Back to Journals » Patient Preference and Adherence » Volume 15
Use of GELSECTAN® in Patients with Irritable Bowel Syndrome (IBS): an Italian Experience
Authors Bellini M, Berti G, Bonfrate L, Ciranni F, Di Ciaula A, Di Ruscio M, Dell'Era A , Lambiase C, Noto A, Pancetti A, Portincasa P, Rettura F
Received 12 May 2021
Accepted for publication 4 August 2021
Published 13 August 2021 Volume 2021:15 Pages 1763—1774
DOI https://doi.org/10.2147/PPA.S318859
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Massimo Bellini,1 Ginevra Berti,1 Leonilde Bonfrate,2 Flavia Ciranni,1 Agostino Di Ciaula,2 Mirko Di Ruscio,3 Alessandra Dell’Era,4,5 Christian Lambiase,1 Antonino Noto,2 Andrea Pancetti,1 Piero Portincasa,2 Francesco Rettura1
1Gastrointestinal Unit, Department of Translational Research and New Technologies in Medicine and Surgery, University of Pisa, Pisa, Italy; 2Clinica Medica A. Murri, Department of Biomedical Sciences and Human Oncology, University of Bari Aldo Moro Medical School, Bari, Italy; 3IBD Unit, IRCCS Ospedale Sacro Cuore-Don Calabria, Negrar di Valpolicella, Verona, Italy; 4Department of Biomedical and Clinical Sciences, “Luigi Sacco”, University of Milan, Milan, Italy; 5Gastroenterology and Endoscopy Unit – ASST Fatebenefratelli Sacco, Milan, Italy
Correspondence: Francesco Rettura
Gastrointestinal Unit, Department of Translational Research and New Technologies in Medicine and Surgery, University of Pisa, Pisa, Italy
Tel +39 50 997411
Fax +39 50 997412
Email [email protected]
Abstract: Irritable bowel syndrome is a chronic functional gastrointestinal disorder characterized by recurrent chronic abdominal pain and impaired bowel habits, which affects daily activity and work productivity, and is associated with a significant healthcare economic burden as well as an impaired quality of life and psycho-affective profile. Management of patients is a great challenge for physicians; at the present, the therapeutic strategy aimed to treat the different symptoms, and no medical therapy is proven to modify the natural history of the disease. GELSECTAN® (xyloglucan, pea protein and tannins, xylo-oligosaccharides) is a medical device with both protective and prebiotic actions on the intestinal mucosa, able to restore intestinal permeability and to improve gastrointestinal symptoms, controlling diarrhoea, abdominal pain and bloating in adult patients with irritable bowel syndrome. We report and discuss four cases of different patients with irritable bowel syndrome successfully managed with Gelsectan in the real clinical practice. Literature data, as well as these case reports, show that this device is effective and safe in improving symptoms and bowel habits associated to irritable bowel syndrome; its efficacy and safety were confirmed for the long-term use too. Agents with film-forming protective properties, such as Gelsectan, represent a new alternative therapeutic option for the management of patients with irritable bowel syndrome.
Keywords: irritable bowel syndrome, GELSECTAN®, xyloglucan, tannins, xylo-oligosaccharides
Introduction
Irritable bowel syndrome (IBS) is a chronic functional gastrointestinal disorder characterized by recurrent chronic abdominal pain and impaired bowel habits (constipation, diarrhoea or both), in absence of detectable organic cause (Rome IV criteria).1 This syndrome represents the most common functional gastrointestinal disorder in primary and secondary care.2 The worldwide prevalence of IBS is about 4%3 and it is significantly higher in women than in men. Several factors play a role in the pathophysiology of IBS, including genetic predisposition, gastrointestinal motility, visceral hypersensitivity, increased intestinal permeability, immune system, a low grade of inflammation, alterations in intestinal microbiota, and food sensitivity.4,5 Four subgroups of IBS patients have been identified according to the predominant stool pattern by using the Bristol Stool Form Scale (BSFS):6 IBS with predominant diarrhoea (IBS-D), IBS with predominant constipation (IBS-C), IBS with mixed stool pattern (IBS-M), and IBS unclassified (IBS-U).7 IBS is not a life-threatening disease, but it deeply modifies the patients’ quality of life (QoL) with consequences on their psycho-affective profile.8 It is frequently associated to a heavy socio-economic burden due to absenteeism from work, frequent diagnostic tests and medical checkups.9,10 Moreover, the consumption of healthcare resources is increased by the fact that adequate therapies, able to globally treat IBS digestive symptoms and comorbidities, are not yet available.11
Management of IBS-D patients is a great challenge for physicians; at the present, the therapeutic strategy is aimed to treat the different symptoms. The first-line approach includes dietary modifications, antidiarrhoeals, and antispasmodic drugs. The second-line approach includes bile acid sequestrants, antidepressants, 5-hydroxytryptamine (serotonin) 3 receptor antagonists, antibiotics, probiotics, and psychological therapies. However, all these therapeutical strategies often obtain only partial and unsatisfactory results.12 This is probably due to the multifaceted, and not yet completely known, pathophysiology. Thus, the major efforts are directed towards predominant symptoms of IBS patients, acting by modulating the pathophysiological mechanisms in IBS.13 However, no medical therapy is proven to modify the natural history of IBS and its fluctuating course.
