and international guidelines regarding VTEP in renal surgery.
Keywords: venous-thrombotic-embolic prophylaxis kidney cancer, surgery, nephrectomy, mortality, complication, minimally invasive methods, thrombosis prophylaxis
Introduction
The development of venous thromboembolism (VTE) is due to an imbalance in hematostasis, which in Virchow’s triad is described as an interaction between the vessel wall, blood flow and blood composition.1 Prolonged immobilization or direct compression of the veins from a growing kidney tumor can give reduced flow in cancer patients and are well-known risk factors for VTE. Cancerous diseases can result in both direct and indirect effects on the vessel wall due to tumor invasion or increased inflammatory influence affecting both the vessel walls and the components of the coagulation cascade.
Cancer surgery is associated with a doubling of the risk of postoperative VTE compared with similar surgery for benign diseases.2 Patients with pancreatic or gastric cancer have the greatest risk, while pulmonary, bladder and gynecological cancers also have an increased risk.3 In a prospective cohort study, VTE was the most frequent cause of death within the first 30 days after cancer surgery for a variety of different malignancies and 40% of postoperative VTE occurred at least 21 days after surgical intervention.4 A high dose of low-molecular-weight heparin (LMWH; 5,000 vs 2,500 IU) results in significantly lower incidence of VTE in cancer surgery without an increased bleeding risk.5 A Cochrane review concluded that 4 weeks of thrombosis prophylaxis after major abdominal and pelvic surgery reduces the risk of postoperative VTE.6
The five Nordic countries (Denmark, Finland, Iceland, Norway and Sweden) comprise 25 million people, and have quite similar treatment traditions and state-funded high-quality health care systems.
The Nordic Renal Cancer group is a newly formed working group with representatives from all the Nordic countries, with the aim of performing high-quality research on kidney cancer in the Nordic countries.7 The purpose of this study is to examine the use of VT prophylactic treatment (VTEP) among renal cancer patients undergoing curative therapy in the five Nordic countries prior to the publishing of the first European Association of Urology (EAU) Guidelines on thromboprophylaxis in urological surgery.8
Materials and methods
The study group
The study was carried out by a collaborative group originating from the Scandinavian Association of Urology and is presented at the homepage of the Scandinavian Association of Urology (www.NUF.nu).
The questionnaire
A 21-question Internet-based questionnaire on renal tumor management before and after surgery was mailed to all Nordic departments of urology performing renal cancer surgery (Supplementary material). The questions addressed the use of VTEP and were subdivided into different surgical modalities: open radical and partial nephrectomy (Nx), laparoscopic/robotic Nx and laparoscopic and percutaneous thermal ablation of tumors.
In total, 91 institutions from all five countries were invited to participate. The questionnaires were mailed to the departments during late fall of 2016, and after two rounds of invitations, the database was closed on February 1, 2017. Six institutions did not perform renal surgery in 2016. We received responses from 45 of 85 hospitals performing any form of renal surgery (response rate 53%), as shown in Table 1. There were responses from 6 institutions from Denmark (75%), 12 from Finland (48%), 1 from Iceland (100%), 11 from Norway (73%) and 15 from Sweden (48%), as shown in Table 1.
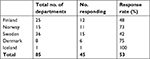  | Table 1 The response rate from the different Nordic countries among the institutions which perform therapeutic procedures for renal cancer |
The survey did not include patient-related data or affected patient treatment or care. Therefore, it did not require approval from the ethical committee. Completion of the survey was considered as informed consent from the participating departments.
