Back to Journals » Blood and Lymphatic Cancer: Targets and Therapy » Volume 7
Use of carfilzomib in second-line therapy and beyond for relapsed multiple myeloma
Received 8 August 2016
Accepted for publication 1 February 2017
Published 19 July 2017 Volume 2017:7 Pages 53—60
DOI https://doi.org/10.2147/BLCTT.S82444
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor David Dingli
Divaya Bhutani, Jeffrey A Zonder
Department of Oncology, Karmanos Cancer Institute, Wayne State University, Detroit, MI, USA
Abstract: The development of proteasome inhibitors has been a major advance in therapy of multiple myeloma, accounting, in part, for the significant increase in the survival of patients diagnosed with this disease. Bortezomib was the first proteasome inhibitor to be approved for the therapy of multiple myeloma. Carfilzomib is a second-generation proteasome inhibitor with irreversible binding to proteasome and less off-target toxicity. The drug has been approved for use in relapsed/refractory multiple myeloma. In this article, we review the use of carfilzomib as second-line therapy in multiple myeloma. We also review the current standards of care for relapsed/refractory multiple myeloma, with particular focus on the use of carfilzomib in advanced disease.
Keywords: multiple myeloma, carfilzomib, relapsed/refractory
Introduction to the management of relapsed and refractory multiple myeloma
Over the past two decades, improvements in therapy have led to improved outcomes for people with multiple myeloma. According to the SEER database, the percentage of newly diagnosed patients surviving beyond 5 years from diagnosis increased from 30% in 1999 to 48.5% in 2012.1 The major reason for this development has been discovery and widespread implementation of novel agents, namely proteasome inhibitors and immunomodulatory drugs, during that period. Novel therapeutic combinations incorporating these newer drugs have yielded impressive results, with overall response rates approaching in excess of 80%–90% and rates of complete remission (CR) approaching as high as 40%–50%.2–5 Despite these improvements in frontline therapy, multiple myeloma remains incurable and relapse after frontline therapy remains the norm in the majority of the patients.
The treatment of relapsed and refractory myeloma, thus, remains a very large and important part of management of patients with this disease.6 Most patients require multiple lines of therapy during their disease course. In this review, after briefly outlining the current and emerging therapeutic options for patients with relapsed and/or refractory multiple myeloma, we will specifically focus on the use of carfilzomib as second-line therapy.
Overview of current treatment approaches
Drug combinations available for use in relapsed or refractory multiple myeloma
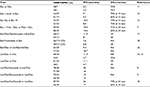
Multiple drugs are approved for use in this patient population either as single agents or in combination, including melphalan, cyclophosphamide, thalidomide, lenalidomide, pomalidomide, bortezomib, carfilzomib, ixazomib, liposomal doxorubicin, panobinostat, elotuzumab, and daratumumab. Pivotal randomized trials establishing the use of many of these agents are detailed in Table 1. Table 2 provides a list of noteworthy Phase 1 and Phase 2 trials that incorporate one or more of these agents. One important observation from these trials is that with newer drug combinations, the response rates are quite high even in relapsed/refractory setting. Although differences in inclusion/exclusion criteria and the resultant variability in the patient populations make it impossible to directly compare the results of specific trials, it is evident that several regimens induce responses in ≥70% of treated patients. Furthermore, the quality of responses (as assessed by the frequency of achieving at least a very good partial response [VGPR]) is improving. As an example, the likelihood of achieving at least a VGPR with recent triplet regimens7,8–10 is 2–3 times higher than with single-agent bortezomib,11–13 and 10 times higher than with dexamethasone alone.14,15 Finally, disease control may be prolonged, particularly as some of the noted regimens incorporate ongoing maintenance therapy.9,10,16
Two-drug vs three-drug regimens
As various combination regimens have been developed for the treatment of patients with relapsed/refractory multiple myeloma, optimal use of the specific drugs has become a subject of controversy. A perusal of Tables 1 and 2 shows that both two-drug (doublet) and three-drug (triplet) regimens are superior to single-agent therapy in this setting. Furthermore, most of the included trials comparing triplets to doublets demonstrate overall superiority of three-drug combinations in terms of initial response rate and duration of response. But the question of survival benefit remains a difficult one given that all these drugs would be available to the patients at the time of progression and the clinical trials are not designed to compare sequential treatments. In addition, the data for overall survival (OS) are not completely mature in many of the randomized trials comparing three- vs two-drug combinations.7,8–10,17,18 Thus, it is unclear at this time whether three-drug regimens would lead to superior survival as long as patients eventually have access to all available therapies. Another relevant consideration is the potential for increased toxicity as additional drugs are added to a regimen. Tables like the ones herein rarely provide insight with regards to this aspect of therapy selection, instead focusing on efficacy end points. Particularly in older and/or frail patients, the toxicity profile of specific combinations should be carefully considered and balanced against the incremental improvement in expected immediate disease control.