Due to the fact that an intestinal barrier alteration, associated with immune activation, is a possible pathophysiologic mechanism of the IBS,14 a new interesting approach could be aimed to improve the gut permeability correcting the possible mucosal intestinal barrier alteration. The mucosal intestinal barrier includes polarized epithelial cells, joined by tight junctions (TJs),15 which are made by different proteins such as claudins, major components responsible for the barrier’s permeability and polarity of the epithelial cells.16 Mucine networks, fibrillar aggregates of mucin glycoproteins, forming a protective shield on the epithelium above the mucosa, are another important element of the barrier.17–19 If this protective barrier is impaired, the mucosa can be easily crossed by pathogens with consequent inflammatory disorders and altered permeability. In this perspective, film-forming mucosal protective agents,20 such as Xyloglucan (XG), have been recently suggested as valuable therapeutic devices.
The novel formulation GELSECTAN® (Legal manufacturer: DEVINTEC SAGL, Switzerland. Italian distributor: Norgine Italia S.r.l., Italy), containing XG, pea protein and tannins (PPT) from grape seed extract, and xylo-oligosaccharides (XOS), is a medical device with both protective and prebiotic actions on the intestinal mucosa, able to restore intestinal permeability and to improve gastrointestinal symptoms.21
XG has proven to be able to restore the physiological function of the mucosal intestinal barrier due to its mucosal protective properties.15 It is a non-ionic, neutral, branched polysaccharide derived from the tamarind seed (Tamarindus indica) and it consists of a cellulose-like backbone carrying xylose and galactosyl-xylose substituents. Four types of oligosaccharides are allocated as repeating units (an heptasaccharide, two types of octasaccharide and a nonasaccharide). Monomer units contains three types of sugars (xylose, galactose and glucose) at a molar ratio of 2.25:1:2.8.22,23 XG has a configuration resembling mucin molecular structure (known as “mucin-like”), giving optimal mucoadhesive properties and enabling it to act as a physical barrier. It builds a protective film on the mucosa, acting as a barrier against pathogens, allergens and proinflammatory agents.15 The beneficial role of XG was also demonstrated for the treatment of acute diarrhoea in adults and children.18,24 PPT complexes showed a strong antioxidant activity by inhibiting in vitro lipid peroxidation and lipoxygenases and scavenging radicals.25 PPT is also a mucoprotective agent.21 XOS, sugar polymers of xylose units, are prebiotics known to exert a beneficial effect via a bifidogenic effect in the colon.21 XOS increase the number of Bifidobacterium and Akkermansia bacteria in the colon leading to anti-oxidant, anti-allergy or anti-inflammatory activities.26
In a rat model of IBS, Gelsectan was able to inhibit stress-induced visceral hypersensitivity and gut hyperpermeability, providing a preclinical rational for its use in IBS-D patients.27 Gelsectan is indicated for symptomatic relief and prophylaxis of chronic or relapsing diarrhoea, abdominal pain, bloating and flatulence, both in patient with IBS-D. A recent multicentre, double-blind, placebo-controlled, randomised, crossover clinical trial supports the efficacy and safety of Gelsectan for controlling diarrhoea, abdominal pain and bloating in adult patients with IBS-D.21
In this publication, 4 patients with IBS-D treated with Gelsectan in Italian reference centers will be discussed; all patients have provided consent for the publication of the cases.
Case Reports
IBS, Bile Acid Malabsorption or Both?
A 72-year-old woman with a history of hypertension, cervical arthrosis and a long-lasting IBS-D characterized by recurrent abdominal pain, fecal urgency, and 3–4 daily bowel movements (BSFS: 5–6), referred to the Gastrointestinal Unit of the University of Pisa for symptoms worsening. She reported watery diarrhoea (10 daily bowel movements, BSFS: 7) for four weeks with a significant impairment of frequency and severity of abdominal pain, bloating, defecation urgency with occasional fecal incontinence. Melena, haematochezia and lactose intolerance were not reported, such as the use of antibiotics and laxatives. Recent travels and contacts with sick people were ruled out. Digestive symptoms were evaluated through the IBS Severity Scoring System (IBS-SSS)28 (Figure 1A and B: T0) and a homemade questionnaire in which the symptoms were assessed by a visual analogue scale (VAS),29 where 0 means lack of the symptom and 10 means the greatest possible symptom severity (Figure 2: T0). She also reported weight loss (3 kg in the previous 2 months) and an impaired quality of life, evaluated by using 36-item Short Form Health Survey (SF-36) questionnaire,30–33 mainly linked to the domains: role limitations (emotional problems), vitality, emotional well-being, social functioning, general health and health change (Figure 3: T0).
The patient was treated with ramipril and magaldrate, as well as on demand non steroidal anti-inflammatory drugs and tapentadol for pain due to cervical arthrosis. Physical examination was unremarkable, except for abdominal tenderness.