Results
None of the 45 institutions used VTEP before surgery unless the patient had a vena caval tumor thrombus. Overall, the proportion of institutions that used VTEP during hospitalization for patients undergoing renal surgery included 45% using early mobilization, 52% using compression stockings and 89% using LMWH (Table 2). In patients undergoing open radical Nx, 80% of the institutions used VTEP during their hospitalization (23% compression stockings and 94% LMWH; Table 3). After leaving the hospital, the proportion and type of VTEP received varied considerably across institutions (5% for 1 week, 35% for 2 weeks and 60% for 4 weeks). For patients undergoing open partial Nx, 75% of institutions utilized VTEP (27% compression stockings and 91% LMWH; Table 3). After discharge, the VTEP regimen offered to patients was for 1 week in 12%, 2 weeks in 48% and 4 weeks in 40% of the institutions. For patients undergoing robotic radical Nx, 73% of the institutions utilized VTEP (27% compression stockings and 85% LMWH; Table 3). After hospital discharge, VTEP duration across institutions was 15% for 1 week, 39% for 2 weeks, 36% for 4 weeks and 10% for other. For those who underwent laparoscopic/robotic partial Nx, 70% of the institutions utilized VTEP (29% compression stockings and 85% LMWH; Table 3). VTEP was continued after discharge from the hospital for 1 week, 2 weeks and 4 weeks in 20%, 48% and 32% of the institutions, respectively. Five centers performed laparoscopic/robotic thermal ablation of tumors, and overall, 60% used compression stockings and 80% used LMWH. Two centers continued VTEP for 1 week (40%) and three centers continued it for 2 weeks (60%). Three centers performed percutaneous ablation and used VTEP using compression stockings (67%) and 33% used LMWM. After discharge, one facility continued VTEP for 1 week, while the others continued it for 2 weeks. The responses for individual questions among institutions from the different Nordic countries are shown in Table 2.
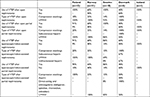  | Table 3 What kind of VTEP is utilized in patients’ undergoing different modalities of surgery? Abbreviations: VTEP, venous thromboembolism prophylaxis; LMWH, Low-molecular-weight heparin. |
Discussion
Our survey results demonstrate wide variability in the type, duration and setting for VTEP among institutions performing therapeutic surgery/procedures for renal cancer in the Nordic countries. As just one example, the use of any VTEP after minimally invasive radical Nx ranged from 0% to 91% by the institutions within a given country (60%–91%, if the one institution that responded from Iceland was excluded). For minimally invasive partial Nx, the range was 40%–90%. Similar wide variability is seen in the type of VTEP utilized and in the duration of VTEP use after discharge from the hospital. This is despite the fact that both the EAU and Danish Society for Hematostasis and Thrombosis recommend that all patients undergoing surgery for malignant solid tumors should have thrombosis prophylaxis, and that it ought to be given for up to 4 weeks after a major surgery.6,8
The variability in practice may reflect critical gaps in our knowledge on the use of VTEP in kidney cancer. Perhaps the most immediate and glaring gap is the prospective clinical trials on VTEP among patients undergoing surgery for renal cancer. Several studies have used the American College of Surgeons National Surgical Quality Improvement Program to estimate the rate of VTE within 30 days after renal cancer surgery and found rates between 0.7% and 1.7% (open radical Nx 1.7%, laparoscopic radical or partial Nx 0.7%).9–13 While several publications have explored the risk factors for the development of VTE,9,11,13–15 there are no prospective, randomized trials comparing different types, duration and therapeutic settings for VTEP among renal cancer surgery patients. A single-center, retrospective experience suggested that perioperative use of pharmacologic VTEP limited to postoperative hospitalization was not associated with lower VTE rates after robotic partial nephrectomy.15 However, in this study no investigations were done to find out whether the patients received any VTEP profylaxsis after discharge from the hospital. Further, the study is based on a survey and has the potential to suffer from bias.
