Back to Journals » International Medical Case Reports Journal » Volume 14
Use of the Human Broncho® Double-Lumen Tube in a Tracheal Bronchus Patient After Failed Lung Isolation with a Broncho-Cath™: A Case Report
Received 9 June 2021
Accepted for publication 29 July 2021
Published 12 August 2021 Volume 2021:14 Pages 539—543
DOI https://doi.org/10.2147/IMCRJ.S323263
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ronald Prineas
Sung-Hye Byun, Kyungmin Kim
Department of Anesthesiology and Pain Medicine, Kyungpook National University Chilgok Hospital, School of Medicine, Kyungpook National University, Daegu, Republic of Korea
Correspondence: Sung-Hye Byun
Department of Anesthesiology and Pain Medicine, Kyungpook National University Chilgok Hospital, School of Medicine, Kyungpook National University, 807, Hoguk-ro, Buk-gu, Daegu, 41404, Republic of Korea
Tel + 82-53-200-5863
Email [email protected]
Abstract: Airway management for one-lung ventilation may be challenging for anesthesiologists depending on the location of the tracheal bronchus orifice and possible anatomical distortions. Polyvinyl chloride double-lumen tube Broncho-Cath™ has been successfully used for one-lung ventilation in most cases of tracheal bronchus arising within 2 cm above the carina. However, there have been reports of occasional failure. A 78-year-old male patient diagnosed with secondary pneumothorax was scheduled for video-assisted thoracic surgery, and the tracheal bronchus originating 1.9 cm above the carina was shown in the preoperative chest computed tomography. Although a left-sided Broncho-Cath was initially placed, one-lung ventilation could not be achieved. Under bronchoscopy view through the tracheal lumen, the tracheal bronchus orifice was found to be partially obstructed. Furthermore, the bronchial cuff was herniated from the left main bronchus, leading to a failure of one-lung ventilation. The Broncho-Cath was replaced with a silicone double-lumen tube Human Broncho®, which has more flexible bronchial segment and an increased marginal gap between the bronchial cuff and the tracheal lumen opening. The Human Broncho was successfully placed in an optimal position within the left main bronchus without blocking the tracheal bronchus orifice, thereby achieving the successful one-lung ventilation. The structurally unique Human Broncho may be considered as an alternative option in thoracic surgery of tracheal bronchus patients if lung isolation cannot be achieved with the Broncho-Cath.
Keywords: tracheal bronchus, double-lumen tube, one-lung ventilation, thoracic surgery, case report
Introduction
A tracheal bronchus (TrB) is one of the most common congenital anomalies of the central airway.1 Most cases are asymptomatic and of little clinical significance in non-thoracic surgery. However, a TrB can make airway management challenging in cases requiring one-lung ventilation (OLV) and thus require extra care.2,3 Fortunately, successful OLV with the use of a double-lumen tube (DLT) has been reported in most cases of thoracic surgery complicated by a TrB,3–5 particularly when the TrB and carina are close enough that the orifice of the TrB is not blocked by the tracheal lumen of the DLT and the main bronchi do not show excessive anatomical distortion.2
Here, we report a TrB patient who was initially intubated with a left-sided polyvinyl chloride (PVC) DLT Broncho-Cath™, but failed lung isolation, and so the problem was resolved by replacing the tube with a silicone DLT Human Broncho® with different structural characteristics.