Role of second autologous stem cell transplant
Autologous stem cell transplantation is often used as part of up-front therapy in younger patients and has been shown to improve both progression-free survival (PFS) and OS in multiple randomized trials.19,20 Although there have been no randomized trials comparing a second autologous stem cell transplantation to nontransplant therapy in relapsed/refractory scenario, it is sometimes offered to sufficiently fit patients. Center for International Blood and Marrow Transplant Research reported outcomes of 187 patients who underwent second autologous stem cell transplantation for relapsed myeloma, analyzed retrospectively.21 The overall response rate was 68% (with 25% of the patients achieving a CR), the median PFS was 11.2 months with a median OS of 30 months. Overall, the therapy was well tolerated with a nonrelapse mortality of 2% during the first year after second autologous stem cell transplant. Similar outcomes have been reported by other groups.22,23 In summary, for eligible patients, a second autologous stem cell transplant is an effective and safe therapy and comparable with other available therapies in this situation.
Pharmacology of carfilzomib and other proteasome inhibitors
Proteasome inhibitors have become one of the most widely used classes of drugs in the therapy of multiple myeloma. Bortezomib was the first proteasome inhibitor to be approved for this disease, first in relapsed disease and subsequently for up-front therapy. The proteasome is an enzymatic complex required for intracellular degradation of proteins in all human cells.24,25 The functional unit named 26S proteasome complex is made of a 20S core catalytic complex that is capped at each end by a 19S regulatory subunit. There are three catalytic sites within the 20S core: β1 (caspase-like), β2 (trypsin-like), and β5 (chymotrypsin-like). The proteasome is responsible for degradation of multiple cellular proteins including some proteins essential to the cell cycle, such as cyclins A, B, D, E, and cyclin-dependent kinase inhibitor,26 tumor suppressor proteins such as p5327 and also I-kB, which is an inhibitor of NF-kappa pathway in plasma cells.28 Dysregulation of such pathways via proteasome inhibition leads to cell apoptosis.24
Bortezomib is a boron-containing proteasome inhibitor25 that binds predominantly to the chymotrypsin-like site of the 20S proteasome, causing inhibition of its function. The binding is reversible and dose dependent.29 Carfilzomib is derived from ketoepoxide compounds that are potent inhibitors of the proteasome, as well.30 Carfilzomib also binds to the β5 chymotrypsin-like subunit, but more specifically with regards to the other catalytic subunits compared with bortezomib. Also, the binding is irreversible.31 It is postulated that this subunit specificity may account for a lower incidence of certain side effects with carfilzomib, namely peripheral neuropathy. In preclincial studies,31,32 carfilzomib inhibited proliferation and activated apoptosis in myeloma cell lines more potently than bortezomib and displayed activity against bortezomib-resistant myeloma cell lines and samples derived from patients with bortezomib-resistant myeloma.32 In addition, Kuhn et al32 showed that in preclinical models, carfilzomib caused preferential inhibition of chymotrypsin-like activity β5 subunit of proteasome at concentration as low as 10 nM and had no effect on the trypsin-like activity of the β2 subunit at concentrations as high as 100 nM.
In terms of pharmacokinetics after intravenous (IV) administration, carfilzomib is rapidly cleared from plasma, with the majority of drug eliminated from plasma within 30 minutes of administration.33,34 The drug is highly protein bound in the plasma. The rapid clearance of carfilzomib is primarily mediated by metabolism instead of renal excretion. The majority of the drug is metabolized and converted into inactive metabolites by extra hepatic metabolism.34 The p-450 system plays only a minor role in metabolism of the drug. The excretion of the drug is mainly in the form of inactive metabolites.
