Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 14
Use of Septal Cartilage in Rhinoplasty to Correct Nasal Deformity After Unilateral Cleft Lip and Palate Surgery
Authors Nguyen HL , Hoang MP , Nguyen VM, Tran TT, Le VS
Received 5 March 2022
Accepted for publication 11 May 2022
Published 18 May 2022 Volume 2022:14 Pages 131—140
DOI https://doi.org/10.2147/CCIDE.S364332
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Christopher E. Okunseri
Hong Loi Nguyen,1 Minh Phuong Hoang,2 Van Minh Nguyen,2 Tan Tai Tran,2 Van Son Le3
1Odonto-Stomatology Center, Hue Central Hospital, Hue City, Vietnam; 2Faculty of Odonto-Stomatology, Hue University of Medicine and Pharmacy, Hue University, Hue City, Vietnam; 3School of Odonto–Stomatology, Hanoi Medical University, Hanoi, Vietnam
Correspondence: Hong Loi Nguyen, Odonto-stomatology Center, Hue Central Hospital, 16 Le Loi Street, Hue City, 530000, Vietnam, Tel +84913498549, Email [email protected]
Background: The most common facial defect is the congenital cleft lip (CL), which can occur with or without a cleft palate (CP). Patients need primary plastic surgery for rehabilitation and esthetics; nevertheless, secondary abnormalities of the lip and nose may develop after primary surgery. These deformities are complex and involve all tissue layers, including the skeletal platform, inner lining, osseocartilaginous structure, and overlying skin. This study evaluated the results of nasal deformity rhinoplasty using septal cartilage in patients with nasal deformities after plastic surgery for unilateral CL and CP.
Methods: This retrospective study was conducted on 21 patients with secondary unilateral CL nasal deformity between June 2015 and August 2016. All patients underwent rhinoplasty with the use of septal cartilage grafts. Pre- and post-operative nasal forms were measured.
Results: The patients had cosmetic problems and impaired nasal airflow due to distorted anatomy. The postoperative nasal forms were improved in all patients. Rhinoplasty using septal cartilage effectively increased the height of the columella and nose and improved the balance of the base width and the length of both sides of the nose. Excellent results were achieved in 18 patients. Three patients showed good results. No patient showed a fair result.
Conclusion: This study demonstrated an effective correction of esthetic deformities and significant improvement in airway patency. A long-term longitudinal study is still required to evaluate the influence of septal cartilage harvesting on face and nasal development until children reach their late teens.
Keywords: nasal deformity, unilateral cleft deformity, secondary rhinoplasty, septal cartilage
Corrigendum for this paper has been published.
Introduction
Cleft lip (CL) and cleft palate (CP) are common maxillofacial birth defects that cause structural changes, greatly affecting function, facial aesthetics, and psychological health from childhood to adulthood.1,2 One in 750 neonates suffers from CL and CP worldwide. Cleft defects are caused by various causes, including genetics, environment, and socioeconomic status.3,4 Plastic surgery to reconstruct the lip and palate is necessary for these kinds of patients. Several technical methods of reconstruction exist; currently, surgeons often apply the two methods of Millard and Tennison.5–9 Several surgeons have improvised these methods to achieve better outcomes.10,11 However, Millard found that after the first phase of plastic surgery, patients required follow-up appointments and second-phase surgery.12 Cohen et al believe that no method of lip reconstruction achieves perfect results after one phase of surgery alone.13
Correction of the nasal deformity in CL patients, which involves abnormalities in all layers, including the skin, cartilage, vestibular portion, and basal bone, remains a challenge for maxillofacial surgeons. Patients frequently have a shorter and deviated columella, an asymmetric nasal tip and nostril, a flattened ala, and a low alar base. The nasal septum is typically deviated in clinical individuals with unilateral cleft lip and palate (UCLP), resulting in variable degrees of nasal obstruction.14 The three main factors involved in nasal deformity are the lack or deviation of congenital anatomical structures, surgical scarring from previous surgical attempts, and developmental variability.15 Therefore, cleft lip nasal deformities commonly pose a challenge for surgeons. They usually focus on the cosmetic elements of cleft lip nasal abnormalities while ignoring the nasal airway functioning.16–18
In recent years, innovative procedures for correcting the characteristic nasal abnormalities of UCLP have been developed, for example, upper and/or lower lateral cartilage suspension, V-Y chondromucosal composite flap, and cartilage grafts such as rib cartilage, ear cartilage,19–24 but it is difficult to conclude which is the most reliable technique for patients with cleft nasal deformities.18,25
Gubisch believed that the excised septum is a precondition for correcting a deviated nose.26 We used the septal cartilage that was harvested during anterior palatoplasty to reinforce the cleft-side alar cartilage; this method was inspired by the method recommended by several authors for the initial repair of septal cartilage deformity. In this study, we analyzed nasal symmetry results and ventilation function in patients with complete unilateral cleft lip and nose abnormalities and the manner of their alterations depending on whether primary nasal repair using a septal cartilage graft was performed.