After the clinical assessment, the following tests were prescribed:
- Routine blood tests, inflammation activity indices, celiac serology, thyroid-stimulating hormone, stool culture, test for ova and parasites, Clostridium difficile toxin and fecal calprotectin. All tests were within the normal range, apart from fecal calprotectin (454 mg/Kg).
- Abdominal ultrasound showed only moderate liver steatosis.
- Colonoscopy with biopsies ruled out inflammatory bowel disease and microscopic colitis.
- Upper Digestive Endoscopy with gastric and duodenal biopsies did not show organic lesions or an infection by Helicobacter pylori. No histological changes of duodenal mucosa were observed.
A treatment with mebeverine hydrochloride (200 mg capsules twice a day) and diosmectite (one sachet twice a day) was recommended. At a check control 6 weeks after the first clinical assessment (T1), symptoms were practically unchanged (Figures 1–3). A new assessment of fecal calprotectin (on 3 samples collected in three consecutive days) and a dosage of gastrointestinal hormone levels (gastrin, pancreatic polypeptide, vasoactive intestinal peptide, chromogranin A, urinary 5-hydroxyindoleacetic acid) were suggested. Moreover, a SeHCAT (75-selenium homocholic acid taurine) test to detect a possible bile acid malabsorption, was prescribed.34 Gelsectan at the scheduled dose for two tablets twice a day, was prescribed.
After further six weeks (visit T2), the patient reported an improvement of the IBS-SSS, the bowel symptom questionnaire and the following domains of SF36: role limitations (emotional problems), vitality, emotional well-being, social functioning, pain, general health and health change (Figures 1–3).
The levels of gastrointestinal hormones were within the normal range and the levels of fecal calprotectin on three samples were only slightly above the normal ranges (63, 72, 87 mg/kg). Conversely, the SeHCAT test showed a 10.5% bile acid retention, suggesting a mild bile acid malabsorption (BAM); for this reason, a therapy with cholestyramine, one sachet a day was prescribed, but the patient refused this drug because she was satisfied of the clinical improvement obtained with Gelsectan. She referred that this clinical improvement, mainly reduction of daily bowel movements and improvement of fecal consistency, abdominal pain, bloating and flatulence, started at the end of the second week of therapy with Gelsectan.
After further three months (T3), the patient reported she continued the treatment with Gelsectan for 8 weeks after T2 and then the therapy was stopped. In comparison with T2, no relevant changes of BSC, daily bowel movements, abdominal pain, fecal urgency, IBS-SSS, and SF 36 scores, were observed, but moderate abdominal bloating and flatulence with an occasional mild abdominal pain (Figures 1–3).
The patient was suggested to repeat a SeHCAT test to evaluate possible changes, but she refused to undergo the test.
Improvement of Gastrointestinal Symptoms and Intestinal Permeability in a 42-Year-Old Man with IBS-D
A 42-year-old man was referred in June 2019 to our outpatient clinic (Internal Medicine, University of Bari, Italy) due to chronic abdominal pain and diarrhoea. His past medical history was unremarkable until last five years, when he first suffered from recurrent abdominal pain, daily mucus loose stools (up to 5 times daily), and bloating. He also reported fatigue and loss of appetite, without a weight loss. During the past 2 years, these gastrointestinal symptoms worsened, with severe abdominal pain and fecal urgency, mainly in the immediate postprandial period. The patient never smoked or reported alcohol consumption. He reported a case of colon cancer in his family (father), without a family history of inflammatory bowel disease or celiac disease.
In the past, he underwent lactulose (LA), glucose and lactose Breath Tests. A lactose intolerance was diagnosed and treated with free lactose diet and low-FODMAP diet, with a poor improvement of the symptoms. He also assumed loperamide and antispasmodics, with low clinical benefit. The patient noted that symptoms were alternating in severity (periods of improvement and worsening), but recently, they occurred more frequently, with growing severity. Symptoms worsened, in particular, in the last two years, and this was attributed to an increased professional stress. The patient also developed anxiety, depression, and decreased intimacy. The patient denied abdominal surgery, acute enteric infection, exposure to drugs, and trips before the onset of the symptoms.
At the physical examination, the body mass index was 22.8 kg/m2, and the vital signs were within the normal range (blood pressure 110/60 mm Hg, pulse 66 beats per minute, respiratory rate 14 breaths/minute). The physical examination showed a moderate lower abdominal tenderness, without peritoneal signs. The initial workup included laboratory tests (ie, full blood count, C-reactive protein, erythrocyte sedimentation rate, celiac serology, fecal calprotectin). All findings were normal, except a slight increase in fecal calprotectin (87 μg/g, normal range 50–60 μg/g). A colonoscopy with random biopsies throughout the colon was negative. In absence of other possible organic diseases, a diagnosis of IBS-D was therefore formulated.