Case Presentation
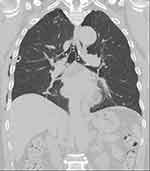
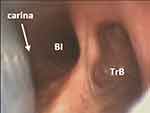
A 78-year-old male patient (168 cm, 70 kg) was scheduled for video-assisted thoracoscopic wedge resection due to recurrent secondary right-sided pneumothorax despite the insertion of a chest tube. In the preoperative chest computed tomography (CT) scan, the take-off of a TrB could be identified in the tracheal wall on the right side, approximately 1.9 cm above the carina (Figure 1). This originating level was based on the lower margin used in previous reports,2,4 and it has been reported that OLV could be successfully performed with a DLT in most cases of the TrB originating within 2 cm from the carina.4 Therefore, the left-sided Broncho-Cath (Covidien, Mansfield, MA, USA), and a 37-Fr tube was chosen based on the left main bronchus (LMB) diameter on chest CT. Standard monitoring (including electrocardiography, pulse oximetry, and non-invasive blood pressure) was performed. Total intravenous anesthesia was performed using propofol and remifentanil, and 70 mg of rocuronium was administered intravenously for muscle relaxation. Tracheal intubation was performed using a video-laryngoscope (UEscope®, Zhejiang UE Medical Co., Zhejiang, China), and then a flexible bronchoscope (aScope™ 4 Broncho Large 5.8/2.8, Ambu® A/S, Ballerup, Denmark) was used to confirm the DLT position. When the bronchoscope was inserted into the tracheal lumen of the DLT, to the right of the tracheal carina a ridge and a partially obstructed orifice could be seen in the bottom right of the monitor of the bronchoscopy system (Figure 2). The DLT was located to the left of tracheal carina; however, there was a slight herniation of the bronchial cuff of the DLT out of the LMB, which is not shown clearly in Figure 2. The problems in this case can be summarized as follows. 1) Because the tube depth at contact with the patient’s teeth had already been indicated as 31 cm, the DLT could not be advanced any further to optimally reposition the herniated bronchial cuff—the Broncho-Cath was short to be used in this patient. 2) Moreover, the TrB orifice was already partially obstructed when viewed through the tracheal lumen, indicating that it could become completely obstructed if the tube was advanced further. An air leakage occurred while clamping the connector for the non-dependent lung, and satisfactory OLV required for surgery could not be achieved. Therefore, we decided to replace the existing DLT with a 37-Fr left-sided Human Broncho (Insung Medical Co., Wonju, Korea) that differs from a Broncho-Cath in terms its structure. Under bronchoscopic view after replacing, the bronchial cuff of the DLT showed no herniation and was located to the left just below the tracheal carina, and the TrB orifice was not obstructed by the tracheal lumen (Figure 3). The patient’s vital signs and respiratory parameters were unremarkable without any air leakage during clamping of the connector for the non-dependent lung. In the thoracoscopic view after starting surgery, the operative lung collapse was accomplished, and right upper lobe apex and right lower lobe superior segment bullectomies were performed successfully without any other events. There were no findings of postoperative air leakage; the patient was discharged after chest tube removal and is currently healthy. The patient has provided informed consent for the publication of this case report.
 |
Figure 2 Bronchoscopy view via the tracheal lumen of the double-lumen tube. The orifice of the tracheal bronchus (TrB) was partially obstructed by the tracheal lumen. |
Discussion
A TrB is an aberrant, accessory, or ectopic bronchus that branches directly from the lateral wall of the main trachea. The incidence is reported to be between 0.1% and 5%.4,6 A TrB can originate anywhere between the carina and the cricoid cartilage, but is most commonly observed within 2 cm above the carina.2,3,6–8 Depending on the level at which the TrB arises, anesthesiologist need to use different methods for airway management. The Conacher classification system describes TrB based on the potential challenges to intubation.1 In this widely used system, Type 1 TrB originate at the mid-tracheal level and are accompanied by distal tracheal narrowing,1,3,9 while Type 3 TrB, which are also known as carina trifurcations, arise from the carina.1,8 The level of origin of a Type 2 TrB, characterized by a distal trachea of normal diameter, has been reported as being from 1 cm above the carina to as much as 6 cm from the carina.1,10 The present case can be classified as Type 2 TrB.