Materials and Methods
Patients
A retrospective study was performed on 21 patients with UCLP who underwent primary cheiloplasty and palatoplasty surgery but had nasal deformities which required adjustment. These patients visited two odonto-stomatology centers (one in Hanoi and one in Hue City) for examination and treatment from June 2015 to August 2016. The enrolled patients with secondary unilateral CL nasal deformity were ≥ 14 years old and met the health criteria for surgery under anesthesia. Patients who had undergone surgery to alter the lip and/or nose within the previous six months or had an infection in the region of surgery were excluded.
All patients were of Kinh nationality from Red River Delta and the central of Vietnam who presented nasal deformities with or without nasal obstruction and was diagnosed with nonsyndromic complete unilateral CL nasal deformity. Informed consent was sent to the patients before the surgery.
Basal and lateral view 1:1 ratio photographs of all patients were taken at the same distance and under the same lighting circumstances in a 1:1 ratio. Two evaluators (M.P.H. and V.M.N) used digital analytic software (Photoshop CC, Version 2014.2.2; Adobe Systems, Inc., San Jose, Calif.) to gather all measures.
The nasal symmetry was assessed using metrics collected from frontal, lateral, and basal view pictures taken before surgery and during follow-up visits (7 days, 3 months, and 6 months postoperatively).
Each patient was carefully consulted, admitted to the hospital, fully preoperatively tested, and clinically examined.
Anthropological Measurements
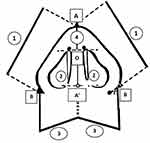
Definitions of the outcomes and measurements are shown in Figure 1.
NOSE Questionnaire Data Analysis
Patients filled out a preoperative and postoperative Nasal Obstruction Symptoms Evaluation (NOSE) questionnaire.9,27 Before nose surgery and during each postoperative appointment, this questionnaire data were collected from patients’ medical records. The records from the final follow-up questionnaire were used in the postoperative analysis of the NOSE questionnaire.
Surgical Procedures
Step 1: Preparing the patient. After the patient was anesthetized with tracheal intubation, the outer and inner nasal regions were disinfected using betadine. Then, a local anesthetic was administered along with a vasoconstrictor.
Step 2: Making an incision, a bilateral reverse-U and a transcolumellar incision were used
Step 3:Separated structures (upper lateral cartilages, lower lateral cartilages, and alar base from abnormal attachment), and exposed septal cartilage.
Step 4: Isolated the nasal septum from the anterior nasal spine by cutting the deviated septum cartilage, leaving a 1.5-cm margin with the nasal dorsal and nasal columella.
Step 5: Shaped the grafting cartilage and positioned it to reform the nose.
Step 6: Surgically shortening the base of the nose. After reconstructing the nasal septum, pillar, tip and ala, additional reduction of the nasal ala could be performed if necessary. The skin was dissected at the scar area using an elliptical excision. The base of the nose was sutured with Vicryl 5-0 and Nylon 6-0.
Step 7: Placed the skin of the tip of the nose at the original position and evaluated the form of the nose.
Step 8: Placing the nasal conformer to maintain the position of the septum and the shape of the reconstructed nose (Figure 2).
Evaluation of the Improvement in the Nasal Condition Postoperatively
The assessment of nasal symmetry was based on measurements from the basal view photographs taken during the follow-up visits (at least 3-year follow-up).