The intensity of symptoms (abdominal pain and bloating) was assessed by a VAS (expressed in mm and ranging from 0 to 100). The IBS-SSS was used to evaluate the severity of IBS (ie, score < 75: remission; 75–175 = mild, 175–300 = moderate, > 300 = severe score).26 Bowel movements were assessed through the BSFS. We also assessed the colonic permeability through the oral administration of the sucralose (SA), a sugar characterized by a selective absorption in the colon tract.35,36 QoL was evaluated according to the IBS-QoL questionnaire, with scores ranging from 0 to 100.37
At baseline, the patient showed a severe IBS-D, an impaired colonic permeability and a low QoL (Table 1).
 |
Table 1 Changes After 30 Days of Treatment with GELSECTAN® in Symptoms, Bowel Habits, IBS-SSS, and QoL, Intestinal Permeability |
Patient was treated with Gelsectan for 30 days, the dose consisted of two capsules twice daily before meals. Patient continued to follow the free lactose and low FODMAPs diet. During the treatment, no adverse events were reported. Symptoms and IBS-SSS, bowel movements, intestinal permeability and QoL was re-evaluated after treatment.
Respect of baseline, at the end of the treatment abdominal pain, bloating and IBS-QoL total score improved, as well as a decrease from 355 to 100 of the IBS-SSS score, showing the same reduction according to individual domains of dissatisfaction with bowel habits, interference with QoL, and number of days in the last 10 days with pain, were observed (Table 1). Furthermore, the BSFS also decreased, and the rate of SA recovery (%) drastically improved after the treatment (Table 1).
Efficacy of a Long-Term Therapy (~6 Months) with Gelsectan in a Woman with Crampy Abdominal Pain Followed by Bowel Movement
A female 46 years old patient referred to a gastroenterologist complaining crampy abdominal pain followed by bowel movement. The symptoms started when she was young, but recently increased in frequency, reaching about 8–9 times per day in the “bad days”. During the time, the patient consulted her general practitioner who prescribed some blood tests, which were normal except for the thyroid function. As a consequence, a hypothyroidism was diagnosed and a replacement therapy with levothyroxine was started, with a regular endocrinologic follow-up. She also referred a diagnosis of reflux disease, treated with on demand proton pump inhibitors, and a previous gastritis due to Helicobacter pylori, successfully eradicated.
Her physician said that the recent worsening of symptoms was probably due to the recent life changes (she had started a new job) and prescribed a treatment with antispasmodic drugs and probiotics. Due the persistence of symptoms, physician finally referred the patient to the gastroenterologist.
During the visit, the patient gave to the gastroenterologist these further information: the evacuation usually starts with normal stool that became more liquid during the evacuating session; she never observed blood during the evacuation; sometimes she feels urgency associated to the need of evacuating; usually, symptoms worsen after lunch or dinner but sometimes the need to evacuate arises immediately after waking up; she gained weight during the years; she is always tired and has problems in concentrating. Familiar history was positive for Crohn’s disease (a cousin) and colon cancer (her father).
At the physical examination, an abdominal distension due to meteorism and abdominal pain at deep palpation was detected. The workup included the following laboratory tests: blood analysis to rule out celiac disease and to evaluate a possible anemia; fecal tests including calprotectin, fecal occult blood and fecal parasite test for Giardia intestinalis antigen research. The patient was also asked to keep a diary to annotate foods and situations which could trigger the symptoms. Blood analysis showed a normal hemocromocitometric test, normal iron tests and negative anti-transglutaminase antibodies. Parasitologic test were negative also for Giardia intestinalis antigens; the value of the fecal calprotectin was slightly elevated and one out of three fecal occult blood tests was positive.
Due to her familiar history of inflammatory bowel disease and abnormal fecal tests, a small bowel ultrasound and an ileo-colonoscopy were prescribed. The small bowel ultrasound showed no significant increases in intestinal wall thickness; the terminal ileus and colon walls showed normal thickness with stratified echo structure. No significant dilation or liquid stagnation at the level of the ileal and jejunal loops were observed, as well as no mesentery hypertrophy, lymphadenomegaly or intra-abdominal effusion. The ileo-colonoscopy was performed in adequate bowel preparation conditions and the distal ileum was also observed. The ileal and colonic mucosa was normal and small internal hemorrhoids were observed. The histologic analysis of biopsies of all the explored districts, performed in order to rule out inflammatory bowel disease and microscopic colitis, showed only a mild aspecific inflammation, without alterations of the colon architecture. Finally, the diary showed that the symptoms were no triggered by foods or situations.
Due to the characteristics of the symptoms and the negative results of all the tests, a diagnosis of IBS was formulated. Since the patient did not respond to a previous treatment with antispasmodic drugs and probiotics, a therapy with rifaximin was prescribed; a follow-up visit was scheduled after 3 months.
During this follow-up visit, the clinical status of the patient improved, with a reduction of bowel movements to 4–5 per day and some urgency; however, the painful distension of the belly was already present. At the physical examination, the abdomen was less bloated than the previous visit, but the patient still felt discomfort at palpation. A treatment with Gelsectan, starting with a loading dose of 2 capsules twice a day, before breakfast and dinner, for two weeks and then a maintenance dose of 1 capsule twice a day for 2 months, was started; a new follow-up visit was scheduled after 3 months in order to re-evaluate the treatment.
After three months, the patient said that she experienced a clear improvement of the symptoms after the first two weeks of treatment and that the situation furtherly improved during the following months. The first symptom to disappear was the need to urgency to evacuate; in the following weeks, she noticed a reduction of bowel movements and a reduction of bloating and abdominal pain. At physical examination, the abdomen was still bloated but with less discomfort at palpation.