Another significant gap is the lack of specific guidelines for VTEP in urologic surgery. The American Urologic Association and the International Consultation on Urological Disease produced a collaborative review, Anticoagulation and Antiplatelet Therapy in Urologic Practice, which predominantly focused on the management of patients on chronic anticoagulation or antiplatelet therapy for differing medical comorbidities who required a urologic intervention. While there have been several review papers on the subject of VTEP in urology,16,17 urologic surgery-specific guidelines are largely lacking and where guidance exists, it is generally predicated on indirect evidence from other surgical procedures rather than procedure-specific studies within the urologic literature. For example, the EAU has created a guideline on VTEP (http://uroweb.org/guideline/thromboprophylaxis/#3) in which the quality and indirect nature of the evidence available to the panel meant that the overwhelming majority of recommendations were with low or very low quality of evidence and most of the recommendations had to be “weak”. This is not a reflection on the quality of the guideline per se, but on the quality of the evidence available in the literature that underlies the guideline process itself.
It is not surprising that given the gaps in evidence and specific guidance surrounding VTEP for urologic surgery, there have been large variations in the use of VTEP reported both for radical cystectomy16,18,19 and radical prostatectomy.16,18–20 Our study is the first report to survey the use of VTEP across institutions focused on surgery for renal tumors. As is the case with pelvic malignancies, there is widespread variation in the use of VTEP in terms of the type used, the surgical indications, whether it was used after hospital discharge and the total duration after surgery. The significant variability of VTEP across most urologic cancer surgery clearly highlights the need for urologic-specific VTEP guidelines such as the most recent one published by the EAU. Dissemination of these guidelines and more widespread adoption should help to reduce these variations in care and align practice patterns with the evidence available. There are several limitations of this study that should be acknowledged. This is a survey study and, therefore, cannot measure the behaviors of those institutions that did not fill out the instrument. However, the overall return rate, 53%, among those institutions performing kidney tumor surgery, was moderate for a survey-based study, which mitigates this to some degree. Additionally, the study was completed before the EAU guidelines on VTEP were published. However, the results of our study may still be used as baseline evaluation to which future practice patterns can be compared in Scandinavia. It would be useful to repeat this study at defined intervals to test the incorporation of the EAU guidelines into clinical practice. Finally, this survey was intentionally restricted to the Nordic countries and, therefore, may not reflect the practice patterns elsewhere.
Conclusion
The study shows large differences in peri- and postoperative prophylactic treatment for VTE after renal surgery. This variation in care often does not match current guidelines from either the EAU or the Danish Society for Hematostasis and Thrombosis and should be reevaluated as these guidelines become more widely disseminated. Further studies are needed to be able to give evidence-based recommendations.
Acknowledgment
The Nordic Renal Cancer collaboration group is funded by the Scandinavian Association of Urology. The abstract is available online here: http://www.diva-portal.org/smash/record.jsf?pid=diva2%3A1135113&dswid=-5326.
Disclosure
The authors report no conflicts of interest in this work.
References
Brotman DJ, Deitcher SR, Lip GY, Matzdorff AC. Virchow’s triad revisited. South Med J. 2004;97(2):213–214. | ||
White RH, Zhou H, Romano PS. Incidence of symptomatic venous thromboembolism after different elective or urgent surgical procedures. Thromb Haemost. 2003;90(3):446–455. | ||
Khorana AA, McCrae KR. Risk stratification strategies for cancer-associated thrombosis: an update. Thromb Res. 2014;133(Suppl 2):S35–S38. | ||