We evaluated patients at 7 days, 3 months, and 6 months after surgery and divided them into 3 levels based on the improvement of 5 remaining nasal deformities after surgery, including asymmetric nasal tips, flattened alae, wide nasal bases, low alar bases, and non-ventilated nasal passages. When all five characteristics improved, the level of nasal improvement after surgery was classified as excellent, followed by good (4 out of 5 characteristics improved), and fair (≤ 3 out of 5 characteristics improved).
Data Analysis
The non-parametric Wilcoxon signed-rank test was used to assess the statistical significance of differences between the cleft and non-cleft sides, and between pre- and post-operative measurements. A value of P < 0.05 yielded 95% confidence interval. All statistical analyses were conducted using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA).
Results
There were 21 patients (9 males and 12 females) in our study, with the mean age being relatively equal in both the male and female participants (18.7 ± 3.4 years and 19.1 ± 3.3 years, respectively). The features of nasal deformity remaining after unilateral CL surgery are shown in Table 1. A flat ala was present in 21 patients (100%) and a wide nose base in 18 (85.7%) patients. These characteristics were the most common in our patients, followed by the asymmetric nasal tip in 15 patients (71.4%) and a low alar base in 3 patients (14.3%).
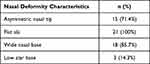 |
Table 1 Remaining Nasal Deformity Characteristics After Unilateral Cleft Lip Surgery |
Ventilation Function of the Nose Before Surgery
Patients with facial clefts present with varying degrees of nasal obstruction. We used the NOSE data to evaluate the nasal ventilation functions. Regarding the ventilation function of the nose before surgery, 19 patients, accounting for 90.5%, had a clearly ventilated nose, and only 2 patients (9.5%) had a non-ventilated nose.
Clinical Characteristics After Surgery
Most of the clinical features improved immediately after surgery; only 3 patients (14.3%) had a wide nose base postoperatively. Features such as asymmetric nasal tips, flat alae, and low alar bases demonstrated improvement.
Ventilation Function of the Nose After Surgery
Postoperatively, all patients (100%) had a clearly ventilated nose reflected by NOSE Questionnaire Data Analysis.
Columella Height and Nasal Height
The results revealed that the mean columella height was 2.81 ± 0.87 mm higher than before surgery. The average nasal height increased by 3.40 ± 1.30 mm after the nasal deformity surgery (Table 2).
 |
Table 2 Columella and Nasal Height (7 Days After Surgery) |
The width of alar base on the cleft side pre-operative’s highest value is 21.5mm, the smallest is 14.0mm and the average is 17.55±2.29mm and the highest after surgery is 20.5mm, the smallest is 12.5mm, the average is 15.83±2.22mm. The maximum nasal alar length on the cleft side before surgery is 30.5mm, the smallest is 24.0mm, the average is 26.29±2.04mm, the highest after surgery is 31mm, the smallest is 23mm, the average is 26.29±2.04mm. 26.81±2.13mm (as shown in Tables 3 and 4).
 |
Table 3 Width of Alar Base (7 Days After Surgery) |
 |
Table 4 Nasal Alar Length (7 Days After Surgery) |
The degree of nasal improvement after surgery was assessed at 7 days, 3 months, and 6 months after surgery. At 7 days after surgery, 18 patients demonstrated excellent results (85.7%), three had very good results (14.3%), while none of them had only good results. At the 3-month follow-up, the same number of patients had excellent results, two patients (9.5%) had good results, and 1 patient (4.8%) had fair results. In the 15 patients that were followed up after 6 months, 13 patients (86.7%) had excellent results, 2 (13.3%) had good results, and none had fair results (as shown in Figures 3 and 4).