The patient was instructed to continue the treatment at the same dosage for the next two months and then to reduce the dosage to 1 capsule per day (before breakfast). At follow-up re-evaluation, approximately 6 months after the start of the treatment with Gelsectan, the patient was fine and more vigorous; abdominal pain, distension and bloating of the abdomen completely disappeared. She also said that, after some months of well-being, she stopped the treatment with Gelsectan, but after some days, she observed a slight relapse of symptoms: for this reason, she is again on treatment (1 capsule per day).
Efficacy and Safety of Gelsectan in an Elderly Woman with IBS
An 81-year-old female was referred for a gastroenterology consult at our IBD Unit. The patient was followed up in the Rheumatology Unit for a previous diagnosis of rheumatoid arthritis and osteoporosis, well controlled from a therapeutic point of view. She had also a gastro-esophageal reflux disease, chronically treated with pantoprazole 20 mg once daily.
The patient had no gastrointestinal symptoms until 1 year ago when she developed abdominal pain and diarrhoea (an average of 4–6 daily bowel movements). These gastrointestinal symptoms, including bloating and frequent watery non-bloody stools, were persistent and progressively worsening.
Her general practitioner prescribed stool cultures and laboratory tests, including serologic tests for celiac disease and hyperthyroidism, which resulted completely normal; a lactose breath test was also negative. Only fecal calprotectin was borderline (186 μg/g). Thus, the patient underwent an ileocolonoscopy for excluding a macroscopic colitis. However, biopsies were not performed, so it was not possible to exclude a microscopic colitis. Due to the fact that the patient continued to experiencing pain and diarrhoea, a computed tomography scan was performed in order to evaluate abdominal and pelvic regions; again, the findings were normal. Finally, a therapy with rifaximin 200 mg twice daily for 2 weeks followed by a probiotics therapy was performed without a satisfactory relief on symptoms.
The patient was referred to our Unit three months later. During the first visit, the patient said that no first-degree family members had celiac disease or IBD. The patient’s weight remained stable (70 kilograms) and she had no other medical issues. The physical abdominal examination was normal except a mild tenderness in the area over the ascending and the sigmoid colon. Stool cultures and blood samples (negative C-reactive protein), as well as a lactulose breath test, was carried out with negative results; the fecal calprotectin test confirmed a borderline result (125 μg/g). It was not possible to stop treatment with pantoprazole due to reflux related symptoms. Thus, an ileo-colonoscopy with biopsies throughout the terminal ileum and the colon were performed and, finally, a microscopic colitis was also excluded. Consequently, IBS-D was diagnosed according to the Rome IV criteria.
A treatment with Gelsectan was prescribed according the following schedule: 2 capsules twice daily (before breakfast and dinner) for 4 weeks, then 1 capsule twice daily for other 2 weeks. The patient reported a complete resolution of the diarrhoea just after 3 weeks (Figure 4), while abdominal pain disappeared after 6 weeks (Figure 5); a mild bloating persisted after the end of the treatment. The patient was very satisfied with the treatment: therefore, we suggested her the possibility to repeat a similar course of treatment in case of relapsing symptoms.
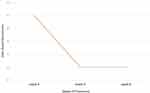 |
Figure 4 Diarrhoea following treatment with GELSECTAN®. |
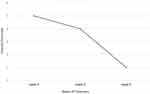 |
Figure 5 Abdominal pain following treatment with GELSECTAN®. VAS scale from 0 to 10 (0 = No pain and 10 = Worst pain). |
Recently, the patient referred again to our unit and confirmed a good control of symptoms. She performed another cycle of treatment with Gelsectan one month earlier.
Discussion
Gelsectan was evaluated in a recent double-blind study in which 60 patients were randomly assigned to receive XG + PPT + XOS or placebo for 28 days, then crossed over to the alternative treatment, and followed for a further 60 days. The patients enrolled were aged 18–65 years with a confirmed diagnosis of IBS-D according to the Rome III criteria, because at the time the study was designed the Rome IV guidelines were not yet available.21 Our publication aims to explore some issues not considered in the previous study by discussing 4 case reports of IBS-D patients, in accordance with the Rome IV criteria, treated with Gelsectan.