The pharmacokinetics and safety of carfilzomib is similar in patients with poor renal function as compared to patients with normal renal function.35 Thus, the drug can be safely used in patients with impaired renal function without dose reduction. Currently, carfilzomib is approved as a twice-weekly IV infusion on days 1, 2, 8, 9, 15, and 16 of a 28-day cycle (20 mg/m2 in cycle 1, week 1 and 27 or 56 mg/m2 beyond). The drug is also approved using the same administration schedule at a dose of 27 mg/m2 in combination with lenalidomide and dexamethasone.
Clinical studies in patients with relapsed multiple myeloma, with a focus on second-line use
On the basis of the excellent preclinical activity,31,32 carfilzomib was initially evaluated in two Phase 1 human studies.36,37 In the first study, the drug was administered on five consecutive days in a 14-day cycle and dose escalation proceeded from 1.2 to 20 mg/m2. Twenty-nine patients with various hematologic malignancies were enrolled in the study and the maximum tolerated dose (MTD) was established at 15 mg/m2 in this study. Dose limiting toxicities seen in the 20 mg/m2 cohort consisted of febrile neutropenia and grade 4 thrombocytopenia. Pharmacodynamic studies revealed proteasome inhibition of >75% after a single dose of carfilzomib at dose levels of 15 mg/m2 and higher. Clinical responses were seen in patients with multiple myeloma at doses >11 mg/m2. Because of anticipated logistical difficulties related to prolonged therapy with dosing on 5 consecutive days every 2 weeks, a separate Phase 1 study was done to investigate twice-weekly schedule.37
In the second Phase 1 study,37 patients with multiple myeloma and lymphoma (N=48) were enrolled and treated with escalating doses of carfilzomib from 1.2 to 27 mg/m2 with twice-weekly IV infusions on days 1, 2, 8, 9, 15, and 16 of a 28-day cycle. In this study, the MTD was not reached. Very few nonhematologic grade ≥3 adverse events (AEs) were seen. The common grade 1–2 nonhematologic AEs were gastrointestinal upset and fever. There was no documented grade 3+ peripheral neuropathy. The grade 3+ hematologic AEs observed were anemia and thrombocytopenia, each seen in ~27% of patients. Pharmacodynamic studies confirmed that doses of 15 mg/m2 resulted in >80% proteasome inhibition in whole blood with very minimal recovery of proteasome activity seen between the doses of carfilzomib. Objective responses were seen both in multiple myeloma and non-Hodgkin’s lymphoma and doses >15 mg/m2 on this dosing schedule. On the basis of this study, this dosing schedule was chosen for evaluation in further trials.
On the basis of the above data, carfilzomib was evaluated in a Phase 2 study38 of relapsed and refractory multiple myeloma patients at a dose of 20 mg/m2 in the first cycle and then increased to 27 mg/m2 in the subsequent cycles (20/27 mg/m2) along with dexamethasone 4 mg with each dose of carfilzomib. In this study, 95% of the 257 enrolled patients were refractory to their last therapy; 80% were refractory or intolerant to both bortezomib and lenalidomide. Patients had received a median of five lines of therapy prior to the study. The overall response rate in the study was 23.7% with a CR+VGPR rate of 14% and median duration of response 7.8 months in responding patients. In terms of the AEs, the most common grade ≥3 AEs were anemia and thrombocytopenia, each seen in ~25% of the patients, and also fatigue in ~8% of the patients. Dyspnea attributed to carfilzomib, usually transient, was seen in ~17% of patients. Renal dysfunction was seen in 25% of patients, with roughly two-thirds of cases felt to be related to carfilzomib therapy. Congestive heart failure was seen in 3.8% of patients. Finally, although worsening peripheral neuropathy was seen in 12.4% of patients, it was grade ≥3 in only 1.1% of patients.
Another Phase 2 study39 evaluating the use of single-agent carfilzomib in bortezomib-naive relapsed/refractory multiple myeloma patients showed somewhat better antimyeloma activity. The objective response rate (ORR) was 52% with a CR+VGPR rate of 19% in patients treated at a 20/27 mg/m2 dose (N=70). The median number of earlier therapies was two in this study. AEs were similar to those seen in previous trials, including a low incidence of severe peripheral sensory neuropathy. Thus, as had been previously demonstrated with bortezomib,6,12,13 antimyeloma efficacy of carfilzomib seems to be higher when used in less heavily treated patients.