 |
Figure 3 Nasal deformity on the right side. Front and basal view photographs taken preoperatively (A), 7 days postoperatively (B), and 3 months postoperatively (C). |
 |
Figure 4 Nasal deformity on the left side. Front and basal view photographs taken preoperatively (A), 7 days postoperatively (B), and 3 months postoperatively (C). |
Discussion
Characteristics of Nasal Deformity in Patients After Unilateral CL and Palate Surgery
In our study, the proportion of female patients was higher than that of male patients and this ratio is similar to that observed in the study conducted by Jeong et al.18
The appropriate age for rhinoplasty to correct nasal deformity is still being discussed, considering the development of the nose and lips and the occurrence of secondary deformities after corrective surgery. According to Pawar et al, Cuzalina et al, and Jonnalagadda et al, final-phase rhinoplasty should be performed after the completion of the maxillary and nasal growth.15,20,28 Final-phase rhinoplasty is usually performed at 14–16 years of age in women and 16–18 years in men. In our study, the youngest patient was 14 years old, and the oldest was 27, while the most frequently observed patient age was 19 years (5 patients, accounting for 23.8%). The mean age of patients was relatively equal in both the male and female sexes, 18.7 ± 3.4 years and 19.1 ± 3.3 years, respectively.
The goal of this surgery was to create long-term symmetry, improve the form of the base and tip of the nose, reduce nasal congestion, and manage nasal scarring.15,20,28
Remaining Features of Nasal Deformity After Unilateral CL Surgery
This study investigated the most common clinical deformities that remain after CL surgery, including asymmetric nasal tips, flattened alae, wide nasal bases, low alar bases, and non-ventilated nasal passages. Most of the patients had these characteristics, which were consistent in previous studies.23,29,30 Espel et al studied 50 patients that had undergone unilateral CL surgery, and 48 patients had a flattened alar (96%), 24 patients had a deviated nasal columella (48%), and 28 patients had wide nostrils (56%).31
Out of our 21 surgical patients, 19 (90.5%) had a clear nasal passage, and only two patients (9.5%) had a non-ventilated nose preoperatively. According to Cohen et al, the problem of nasal ventilation was less crucial during the final phase of rhinoplasty. Few authors have agreed with the practice of performing concurrent septal reconstruction or reducing the nasopharynx at the time of the surgical correction of nasal deformities; however, little attention has been paid to the functional outcomes achieved after reconstruction. Consequently, very few functional outcomes of nasal ventilation have been reported.13
According to a study by Hens et al, nasal obstruction was the motivating factor for undergoing second-phase rhinoplasty in 97% of their patients, thus highlighting the importance of considering the functional aspects of second-phase rhinoplasty and the need for further research on this topic.32 Huempfer-Hierl et al performed a prospective study among 68 patients undergoing second-phase rhinoplasty and assessed the functional activity using a nasal barometer first preoperatively and then 6 months postoperatively.33 Analysis of the respiratory function data demonstrated a significant increase in nasal volume and high patient satisfaction.
According to Massie et al, septal deviation often occurs in patients with CL and CP.34 Despite this finding, the influence of septal bone and cartilage on nasal obstruction in these patients is not well understood. The author performed a retrospective study on a group of patients undergoing cone-beam computed tomography from November 2011 to July 2015. Of the 40 study participants, 24 were CL and CP patients, and 16 were age-controlled individuals who formed the control group. The results showed that patients with CL and CP had significantly increased nasal obstruction compared to the control group.
Short-Term Results After Rhinoplasty Using Nasal Septum Cartilage on Patients Who Had Unilateral CL Surgery
In our study, the heights of the columella and nose on the cleft side pre- and post-operatively had a significant difference. These findings are similar to those in other studies that used other alternative graft materials.30,35–37 Therefore, rhinoplasty using septal cartilage in patients who have had unilateral CL surgery effectively increases the height of the nose and columella. The hypoplastic cartilage was compensated for using a septal cartilage graft, which acts as a supporting framework for the skin and subcutaneous tissue.
During surgery to close the CL in the first phase, the surgeon always measures the size of the non-cleft side of the nose and uses this size as the target measurement for the nose on the cleft side. According to He et al, the base of the nose on the cleft side is always wider than that on the other side in cases of unilateral CL. In addition, the base of the nose not only lacks in skin and muscle, but also in bone. There are almost no cases where the size of the nasal base on the cleft side is equal to or narrower than the unaffected side. This enlargement is partially the result of the deformity secondary to the contraction of the orbicularis oris muscle during development. Surgery to narrow the base of the nose is always necessary in cases of second-phase rhinoplasty.38
In our study, the width of the alar base on the non-cleft side after surgery was almost equal to that on the cleft side, which demonstrated the symmetry of the nasal base postoperatively. Thus, the surgery effectively balanced the width of the nasal base on both sides.