In the first case report, the patient, even if reporting typical IBS symptoms, deserved further investigations mainly due to advanced age, the worsening of her usual IBS symptoms and the weight loss. The outcome of a positive SeHCAT test, together with the symptoms reported by the patient, would have enabled us to prescribe a Bile Acid Sequestrant (BAS) such as cholestyramine, even if the sudden impairment of her IBS-D symptoms together with the increase of fecal calprotectin, shortly returned to almost normal levels, could support the hypothesis that an acute and transient viral enteritis could be responsible for the worsening of the clinical conditions. In this case, BAM could have been due to the changes of permeability induced by the inflammation. However, symptoms greatly improved after the administration of Gelsectan, not only compared to T0 but also compared to symptoms reported before T0, and the fecal calprotectin levels almost normalized. An acute intestinal infection can lead to an increase in calprotectin levels, as well as to an impairment of the ileal reabsorption of bile acids. A spontaneous resolution caused by an improvement of the inflammation after a viral clearance cannot be ruled out, but it is to highlight the fact that, after the use of this medical device, the patient referred an improvement of the symptoms even compared to her usual IBS condition. It is very likely that Gelsectan created a barrier that protected the intestinal mucosa from the irritating action of bile acids, with a quick improvement of the symptoms. Moreover, thanks to its restoring activity of the intestinal permeability, Gelsectan prevented the patient from undergoing prolonged BAS therapy, which was not easy to follow due to the poor palatability, the possible malabsorption of lipids and liposoluble vitamins, and interference with the absorption of other drugs. To our knowledge, this is the first case that reported a BAM improvement after Gelsectan. It would be unrealistic to draw hasty conclusions, but we think that this device, due to its components, could be useful in patients with mild/moderate BAM, frequently reported as a cause of IBS-D and functional diarrhoea.38
The efficacy of Gelsectan in restoring intestinal permeability was confirmed by the second case report, in which the patient, at baseline, showed a severe IBS-D, a low QoL, and an impaired colonic permeability detected by oral administration of the SA. In IBS-D, the expression of transmembrane and intracellular proteins decreases, damaging the integrity of the epithelial barrier and increasing intestinal permeability.39,40 In previous studies, patients with the IBS-D showed an impaired expression of E-cadherin, the core component of epithelial adherens junctions, in the colonic mucosa.41,42 The epithelial barrier defects might be associated with diarrhoea and with more severe symptoms, triggering a lot of immune events and inflammatory reactions in the gut mucosa.41 It is known that several stimuli might affect permeation processes within the gut, including dietary habits, inflammatory mediators and psychological stress.43,44 In this clinical case, patient reported fluctuating phases of disease, with more pronounced symptoms in the last year in parallel with stress period (Figure 6).
In addition to a different course of the disease, IBS is characterized by different symptoms that may respond in a different manner to the treatment with Gelsectan. In the third patient above, the urgency and the number of evacuations were the first symptoms to disappear, followed by bloating and distension. Abdominal pain and systemic symptoms only improved after a long-term treatment. A personalized treatment based on the patient’s response to Gelsectan may be useful, adjusting the dosage of the medical device according to the patients’ symptoms. In our patient, it was decided to prolong the treatment at the dosage of one capsule daily in order to achieve the complete remission of the symptoms.
Furthermore, there is a lack of evidence about the role of Gelsectan in elderly patients and the impact of concomitant medications or comorbidities on these patients. These conditions could often lead to a limitation in the enrollment of elderly patients in clinical trials. The last case report described an 81-year-old patient with a challenging diagnosis of IBS-D. Our first hypothesis of microscopic colitis, caused by pantoprazole, was not confirmed: for this reason, we assumed that the higher value of fecal calprotectin was a false positive. Symptoms significantly and rapidly improved after treatment and no complications or side effects were reported during the observation. This observation, coming from the daily clinical practice, could highlight the efficacy and safety of this new medical device, also in elderly patients.
Hence our paper, despite being a case series, aims to propose further therapeutic insights to be explored in future clinical trials, such as the use of Gelsectan in the long term, in elderly patients, and in those with mild/moderate BAM, frequently reported as a cause of IBS-D and functional diarrhoea.
Conclusion
The management of patients with IBS-D represents a great challenge for physicians: in fact, this disease has a significant impact on the patients’ QoL and it is frequently associated to a heavy socio-economic burden; besides, no standard treatment protocols are available and the treatment is usually focused on symptoms even if in most patients a clinical remission is not reached. Non-pharmacological devices with proven protective barrier properties (film-forming mucosal protectors) have been recently suggested for the management of the changes of intestinal permeability and intestinal microbiota.
In particular, Gelsectan is a medical device that acts both by forming a protective mechanical barrier on the intestinal mucosa and exerting a bifidogenic effect in the colon. Thanks to this dual mechanism of action, Gelsectan restores the epithelial barrier function and integrity and a natural-occurring microbiota.
Literature data, as well as the above presented case reports, show that agents with film-forming protective properties together with prebiotics, such as Gelsectan, represent a novel, effective and safe therapeutic option for the management of IBS-D patients.
Abbreviations
BAM, bile acid malabsorption; BAS, bile acid sequestrants; BSFS, Bristol Stool Form Scale; IBS, irritable bowel syndrome; IBS-C, irritable bowel syndrome with predominant constipation; IBS-D, irritable bowel syndrome with predominant diarrhoea; IBS-M, irritable bowel syndrome with mixed stool pattern; IBS-QoL, irritable bowel syndrome quality of life; IBS-SSS, irritable bowel syndrome symptom severity score; IBS-U, irritable bowel syndrome unclassified; LA, lactulose; PPT, tannins; QoL, quality of life; SeHCAT, 75-selenium homocholic acid taurine; SF-36, 36-item Short Form Health Survey; SA, sucralose; TJs, Tight junctions; VAS, Visual Analogue Scale; XG, xyloglucan; XOS, xylo-oligosaccharides.
Ethics Approval
This study was approved by the respective institutional research ethics committees, and was conducted in accordance with the Declaration of Helsinki.