As previously described, successful lung isolation can be achieved using a DLT, when the distance between the TrB and carina is close enough to avoid obstruction of the TrB orifice and when the main bronchi do not show anatomical distortion.4 If not, it may be necessary to use a combination of instruments, such as a single-lumen endotracheal tube (SLT) with a bronchial blocker (BB) or a Fogarty catheter.2,3,5,6,9 However, this presents difficulties when right-sided thoracic surgery is performed in the presence of a right-sided TrB, as two BBs are required to block the TrB and bronchus intermedius orifices in order to secure the surgical field of view.3,5,6 In fact, in thoracic surgery requiring OLV, DLTs are preferred over other devices such as BB. A DLT provides excellent lung isolation and can also be used to suction the operative lung when necessary and to apply continuous positive airway pressure.3 Moreover, it allows intraoperative bronchoscopic visualization without interfering with ventilation.3 Therefore, when possible, use of a DLT may be safer for the patient as well as more convenient for the clinician. Lee et al reported three cases of patients with a TrB within 2 cm of the carina (2 cm, 0 cm, and 1 cm above the carina) in which OLV was unsuccessful when using an SLT with BB; the problems were resolved by using a Broncho-Cath.4 On the other hand, in one case, OLV using a Broncho-Cath was not possible even for Type 3 TrB originating next to the carina.9 This case is thought to have resulted from the bronchial lumen of the Broncho-Cath obstructing the bronchial wall due to a left-shifted carina and an apically retracted LMB, causing an excessively acute angle of entry from the carina to the LMB. The authors explained that a flexible DLT with a wire-reinforced bronchial lumen might not have obstructed the bronchus, but that such a product was not available.9
The Human Broncho is a DLT made of silicone. In general, silicone DLTs have a softer body and a more flexible bronchial tip, which helps reduce the incidence of postoperative sore throat.11 Additionally, the Human Broncho has an obtuse angled, non-beveled, and wire-reinforced bronchial segment, and a recent study reported that it showed superior performance of tube railroading over fiberoptic bronchoscope compared to PVC SLTs during tracheal intubation.12 The soft but wire-reinforced bronchial segment is expected to respond flexibly, even if the angle formed by the bronchial cuff with respect to the trachea becomes more acute. Another structural feature of the Human Broncho is that it has a shorter and more distally located bronchial cuff compared to the Broncho-Cath, which reduces the risk of left upper lobe bronchus obstruction, increasing the margin of safety.13 It also makes the gaps between the upper edge of the bronchial cuff and the tracheal lumen opening (distal and proximal end) denoted as (a) and (b) longer in the Human Broncho (3.4, 4.0 cm) than Broncho-Cath (1.8, 2.9 cm; Figure 4A and B). Moreover, the distance from the upper edge of the bronchial cuff to the end of the tracheal segment denoted as orotracheal segment is longer in the Human Broncho (33.5 cm) than the Broncho-Cath (30 cm; Figure 5).
 |
Figure 5 The distance from the upper edge of the bronchial cuff to the end of the tracheal segment denoted as orotracheal segment was 30 cm for the Broncho-Cath and 33.5 cm for the Human Broncho. |
The fact that the orotracheal segment distance is longer means that there is more potential space that could be accommodated from the carina to the mouth corner. In the Broncho-Cath that was initially placed, the bronchial cuff was herniated, but it was impossible to advance the DLT to solve this problem. In a previous study, when determining the permeable range without TrB occlusion, the space from the bronchial cuff to the tracheal cuff14 corresponding to the distance in (c) rather than (a) or (b) of Figure 4 is used. According to this concept, the permeable range (c) in both types of DLT could involve the TrB orifice of our patient (origin height and diameter of 1.9 cm and 1.4 cm, respectively), since the length of (c) is 4.0 cm for the Broncho-Cath and 4.7 cm for the Human Broncho. However, the distance up to the distal edge of the tracheal cuff is only theoretically the most proximal allowable position, and the air flow could be interrupted at the TrB orifice of between (b) and (c) depending on the diameter and deviation of the trachea. Thus, in fact, the TrB inlet was partially blocked from the end of the tracheal lumen of the Broncho-Cath in our patient. Additionally, a 39-Fr Broncho-Cath differs only in diameter, but not in length, from a 37-Fr Broncho-Cath. Therefore, replacing the tube with a 39-Fr Broncho-Cath would not have solved this problem. Fortunately, we succeeded by selecting the Human Broncho as an alternative due to the advantages of DLT over a BB or Fogarty catheter. However, if a Human Broncho is not available or if OLV cannot be achieved due to anatomical problems, traditional alternatives including a BB or Fogarty should be applied, despite being inconvenient.
The structural properties of the Human Broncho, including the greater tracheal orifice gap and the longer orotracheal segment, allowed it to be placed optimally within this patient’s LMB while ensuring enough space to avoid obstruction of the present patient’s TrB orifice originating from 1.9 cm and whose upper margin located up to 3.3 cm over the carina. In conclusion, the use of a Human Broncho for lung isolation in thoracic surgery in patients with a TrB not far from the carina, to which a DLT can be applied, can be considered a useful alternative to a Broncho-Cath.