Agnelli G, Bolis G, Capussotti L, et al. A clinical outcome-based prospective study on venous thromboembolism after cancer surgery: the @RISTOS project. Ann Surg. 2006;243(1):89–95. | ||
Bergqvist D, Burmark US, Flordal PA, et al. Low molecular weight heparin started before surgery as prophylaxis against deep vein thrombosis: 2500 versus 5000 XaI units in 2070 patients. Br J Surg. 1995;82(4):496–501. | ||
Rasmussen MS, Jørgensen LN, Wille-Jørgensen P. Prolonged thromboprophylaxis with low molecular weight heparin for abdominal or pelvic surgery. Cochrane Database Syst Rev. 2009;21(1):CD004318. | ||
Nisen H, Järvinen P, Fovaeus M, et al. Contemporary treatment of renal tumors: a questionnaire survey in the Nordic countries (the NORENCA-I study). Scand J Urol. 2017;51(5):360–366. | ||
Ljungberg B, Bensalah K, Canfield S, et al. EAU guidelines on renal cell carcinoma: 2014 update. Eur Urol. 2015;67(5):913–924. | ||
McAlpine K, Breau RH, Mallick R, et al. Current guidelines do not sufficiently discriminate venous thromboembolism risk in urology. Urol Oncol. 2017;35(7):457.e1–457.e8. | ||
Jordan BJ, Matulewicz RS, Trihn B, Kundu S. Venous thromboembolism after nephrectomy: incidence, timing and associated risk factors from a national multi-institutional database. World J Urol. 2017;35(11):1713–1719. | ||
De Martino RR, Goodney PP, Spangler EL, et al. Variation in thromboembolic complications among patients undergoing commonly performed cancer operations. J Vasc Surg. 2012;55(4):1035.e4–1040.e4. | ||
Alberts BD, Woldu SL, Weinberg AC, Danzig MR, Korets R, Badani KK. Venous thromboembolism after major urologic oncology surgery: a focus on the incidence and timing of thromboembolic events after 27,455 operations. Urology. 2014;84(4):799–806. | ||
Tyson MD, Castle EP, Humphreys MR, Andrews PE. Venous thromboembolism after urological surgery. J Urol. 2014;192(3):793–797. | ||
Clément C, Rossi P, Aissi K, et al. Incidence, risk profile and morphological pattern of lower extremity venous thromboembolism after urological cancer surgery. J Urol. 2011;186(6):2293–2297. | ||
Kara O, Zargar H, Akca O, et al. Risks and benefits of pharmacological prophylaxis for venous thromboembolism prevention in patients undergoing robotic partial nephrectomy. J Urol. 2016;195(5):1348–1353. | ||
Violette PD, Cartwright R, Briel M, Tikkinen KA, Guyatt GH. Guideline of guidelines: thromboprophylaxis for urological surgery. BJU Int. 2016;118(3):351–358. | ||
Saluja M, Gilling P. Venous thromboembolism prophylaxis in urology: a review. Int J Urol. 2017;24(8):589–593. | ||
Pridgeon S, Allchorne P, Turner B, Peters J, Green J. Venous thromboembolism (VTE) prophylaxis and urological pelvic cancer surgery: a UK national audit. BJU Int. 2015;115(2):223–229. | ||
Sterious S, Simhan J, Uzzo RG, et al. Familiarity and self-reported compliance with American Urological Association best practice recommendations for use of thromboembolic prophylaxis among American Urological Association members. J Urol. 2013;190(3):992–998. | ||
Weinberg A, Wright J, Deibert C, et al. Nationwide practice patterns for the use of venous thromboembolism prophylaxis among men undergoing radical prostatectomy. World J Urol. 2014;32(5):1313–1321. |
Supplementary material
Venous-thrombotic-embolic (VTE) prophylaxis survey for renal surgery
- Country in which you practice
- What form(s) of VTE prophylaxis do you use in patients with renal tumors before surgery (check all that apply)?
- None
- Aspirin
- Direct-acting oral anticoagulants (dabigatran, apixaban, rivaroxaban, edoxaban)
- Subcutaneous heparin
- Low molecular weight heparin
- Unfractionated heparin
- Other
- What form(s) of VTE prophylaxis do you use in patients undergoing renal surgery while they are in the hospital (check all that apply)?
- None
- Early ambulation
- Sequential compression device
- Compression stockings
- Aspirin
- Direct-acting oral anticoagulants (dabigatran, apixaban, rivaroxaban, edoxaban)
- Subcutaneous heparin
- Low molecular weight heparin
- Unfractionated heparin
- Other
- Do you use VTE prophylaxis in patients undergoing open nephrectomy after they leave the hospital?