Funding
Norgine Italia has provided support for the publication fees of case reports of patients with IBS-D treated with GELSECTAN®. Norgine Italia did not condition the writing of the article or provide grant to the authors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Mearin F, Lacy BE, Chang L, et al. Bowel disorders. Gastroenterology. 2016;18:
2. Soncini M, Stasi C, Usai Satta P, et al.; AIGO. IBS clinical management in Italy: the AIGO survey. Dig Liver Dis. 2019;51(6):782–789. doi:10.1016/j.dld.2018.10.006
3. Sperber AD, Bangdiwala SI, Drossman DA, et al. Worldwide prevalence and burden of functional gastrointestinal disorders, results of Rome Foundation Global Study. Gastroenterology. 2021;160(1):99–114.e3. doi:10.1053/j.gastro.2020.04.014
4. Camilleri M. Peripheral mechanisms in irritable bowel syndrome. N Engl J Med. 2012;367(17):1626–1635. doi:10.1056/NEJMra1207068
5. Mumolo MG, Rettura F, Melissari S, et al. Is gluten the only culprit for non-celiac gluten/wheat sensitivity? Nutrients. 2020;12(12):3785. doi:10.3390/nu12123785
6. Blake MR, Raker JM, Whelan K. Validity and reliability of the Bristol stool form scale in healthy adults and patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther. 2016;44(7):693–703. doi:10.1111/apt.13746
7. Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997;32(9):920–924. doi:10.3109/00365529709011203
8. Portincasa P, Moschetta A, Baldassarre G, et al. Pan-enteric dysmotility, impaired quality of life and alexithymia in a large group of patients meeting ROME II criteria for irritable bowel syndrome. World J Gastroenterol. 2003;9(10):2293–2299. doi:10.3748/wjg.v9.i10.2293
9. Sandler RS, Everhart JE, Donowitz M, et al. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122(5):1500–1511. doi:10.1053/gast.2002.32978
10. Bellini M, Gambaccini D, Stasi C, et al. Irritable bowel syndrome: a disease still searching for pathogenesis, diagnosis and therapy. World J Gastroenterol. 2014;20(27):8807–8820. doi:10.3748/wjg.v20.i27.8807
11. Bellini M, Rossi A. Is a low FODMAP diet dangerous? Tech Coloproctol. 2018;22(8):569–571. doi:10.1007/s10151-018-1835-9
12. Lucak S, Chang L, Halpert A, et al. Current and emergent pharmacologic treatments for irritable bowel syndrome with diarrhea: evidence-based treatment in practice. Therap Adv Gastroenterol. 2017;10(2):253–275. doi:10.1177/1756283X16663396
13. Ford AC, Sperber AD, Corsetti M, et al. Irritable bowel syndrome. Lancet. 2020;396(10263):1675–1688. doi:10.1016/S0140-6736(20)31548-8
14. Vicario M, González-Castro AM, Martínez C, et al. Increased humoral immunity in the jejunum of diarrhoea-predominant irritable bowel syndrome associated with clinical manifestations. Gut. 2015;64(9):1379–1388. doi:10.1136/gutjnl-2013-306236
15. Piqué N, Gómez-Guillén MDC, Montero MP. Xyloglucan, a plant polymer with barrier protective properties over the mucous membranes: an overview. Int J Mol Sci. 2018;19(3):673. doi:10.3390/ijms19030673
16. Oshima T, Miwa H. Gastrointestinal mucosal barrier function and diseases. J Gastroenterol. 2016;51(8):768–778. doi:10.1007/s00535-016-1207-z
17. Allegrini A, Pavone D, Carluccio F. A randomized controlled trial comparing a xyloglucan-based nasal spray with saline in adults with symptoms of rhinosinusitis. Curr Med Res Opin. 2018;34(3):377–385. doi:10.1080/03007995.2017.1341402
18. Gnessi L, Bacarea V, Marusteri M, et al. Xyloglucan for the treatment of acute diarrhea: results of a randomized, controlled, open-label, parallel group, multicentre, national clinical trial. BMC Gastroenterol. 2015;15(1):153. doi:10.1186/s12876-015-0386-z
19. Rolando M, Valente C. Establishing the tolerability and performance of tamarind seed polysaccharide (TSP) in treating dry eye syndrome: results of a clinical study. BMC Ophthalmol. 2007;7:5. doi:10.1186/1471-2415-7-5
20. Eutamene H, Beaufrand C, Harkat C, et al. The role of mucoprotectants in the management of gastrointestinal disorders. Expert Rev Gastroenterol Hepatol. 2018;12(1):83–90. doi:10.1080/17474124.2018.1378573
21. Trifan A, Burta O, Tiuca N, et al. Efficacy and safety of gelsectan for diarrhoea-predominant irritable bowel syndrome: a randomised, crossover clinical trial. United European Gastroenterol J. 2019;7(8):1093–1101. doi:10.1177/2050640619862721
22. Urakawa H, Mimura M, Kajiwara K. Diversity and versatility of plant seed xyloglucan. Trends Glycosci Glycotechnol. 2002;14(80):355–376. doi:10.4052/tigg.14.355