Ethics Approval and Consent to Participate
Written informed consent was obtained from the patient for publication of this case. Since this study used only de-identified patient data, no approval from the institutional review board (IRB) was required.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Conacher ID. Implications of a tracheal bronchus for adult anaesthetic practice. Br J Anaesth. 2000;85(2):317–320. doi:10.1093/bja/85.2.317
2. Moon YJ, Kim SH, Park SW, Lee YM. The implications of a tracheal bronchus on one-lung ventilation and fibreoptic bronchoscopy in a patient undergoing thoracic surgery: a case report. Can J Anesth. 2015;62(4):399–402. doi:10.1007/s12630-014-0293-8
3. Wiser SH, Hartigan PM. Challenging lung isolation secondary to aberrant tracheobronchial anatomy. Anesth Analg. 2011;112(3):688–692. doi:10.1213/ANE.0b013e318206917a
4. Lee DK, Kim YM, Kim HZ, Lim SH. Right upper lobe tracheal bronchus: anesthetic challenge in one-lung ventilated patients -A report of three cases. Korean J Anesthesiol. 2013;64(5):448–450. doi:10.4097/kjae.2013.64.5.448
5. Lee HL, Ho AC, Cheng RK, Shyr MH. Successful one-lung ventilation in a patient with aberrant tracheal bronchus. Anesth Analg. 2002;95(2):492–493. doi:10.1097/00000539-200208000-00049
6. Agarwal S, Banks MA, Dalela S, Bates WB, Castresana MR. Incidental finding of tracheal bronchus complicating the anesthetic management of a left video-assisted thoracoscopic procedure. J Anaesthesiol Clin Pharmacol. 2016;32(1):106–108. doi:10.4103/0970-9185.168167
7. Ghaye B, Szapiro D, Fanchamps JM, Dondelinger RF. Congenital bronchial abnormalities revisited. Radiographics. 2001;21(1):105–119. doi:10.1148/radiographics.21.1.g01ja06105
8. Sarkar ME, Inbaraj A, Zachariah V, Shukla S. Tracheal bronchus: a rare unforeseen anaesthetic challenge. Indian J Anaesth. 2018;62(8):621–624. doi:10.4103/ija.IJA_180_18
9. Yoshimura T, Ueda KI, Kakinuma A, Nakata Y. Difficulty in placement of a left-sided double-lumen tube due to aberrant tracheobronchial anatomy. J Clin Anesth. 2013;25(5):413–416. doi:10.1016/j.jclinane.2013.01.018
10. Ikeno S, Mitsuhata H, Saito K, et al. Airway management for patients with a tracheal bronchus. Br J Anaesth. 1996;76(4):573–575. doi:10.1093/bja/76.4.573
11. Jeon J, Lee K, Ahn G, Lee J, Hwang W. Comparison of postoperative sore throat and hoarseness between two types of double-lumen endobronchial tubes: a randomized controlled trial. J Cardiothorac Vasc Anesth. 2015;29(1):121–125. doi:10.1053/j.jvca.2014.05.028
12. Yoo JY, Chae YJ, Park SY, Haam S, Kim M, Kim DH. Time to tracheal intubation over a fibreoptic bronchoscope using a silicone left double-lumen endobronchial tube versus polyvinyl chloride single-lumen tube with bronchial blocker: a randomized controlled non-inferiority trial. J Thorac Dis. 2019;11(3):901–908. doi:10.21037/jtd.2019.01.108
13. Kwon NK, Jung SM, Park SJ, Han Y. Comparison of displacement of polyvinyl chloride and silicone left-sided double-lumen tubes during lateral positioning. Korean J Anesthesiol. 2019;72(1):32–38. doi:10.4097/kja.d.18.00012
14. Ho AM, Karmakar MK, Lam WW, et al. Does the presence of a tracheal bronchus affect the margin of safety of double-lumen tube placement? Anesth Analg. 2004;99(1):293–295. doi:10.1213/01.ane.0000118106.09944.e7
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.