- Yes
- No – if no go to question 7
- If yes, what prophylaxis do you use (check all that apply)?
- Compression stockings
- Aspirin
- Direct-acting oral anticoagulants (dabigatran, apixaban, rivaroxaban, edoxaban)
- Subcutaneous heparin
- Low molecular weight heparin
- Unfractionated heparin
- Other
- How long do you use VTE prophylaxis after patients leave the hospital for nephrectomy?
- One week
- Two weeks
- Four weeks
- Six weeks
- Other
- Do you use VTE prophylaxis in patients undergoing open partial nephrectomy after they leave the hospital?
- Yes
- No – if no go to question 10
- If yes, what prophylaxis do you use (check all that apply)?
- Compression stockings
- Aspirin
- Direct-acting oral anticoagulants (dabigatran, apixaban, rivaroxaban, edoxaban)
- Subcutaneous heparin
- Low molecular weight heparin
- Unfractionated heparin
- Other
- How long do you use VTE prophylaxis after patients leave the hospital for open partial nephrectomy?
- One week
- Two weeks
- Four weeks
- Six weeks
- Other
- Do you use VTE prophylaxis in patients undergoing laparoscopic/ robot ass. nephrectomy after they leave the hospital?
- Yes
- No – if no go to question 13
- If yes, what prophylaxis do you use (check all that apply)?
- Compression stockings
- Aspirin
- Direct-acting oral anticoagulants (dabigatran, apixaban, rivaroxaban, edoxaban)
- Subcutaneous heparin
- Low molecular weight heparin
- Unfractionated heparin
- Other
- How long do you use VTE prophylaxis after patients leave the hospital for laparoscopic/ robot ass. Nephrectomy?
- One week
- Two weeks
- Four weeks
- Six weeks
- Other
- Do you use VTE prophylaxis in patients undergoing laparoscopic/ robot ass. partial nephrectomy after they leave the hospital?
- Yes
- No – if no go to question 16
- If yes, what prophylaxis do you use (check all that apply)?
- Compression stockings
- Aspirin
- Direct-acting oral anticoagulants (dabigatran, apixaban, rivaroxaban, edoxaban)
- Subcutaneous heparin
- Low molecular weight heparin
- Unfractionated heparin
- Other
- How long do you use VTE prophylaxis after patients leave the hospital for laparoscopic/ robot ass. partial nephrectomy?
- One week
- Two weeks
- Four weeks
- Six weeks
- Other
- Do you use VTE prophylaxis in patients undergoing laparoscopic/robotic thermal ablation of kidney tumors after they leave the hospital?
- Yes
- No – if no go to question 19
- If yes, what prophylaxis do you use (check all that apply)?
- Compression stockings
- Aspirin
- Direct-acting oral anticoagulants (dabigatran, apixaban, rivaroxaban, edoxaban)
- Subcutaneous heparin
- Low molecular weight heparin
- Unfractionated heparin
- Other
- How long do you use VTE prophylaxis after patients leave the hospital for laparoscopic/robotic thermal ablation of kidney tumors?
- One week
- Two weeks
- Four weeks
- Six weeks
- Other
- Do you use VTE prophylaxis in patients undergoing percutaneous thermal ablation of kidney tumors after they leave the hospital?
- Yes
- No – if no finished
- If yes, what prophylaxis do you use (check all that apply)?
- Compression stockings
- Aspirin
- Direct-acting oral anticoagulants (dabigatran, apixaban, rivaroxaban, edoxaban)
- Subcutaneous heparin
- Low molecular weight heparin
- Unfractionated heparin
- Other
- How long do you use VTE prophylaxis after patients leave the hospital for percutaneous thermal ablation of kidney tumors?
- One week
- Two weeks
- Four weeks
- Six weeks
- Other
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