According to Rossell-Perry et al, the width of the alar base on the cleft side before and after surgery was 21.92 ± 1.61 mm and 18.11 ± 2.86 mm, respectively (p = 0.001). The width of the alar base on the non-cleft side and the cleft side after surgery was 17.33 ± 2.66 mm and 18.11 ± 2.86 mm, respectively (p = 0.21). This demonstrated that the difference in the width of the alar base between the healthy side and the cleft side was not statistically significant.39
Before surgery, the alar length on the cleft side was usually longer than that of the non-cleft side. After surgery, the two lengths were nearly equal, which shows that symmetry of the nose was achieved postoperatively (Table 4). Thus, the surgery effectively balanced the length of both sides of the nose.
Evaluation of the Improvement in the Nasal Condition After Surgery
The level of nasal improvement was assessed at 7 days, 3 months, and 6 months after surgery. At 7 days after surgery, excellent results accounted for 85.7%, good results accounted for 14.3%, and no patients had fair results alone. At the 3-month follow-up, the excellent rate remained unchanged, two patients (9.5%) had good results, and one patient (4.8%) had fair results. In the 15 patients followed up at 6 months after surgery, 13 patients (86.7%) had excellent results, two had good results (13.3%), and none had fair results. The patients also had a follow-up visit at 1 month; however, those results were not different from the nose condition observed 7 days after surgery.
Almost no complications were recorded after surgery, which may have been due to the patients being consulted, tested, operated on, cared for postoperatively, and thoroughly re-examined. No cases of infection, cartilage loss, or change in nasal size occurred. An advantage of our study was that the patients were admitted and operated on at 2 major odonto-stomatology centers so that surgical procedures and postoperative care could be performed more carefully. Additionally, these patients were especially interested in the function and esthetics of their noses, so they adhered well to the treatment process and periodical re-examinations.
Conclusion
Despite recent breakthroughs in primary cheiloplasty in individuals with ULCP, variable outcomes persist. Our first data show that applying septal cartilage as a graft during primary rhinoplasty may yield improved nose morphologies, enhance ventilation function, and correct most nasal abnormalities postoperatively. The surgery effectively increased the height of the columella and nose and improved the balance of the base width and the length of both sides of the nose. A long-term longitudinal research is still required to evaluate the influence of septal cartilage harvesting on face and nasal development until children reach their late teens.
Compliance with Ethical Standards
The study complied with the Declaration of Helsinki Ethical Principles for Medical Research.
Ethical Approval and Consent to Participate
Ethical approval was obtained from the institutional review board of Hanoi Medical University (Hanoi, Vietnam) and Hue Central Hospital (Hue city Vietnam). Written informed consent was taken from each participant or parents/legal guardians for pediatric patients for publication of the data and accompanying images.
Funding
This research is not funded by any organization.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Dixon MJ, Marazita ML, Beaty TH, Murray JC. Cleft lip and palate: understanding genetic and environmental influences. Nat Rev Genet. 2011;12(3):167–178. doi:10.1038/nrg2933
2. Gee GC, Payne-Sturges DC. Environmental health disparities: a framework integrating psychosocial and environmental concepts. Environ Health Perspect. 2004;112(17):1645–1653. doi:10.1289/ehp.7074
3. Mai CT, Isenburg JL, Canfield MA, et al. National population-based estimates for major birth defects, 2010–2014. Birth Defects Res. 2019;111(18):1420–1435. doi:10.1002/bdr2.1589
4. Derijcke A, Eerens A, Carels C. The incidence of oral clefts: a review. Br J Oral Maxillofacial Surg. 1996;34(6):488–494. doi:10.1016/S0266-4356(96)90242-9
5. Knežević P, Vuletić M, Blivajs I, Dediol E, Macan D, Virag M. The modification of rotation - advancement flap made in 1950. Acta Stomatol Croat. 2017;51(1):60–64. doi:10.15644/asc51/1/8
6. Freitas R, Alves P, Shimizu G, et al. Beyond fifty years of Millard’s rotation-advancement technique in cleft lip closure: are there many “Millards”? Plast Surg Int. 2012;2012:731029. doi:10.1155/2012/731029
7. Sharma R. Triangular flap technique for unilateral cleft lip deformity. J Cleft Lip Palate Craniofacial Anomalies. 2021;8(2):163–168.