23. Kulkarni AD, Joshi AA, Patil CL, et al. Xyloglucan: a functional biomacromolecule for drug delivery applications. Int J Biol Macromol. 2017;104(Pt A):799–812. doi:10.1016/j.ijbiomac.2017.06.088
24. Santos J, Musta V, Luca CM, et al. Randomized, placebo-controlled trial of xyloglucan and gelose for the treatment of acute diarrhea in children. Expert Rev Gastroenterol Hepatol. 2021;15(3):325–331. doi:10.1080/17474124.2021.1833715
25. Serrano J, Puupponen-Pimiä R, Dauer A, et al. Tannins: current knowledge of food sources, intake, bioavailability and biological effects. Mol Nutr Food Res. 2009;53(Suppl S2):S310–S329. doi:10.1002/mnfr.200900039
26. Carlson JL, Erickson JM, Hess JM, et al. Prebiotic dietary fiber and gut health: comparing the in vitro fermentations of beta-glucan, inulin and xylooligosaccharide. Nutrients. 2017;9(12):1361. doi:10.3390/nu9121361
27. Eutamene H, Placide F, Tondereau V, et al. Tu1254 - protective effect of mucoprotectants and prebiotic combination on gut barrier impairment and visceral hypersensitivity induced by an acute stress in rat. Gastroenterology. 2018;154(6):S–916. doi:10.1016/S0016-5085(18)33080-4
28. Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther. 1997;11(2):395–402. doi:10.1046/j.1365-2036.1997.142318000.x
29. Gaskell SK, Snipe RMJ, Costa RJS. Test-retest reliability of a modified visual analog scale assessment tool for determining incidence and severity of gastrointestinal symptoms in response to exercise stress. Int J Sport Nutr Exerc Metab. 2019;29(4):411–419. doi:10.1123/ijsnem.2018-0215
30. Apolone G, Mosconi P. The Italian SF-36 health survey: translation, validation and norming. J Clin Epidemiol. 1998;51(11):1025–1036. doi:10.1016/s0895-4356(98)00094-8
31. Ware JE
32. Hays RD, Sherbourne CD, Mazel RM. The RAND 36-item health survey 1.0. Health Econ. 1993;2(3):217–227. doi:10.1002/hec.4730020305
33. Brazier JE, Harper R, Jones NM, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305(6846):160–164. doi:10.1136/bmj.305.6846.160
34. Fani B, Bertani L, Paglianiti I, et al. Pros and cons of the SeHCAT test in bile acid diarrhea: a more appropriate use of an old nuclear medicine technique. Gastroenterol Res Pract. 2018;2018:2097359. doi:10.1155/2018/2097359
35. Del Valle-Pinero AY, Van Deventer HE, Fourie NH, et al. Gastrointestinal permeability in patients with irritable bowel syndrome assessed using a four probe permeability solution. Clin Chim Acta. 2013;418:97–101. doi:10.1016/j.cca.2012.12.032
36. Bonfrate L, Di Palo DM, Celano G, et al. Effects of Bifidobacterium longum BB536 and Lactobacillus rhamnosus HN001 in IBS patients. Eur J Clin Invest. 2020;50(3):e13201. doi:10.1111/eci.13201
37. Andrae DA, Patrick DL, Drossman DA, et al. Evaluation of the Irritable Bowel Syndrome Quality of Life (IBS-QOL) questionnaire in diarrheal-predominant irritable bowel syndrome patients. Health Qual Life Outcomes. 2013;11:208. doi:10.1186/1477-7525-11-208
38. Valentin N, Camilleri M, Altayar O, et al. Biomarkers for bile acid diarrhoea in functional bowel disorder with diarrhoea: a systematic review and meta-analysis. Gut. 2016;65(12):1951–1959. doi:10.1136/gutjnl-2015-309889
39. Coëffier M, Gloro R, Boukhettala N, et al. Increased proteasome-mediated degradation of occludin in irritable bowel syndrome. Am J Gastroenterol. 2010;105(5):1181–1188. doi:10.1038/ajg.2009.700
40. Bertrand J, Ghouzali I, Guérin C, et al. Glutamine restores tight junction protein claudin-1 expression in colonic mucosa of patients with diarrhea-predominant irritable bowel syndrome. JPEN J Parenter Enteral Nutr. 2016;40(8):1170–1176. doi:10.1177/0148607115587330
41. Piche T. Tight junctions and IBS–the link between epithelial permeability, low-grade inflammation, and symptom generation? Neurogastroenterol Motil. 2014;26(3):296–302. doi:10.1111/nmo.12315
42. Piche T, Barbara G, Aubert P, et al. Impaired intestinal barrier integrity in the colon of patients with irritable bowel syndrome: involvement of soluble mediators. Gut. 2009;58(2):196–201. doi:10.1136/gut.2007.140806
43. Arrieta MC, Bistritz L, Meddings JB. Alterations in intestinal permeability. Gut. 2006;55(10):1512–1520. doi:10.1136/gut.2005.085373
44. Ferrier L. Significance of increased human colonic permeability in response to corticotrophin-releasing hormone (CRH). Gut. 2008;57(1):7–9. doi:10.1136/gut.2007.129841
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.