Two Phase 3 trials using carfilzomib-containing regimens in patients with multiple myeloma who have had 1–3 prior lines of therapy have been published. The ASPIRE trial10 compared lenalidomide/dexamethasone/carfilzomib with a control arm of lenalidomide/dexamethasone. A total of 792 patients were enrolled in the study. Patients had received a median of two prior lines of therapy, including ~65% of patients who had received bortezomib in the past. Carfilzomib was given at a dose of 20/27 mg/m2 with lenalidomide 25 mg/day and dexamethasone 40 mg. The overall response rate in the experimental arm was 87% as compared to 67% in the control arm, and the likelihood of achieving a VGPR or better was 70% vs 40%. The median PFS was improved from 17 months in the control arm to 26 months in the experimental arm. Two-year OS was improved from 65% to 73% (P=0.04). Efficacy data for the 43% of enrolled patients who had had only one prior line of therapy (ie, were getting second-line therapy) was not specifically reported. Serious AEs were seen in 59% of patient in the experimental arm compared with 53% in the control arm. There was a slight excess of grade ≥3 dyspnea (2.8% vs 1.8%), renal dysfunction (3.3% vs 3.1%), congestive heart failure (3.8% vs 1.8%), ischemic heart disease (3.3% vs 2.1%), and hypertension (4.3% vs 1.8%) in the carfilzomib-containing arm.
The second Phase 3 trial, so called ENDEAVOR trial,16 compared carfilzomib (at a dose of 20 mg/m2 on days 1, 2 of cycle 1, and 56 mg/m2 subsequently) plus dexamethasone with bortezomib (1.3 mg/m2 IV or subcutaneous [SQ] on days 1, 4, 8, and 11) plus dexamethasone in 929 patients. As in the ASPIRE trial, patients had all received between 1 and 3 prior lines of therapy. The preliminary results did show improvement in ORR (63% vs 77%), as well as the rate of achieving a VGPR or better (29% vs 54%). Furthermore, PFS was longer in the carfilzomib arm (18.7 months vs 9.4 months). There was a slight excess of grade 3+ anemia and hypertension in the carfilzomib arm, but the on-therapy deaths due to AEs for each arm was similar (4% for carfilzomib/dexamethasone vs3% for bortezomib/dexamethasone).
Given these results, multiple other carfilzomib-containing combinations, including carfilzomib, pomalidomide and dexamethasone;40 carfilzomib, cyclophosphamide and dexamethasone;41 and carfilzomib plus panobinostat42 have been explored. Table 2 highlights the details of these and other carfilzomib-containing regimens in relapsed multiple myeloma. In general, carfilzomib is given at a dose of 20/27–20/36 mg/m2 when given according to a standard schedule, but the dose may be escalated if a weekly (rather than twice weekly) schedule is used. This will be discussed further in the following section.
Patient-focused perspectives, such as quality of life, patient satisfaction/acceptability, and adherence
The standard twice-weekly (for 3 out of 4 weeks each cycle) administration schedule carfilzomib can be somewhat onerous, particularly for patients receiving the drug over a long period of time. A common strategy to address this is to switch to an alternate-week schedule as “maintenance”, usually after 8–9 cycles of full-intensity therapy.43 Using this approach, carfilzomib is administered on days 1, 2, 15, and 16 of each 4-week maintenance cycle. An alternative to this has been the development of weekly carfilzomib therapy. Escalated weekly dosing has been evaluated in a large Phase 1/2 study44 in which an MTD of 70 mg/m2 given once a week was established. The efficacy of the drug did not appear to be compromised; if anything, the higher dose weekly therapy was associated with an overall response rate of 77% – higher than the response rates in previous trials using standard dose and schedule. The frequency and severity of side effects observed in this trial were similar to previous reports involving standard dosing. As such, carfilzomib 70 mg/m2 weekly is currently being compared with standard 20/27 mg/m2 dosing twice-weekly in a randomized trial. It should be noted that doses of carfilzomib of 36 mg/m2 or higher should be administered over 30 minutes, as opposed to the 2- to 10-minute infusion time used for lower doses.