8. Cutting CB, Dayan JH. Lip height and lip width after extended Mohler unilateral cleft lip repair. Plast Reconstr Surg. 2003;111(1):
9. Fisher MD, Fisher DM, Marcus JR. Correction of the cleft nasal deformity: from infancy to maturity. Clin Plast Surg. 2014;41(2):283–299. doi:10.1016/j.cps.2014.01.002
10. Mulliken JB, Martínez-Pérez D. The principle of rotation advancement for repair of unilateral complete cleft lip and nasal deformity: technical variations and analysis of results. Plast Reconstr Surg. 1999;104(5):1247–1260. doi:10.1097/00006534-199910000-00003
11. Stal S, Brown RH, Higuera S, et al. Fifty years of the Millard rotation-advancement: looking back and moving forward. Plast Reconstr Surg. 2009;123(4):1364–1377. doi:10.1097/PRS.0b013e31819e26a5
12. Millard D. Primary Nasal Correction. Cleft Craft. The Evolution of Its Surgery I. The Unilateral Deformity. Boston: Little, Brown and Company; 1976.
13. Cohen M, Morris DE, White AD, Patel P. Functional and aesthetic correction of secondary unilateral cleft lip nasal deformities. Indian J Plast Surg. 2009;42:91–101. doi:10.4103/0970-0358.57195
14. Sipilä J, Suonpää J. A prospective study using rhinomanometry and patient clinical satisfaction to determine if objective measurements of nasal airway resistance can improve the quality of septoplasty. Eur Archiv Oto Rhino Laryngol. 1997;254(8):387–390. doi:10.1007/BF01642556
15. Cuzalina A, Jung C. Rhinoplasty for the cleft lip and palate patient. Oral Maxillofac Surg Clin North Am. 2016;28(2):189–202. doi:10.1016/j.coms.2015.12.002
16. Vass G, Mohos G, Bere Z, et al. Secondary correction of nasal deformities in cleft lip and palate patients: surgical technique and outcome evaluation. Head Face Med. 2016;12(1):34. doi:10.1186/s13005-016-0132-y
17. Nakamura N, Sasaguri M, Okawachi T, Nishihara K, Nozoe E. Secondary correction of bilateral cleft lip nose deformity - Clinical and three-dimensional observations on pre- and postoperative outcome. J Cranio Maxillo Facial Surg. 2011;39(5):305–312. doi:10.1016/j.jcms.2010.05.008
18. Jeong HS, Lee HK, Shin KS. Correction of unilateral secondary cleft lip nose deformity by a modified Tajima’s method and several adjunctive procedures based on severity. Aesthetic Plast Surg. 2012;36(2):406–413. doi:10.1007/s00266-011-9788-7
19. Angelos P, Wang T. Revision of the cleft lip nose. FPS. 2012;28(4):447–453. doi:10.1055/s-0032-1319838
20. Pawar SS, Wang TD. Secondary cleft rhinoplasty. JAMA Facial Plast Surg. 2014;16(1):58–63. doi:10.1001/jamafacial.2013.1562
21. Kiya K, Oyama T, Taniguchi M, Hosokawa K. Simultaneous correction of deviated columella and wide nostril floor using the Y-V advancement in unilateral cleft lip nasal deformities. JPRAS. 2014;67(5):721–724. doi:10.1016/j.bjps.2013.12.006
22. Sakamoto Y, Miyamoto J, Tamada I, Kishi K. Nasal tip surgery for cleft nose in Asians. J Craniofac Surg. 2014;25(5):1671–1673. doi:10.1097/SCS.0000000000001112
23. Zhang L, Bai X, Li Z, et al. Improvement of aesthetic and nasal airway in patients with cleft lip nasal deformities: rhinoplasty with septal cartilage graft and septoplasty. Cleft Palate Craniofacial J. 2018;55(4):554–561. doi:10.1177/1055665617746260
24. Hafezi F, Naghibzadeh B, Ashtiani AK, Mousavi SJ, Nouhi AH, Naghibzadeh G. Correction of cleft lip nose deformity with rib cartilage. Aesthet Surg J. 2013;33(5):662–673. doi:10.1177/1090820X13488133
25. Burstein F. Surgical treatment of the nasal-maxillary complex in adolescents with cleft lip and palate. J Craniofac Surg. 2007;18:748–755. doi:10.1097/scs.0b013e3180684339
26. Gubisch W. The extracorporeal septum plasty: a technique to correct difficult nasal deformities. Plast Reconstr Surg. 1995;95(4):672–682. doi:10.1097/00006534-199504000-00008
27. Stewart MG, Witsell DL, Smith TL, Weaver EM, Yueh B, Hannley MT. Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngology. 2004;130(2):157–163. doi:10.1016/j.otohns.2003.09.016