The IV route of administration is an inconvenience, particularly as other approved proteasome inhibitors are administered either SQ (bortezomib) or orally (ixazomib). The oral proteasome inhibitor ixazomib has recently been approved in combination with lenalidomide plus dexamethasone for patients with relapsed multiple myeloma who have previously received one line of therapy. The pivotal Phase 3 trial, which led to the approval of ixazomib, did not include patients with bortezomib-refractory disease,8 leaving the question of the oral proteasome inhibitors efficacy in this group. Therefore, at this time, carfilzomib remains the proteasome inhibitor of choice in patients with bortezomib-refractory multiple myeloma. Efforts at developing oprozomib, an oral drug with structural similarities to carfilzomib, have met with difficulty, largely due to gastrointestinal toxicity. This has been observed in trials involving myeloma patients45 and patients with solid tumors.46
Health-related quality of life (QoL) was formally studied in the ASPIRE trial (carfilzomib, lenalidomide, dexamethasone vs lenalidomide, and dexamethasone).10 Two validated health-related QoL instruments (EORTC QLQ-C30 and QLQ MY20) were administered on day 1 of cycles 1, 3, 6, 12, 18, and at the end of the treatment. The triplet therapy group had higher QLQ-C30 Global Health Status/QoL scores compared with doublet therapy over 18 cycles of treatment (P<0.0001). In addition, there was no difference in terms of the impact of AEs on QoL between the two groups indicating no additive negative impact of triplet therapy (KRd) vs doublet therapy (Rd) in this trial.
Conclusions and future directions
Carfilzomib represents an important therapy for patients with relapsed/refractory multiple myeloma. Optimal dose and schedule is still being evaluated. It seems likely that higher doses (20/36–20/56 mg/m2 when administered twice-weekly; 70 mg/m2 when administered once-weekly) are associated with higher response rates without appreciable increases in toxicity. Combining carfilzomib with other agents is feasible and also generally improves efficacy compared with standard twice-weekly carfilzomib monotherapy. In general, inherent and acquired resistance to carfilzomib in relapsed myeloma is an issue even today. Recent work has focused on identifying and overcoming resistance mechanisms. For example, a recent trial adding the CRM-1 inhibitor selinexor to carfilzomib in patients with carfilzomib-refractory myeloma was undertaken after preclinical studies showed that selinexor may restore sensitivity to carfilzomib.47 Furthermore, the role of carfilzomib in the setting of relapsed myeloma will likely evolve if the drug becomes approved for use as part of frontline therapy.
Disclosure
Dr Zonder is a consultant for Takeda, the manufacturer of bortezomib and ixazomib. The authors report no other conflicts of interest in this work.
References
National Institute of Health Surveillance, Epidemiology, and End Results Program data. Cancer Stat Facts: Myeloma. Available from: http://seer.cancer.gov/statfacts/html/mulmy.html. Accessed June 16, 2017. | ||
Sonneveld P, Schmidt-Wolf IG, Van der Holt B. Bortezomib induction and maintenance treatment in patients with newly diagnosed multiple myeloma: results of the randomized phase III HOVON-65/GMMG-HD4 trial. J Clin Oncol. 2012;30(24):2946–2955. | ||
Rosiñol L, Oriol A, Teruel AI, et al. Superiority of bortezomib, thalidomide, and dexamethasone (VTD) as induction pretransplantation therapy in multiple myeloma: a randomized phase 3 PETHEMA/GEM study. Blood. 2012;120(8):1589–1596. | ||
Kumar S, Flinn I, Richardson PG, et al. Randomized, multicenter, phase 2 study (EVOLUTION) of combinations of bortezomib, dexamethasone, cyclophosphamide, and lenalidomide in previously untreated multiple myeloma. Blood. 2012;119(19):4375–4382. | ||
Richardson PG, Weller E, Lonial S, et al. Lenalidomide, bortezomib, and dexamethasone combination therapy in patients with newly diagnosed multiple myeloma. Blood. 2010;116(5):679–686. | ||
Nooka AK, Kastritis E, Dimopoulos MA, Lonial S. Treatment options for relapsed and refractory multiple myeloma. Blood. 2015;125(20):3085–3099. | ||
Garderet L, Iacobelli S, Moreau P, et al. Superiority of the triple combination of bortezomib-thalidomide-dexamethasone over the dual combination of thalidomide-dexamethasone in patients with multiple myeloma progressing or relapsing after autologous transplantation: the MMVAR/IFM 2005-04 Randomized Phase III Trial from the Chronic Leukemia Working Party of the European Group for blood and marrow transplantation. J Clin Oncol. 2012;30(20):2475–2482. | ||
Philippe M, Tamás M, Norbert G, et al. Ixazomib, an investigational oral proteasome inhibitor (PI), in combination with lenalidomide and dexamethasone (IRd), Significantly extends progression-free survival (PFS) for patients (Pts) with relapsed and/or refractory multiple myeloma (RRMM): the Phase 3 Tourmaline-MM1 Study. ASH Meeting 2015 Abstract 727. | ||
Lonial S, Dimopoulos M, Palumbo A, et al. Elotuzumab therapy for relapsed or refractory multiple myeloma. N Engl J Med. 2015;373:621–631. | ||
Stewart AK, Rajkumar SV, Dimopoulos MA, et al. Carfilzomib, lenalidomide, and dexamethasone for relapsed multiple myeloma. N Engl J Med. 2015;372(2):142–152. | ||
Richardson PG, Sonneveld P, Schuster MW, et al. Bortezomib or high-dose dexamethasone for relapsed multiple myeloma. N Engl J Med. 2005;352(24):2487–2498. | ||
Orlowski RZ, Nagler A, Sonneveld P, et al. Randomized phase III study of pegylated liposomal doxorubicin plus bortezomib compared with bortezomib alone in relapsed or refractory multiple myeloma: combination therapy improves time to progression. J Clin Oncol. 2007;25(25):3892–3901. | ||
Moreau P, Pylypenko H, Grosicki S, et al. Subcutaneous versus intravenous administration of bortezomib in patients with relapsed multiple myeloma: a randomised, phase 3, non-inferiority study. Lancet Oncol. 2011;12(5):431–440. | ||
Dimopoulos M, Spencer A, Attal M, et al. Lenalidomide plus dexamethasone for relapsed or refractory multiple myeloma. N Engl J Med. 2007;357(21):2123–2132. | ||
Weber DM, Chen C, Niesvizky R, et al. Lenalidomide plus dexamethasone for relapsed multiple myeloma in North America. N Engl J Med. 2007;357(21):2133–2142. | ||
Meletios A. Dimopoulos PM, Moreau P, et al. Carfilzomib and dexamethasone (Kd) vs bortezomib and dexamethasone (Vd) in patients (pts) with relapsed multiple myeloma (RMM): results from the phase III study ENDEAVOR. ASCO Meeting Abstracts 2015. J Clin Oncol. 2015;33:Abstract 8509. | ||
San-Miguel JF, Hungria VT, Yoon SS, et al. Panobinostat plus bortezomib and dexamethasone versus placebo plus bortezomib and dexamethasone in patients with relapsed or relapsed and refractory multiple myeloma: a multicentre, randomised, double-blind phase 3 trial. Lancet Oncol. 2014;15(11):1195–1206. | ||
Dimopoulos M, Siegel DS, Lonial S, et al. Vorinostat or placebo in combination with bortezomib in patients with multiple myeloma (VANTAGE 088): a multicentre, randomised, double-blind study. Lancet Oncol. 2013;14(11):1129–1140. | ||
Attal M, Harousseau JL, Stoppa AM, et al. A prospective, randomized trial of autologous bone marrow transplantation and chemotherapy in multiple myeloma. N Engl J Med. 1996;335(20:91–97. | ||
Palumbo A, Cavallo F, Gay F, et al. Autologous transplantation and maintenance therapy in multiple myeloma. N Engl J Med. 2014;371:895–905. | ||
Michaelis LC, Saad A, Zhong X, et al. Salvage second hematopoietic cell transplantation in myeloma. Biol Blood Marrow Transplant. 2013;19(5):760–766. | ||
Jimenez-Zepeda VH, Mikhael J, Winter A, et al. Second autologous stem cell transplantation as salvage therapy for multiple myeloma: impact on progression-free and overall survival. Biol Blood Marrow Transplant. 2012;18(5):773–779. | ||