28. Jonnalagadda A, Jami S, Pydi KL. Cleft lip rhinoplasty - a review. Sci J Clin Med. 2016;5(4–1):20–26.
29. Nakamura N, Okawachi T, Nishihara K, Hirahara N, Nozoe E. Surgical technique for secondary correction of unilateral cleft lip-nose deformity: clinical and 3-dimensional observations of preoperative and postoperative nasal forms. J Oral Maxillofacial Surg. 2010;68(9):2248–2257. doi:10.1016/j.joms.2009.06.012
30. Masuoka H, Kawai K, Morimoto N, Yamawaki S, Suzuki S. Open rhinoplasty using conchal cartilage during childhood to correct unilateral cleft-lip nasal deformities. JPRAS. 2012;65(7):857–863. doi:10.1016/j.bjps.2012.01.002
31. Espel P, Garay OM. Photogrammetric analysis of the alterations in nasal cartilaginous and soft tissue structures in patients operated for unilateral cleft lip and palate. Cir Plást Iberolatinoam. 2014;40(1):87–92.
32. Hens G, Picavet VA, Poorten VV, Schoenaers J, Jorissen M, Hellings PW. High patient satisfaction after secondary rhinoplasty in cleft lip patients. Int Forum Allergy Rhinol. 2011;1(3):167–172. doi:10.1002/alr.20023
33. Huempfner-Hierl H, Hemprich A, Hierl T. Results of a prospective anthropometric and functional study about aesthetics and nasal respiration after secondary rhinoplasty in cleft lip and palate patients. J Craniofac Surg. 2009;20(Suppl 2):1863–1875. doi:10.1097/SCS.0b013e3181b6c6fb
34. Massie JP, Runyan CM, Stern MJ, et al. Nasal septal anatomy in skeletally mature patients with cleft lip and palate. JAMA Facial Plast Surg. 2016;18(5):347–353. doi:10.1001/jamafacial.2016.0404
35. Sàndor GK, Ylikontiola LP. Patient evaluation of outcomes of external rhinoplasty for unilateral cleft lip and palate. Int J Oral Maxillofac Surg. 2006;35(5):407–411. doi:10.1016/j.ijom.2006.01.020
36. Lu TC, Yao CF, Lin S, Chang CS, Chen PK. Primary septal cartilage graft for the unilateral cleft rhinoplasty. Plast Reconstr Surg. 2017;139(5):1177–1186. doi:10.1097/PRS.0000000000003297
37. Matsuo K, Hirose T. Secondary correction of the unilateral cleft lip nose using a conchal composite graft. Plast Reconstr Surg. 1990;86(5):991–995. doi:10.1097/00006534-199011000-00028
38. He X, Shi B, Jiang S, et al. 110 infants with unrepaired unilateral cleft lip: an anthropometric analysis of the lip and nasal deformities. J Oral Maxillofac Surg. 2010;39(9):847–852. doi:10.1016/j.ijom.2010.04.007
39. Rossell-Perry P, Romero-Narvaez C. Evaluation of the use of auricular composite graft for secondary unilateral cleft lip nasal alar deformity repair. Plast Surg Int. 2014;2014:270285. doi:10.1155/2014/270285
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.