Shah N, Ahmed F, Bashir Q, et al. Durable remission with salvage second autotransplants in patients with multiple myeloma. Cancer. 2012; 118(14):3549–3555. | ||
Schenkein D. Proteasome inhibitors in the treatment of B-cell malignancies. Clin Lymphoma. 2002;3(1):49–55. | ||
Adams J. The proteasome: a suitable antineoplastic target. Nat Rev Cancer. 2004;4(5):349–360. | ||
Pagano M, Tam SW, Theodoras AM, et al. Role of the ubiquitin-proteasome pathway in regulating abundance of the cyclin-dependent kinase inhibitor p27. Science. 1995;269(5224):682–685. | ||
An WG, Hwang SG, Trepel JB, Blagosklonny MV. Protease inhibitor-induced apoptosis: accumulation of wt p53, p21WAF1/CIP1, and induction of apoptosis are independent markers of proteasome inhibition. Leukemia. 2000;14(7):1276–1283. | ||
Roff M, Thompson J, Rodriguez MS, et al. Role of IkBa ubiquitination in signal-induced activation of NF-κB in vivo. J Biol Chem. 1996; 271:7844–7850. | ||
Lightcap ES, McCormack TA, Pien CS, Chau V, Adams J, Elliott PJ. Proteasome inhibition measurements: clinical application. Clin Chem. 2000;46(5):673–683. | ||
Meng L, Mohan R, Kwok BH, Elofsson M, Sin N, Crews CM. Epoxomicin, a potent and selective proteasome inhibitor, exhibits in vivo antiinflammatory activity. Proc Natl Acad Sci USA. 1999;96(18):10403–10408. | ||
Demo SD, Kirk CJ, Aujay MA, et al. Antitumor activity of PR-171, a novel irreversible inhibitor of the proteasome. Cancer Res. 2007;67(13):6383–6391. | ||
Kuhn DJ, Chen Q, Voorhees PM, et al. Potent activity of carfilzomib, a novel, irreversible inhibitor of the ubiquitin-proteasome pathway, against preclinical models of multiple myeloma. Blood. 2007;110(9):3281–3290. | ||
Wang Z, Yang J, Kirk C, et al. Clinical pharmacokinetics, metabolism, and drug-drug interaction of carfilzomib. Drug Metab Dispos. 2013;41(1):230–237. | ||
Yang J, Wang Z, Fang Y, et al. Pharmacokinetics, pharmacodynamics, metabolism, distribution, and excretion of carfilzomib in rats. Drug Metab Dispos. 2011;39(10):1873–1882. | ||
Badros AZ, Vij R, Martin T, et al. Carfilzomib in multiple myeloma patients with renal impairment: pharmacokinetics and safety. Leukemia. 2013;27(8):1707–1714. | ||
O’Connor OA, Stewart AK, Vallone M, et al. A phase 1 dose escalation study of the safety and pharmacokinetics of the novel proteasome inhibitor carfilzomib (PR-171) in patients with hematologic malignancies. Clin Cancer Res. 2009;15(22):7085–7091. | ||
Alsina M, Trudel S, Furman RR, et al. A phase I single-agent study of twice-weekly consecutive-day dosing of the proteasome inhibitor carfilzomib in patients with relapsed or refractory multiple myeloma or lymphoma. Clin Cancer Res. 2012;18(17):4830–4840. | ||
Siegel DS, Martin T, Wang M, et al. A phase 2 study of single-agent carfilzomib (PX-171-003-A1) in patients with relapsed and refractory multiple myeloma. Blood. 2012;120(14):2817–2825. | ||
Vij R, Wang M, Kaufman JL, et al. An open-label, single-arm, phase 2 (PX-171-004) study of single-agent carfilzomib in bortezomib-naive patients with relapsed and/or refractory multiple myeloma. Blood. 2012;119(24):5661–5670. | ||
Shah JJ, Stadtmauer EA, Abonour R, et al. Carfilzomib, pomalidomide, and dexamethasone for relapsed or refractory myeloma. Blood. 2015;126(20):2284–2290. | ||
Yong KL, Brown S, Hinsley S, et al. Carfilzomib, cyclophosphamide and dexamethasone is well tolerated in patients with relapsed/refractory multiple myeloma who have received one prior regimen. American Society of Hematology Annual Meeting 2015; Orlando, Florida. Abstract 1840. | ||
Berdeja JG, Hart LL, Mace JR, et al. Phase I/II study of the combination of panobinostat and carfilzomib in patients with relapsed/refractory multiple myeloma. Haematologica. 2015;100(5):670–676. | ||
Bringhen S, Petrucci MT, Larocca A, et al. Carfilzomib, cyclophosphamide, and dexamethasone in patients with newly diagnosed multiple myeloma: a multicenter, phase 2 study. Blood. 2014;124(1):63–69. | ||
Berenson J, Cartmell A, Lyons R, et al. Weekly carfilzomib with dexamethasone for patients with relapsed or refractory multiple myeloma: updated results from the phase 1/2 study champion-1. American Society of Hematology annual meeting 2015. Blood. 2015;126:373. | ||
Hari PN, Shain KH, Voorhess PM, et al. Oprozomib and dexamethasone in patients with relapsed and/or refractory multiple myeloma: initial results from the dose escalation portion of a phase 1b/2, Multicenter, Open-Label Study. American Society of Hematology annual meeting 2014; San Francisco, California. Abstract 3453. | ||
Infante JR, Mendelson DS, Burris HA, et al. A first-in-human dose-escalation study of the oral proteasome inhibitor oprozomib in patients with advanced solid tumors. Invest New Drugs. 2016;34(2):216–224. | ||
Jakubowiak A, Jasielec J, Rosenbaum CA, et al. Phase 1 MMRC trial of selinexor, carfilzomib (CFZ), and dexamethasone (DEX) in relapsed and relapsed/refractory multiple myeloma. American Society of Hematology Annual Meeting 2015; Orlando, Florida. Abstract 4223. | ||
Richardson PG, Barlogie B, Berenson J, et al. A phase 2 study of bortezomib in relapsed, refractory myeloma. N Engl J Med. 2003;348(26):2609–2617. | ||
Mikhael JR, Belch AR, Prince HM, et al. High response rate to bortezomib with or without dexamethasone in patients with relapsed or refractory multiple myeloma: results of a global phase 3b expanded access program. Br J Haematol. 2009;144(2):169–175. | ||
Reece DE, Rodriguez GP, Chen C, et al. Phase I-II trial of bortezomib plus oral cyclophosphamide and prednisone in relapsed and refractory multiple myeloma. J Clin Oncol. 2008;26(29):4777–4783. | ||
Kumar SK, Krishnan A, LaPlant B, et al. Bendamustine, lenalidomide, and dexamethasone (BRD) is highly effective with durable responses in relapsed multiple myeloma. Am J Hematol. 2015;90(12):1106–1110. | ||
Schey SA, Morgan GJ, Ramasamy K, et al. The addition of cyclophosphamide to lenalidomide and dexamethasone in multiply relapsed/refractory myeloma patients; a phase I/II study. Br J Haematol. 2010;150(3):326–333. | ||
Dimopoulos MA, Kastritis E, Christoulas D, et al. Treatment of patients with relapsed/refractory multiple myeloma with lenalidomide and dexamethasone with or without bortezomib: prospective evaluation of the impact of cytogenetic abnormalities and of previous therapies. Leukemia. 2010;24(10):1769–1778. | ||
Lentzsch S, O’Sullivan A, Kennedy RC, et al. Combination of bendamustine, lenalidomide, and dexamethasone (BLD) in patients with relapsed or refractory multiple myeloma is feasible and highly effective: results of phase 1/2 open-label, dose escalation study. Blood. 2012;119(20):4608–4613. | ||
Siegel DS, Martin T, Wang M, et al. A phase 2 study of single-agent carfilzomib (PX-171-003-A1) in patients with relapsed and refractory multiple myeloma. Blood. 2012;120(14):2817–2825. | ||
Zonder JA, Usmani S, Scott EC, et al. Phase 2 Study of carfilzomib (CFZ) with or without filanesib (FIL) in patients with advanced multiple myeloma. American Society of Hematology Annual Meeting 2015; Orlando, Florida. Abstract 728. | ||
Richardson PG, Siegel DS, Vij R, et al. Pomalidomide alone or in combination with low-dose dexamethasone in relapsed and refractory multiple myeloma: a randomized phase 2 study. Blood. 2014;123(12):1826–1832. | ||
Lokhorst HM, Plesner T, Laubach JP, et al. Targeting CD38 with daratumumab monotherapy in multiple myeloma. N Engl J Med. 2015;373(13):1207–1219. | ||
Buda G, Orciuolo E, Galimberti S, Ghio F, Petrini M. VDTPACE as salvage therapy for heavily pretreated MM patients. Blood. 2013;122:5377–5377. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.