Back to Journals » Patient Preference and Adherence » Volume 14
Use of a Patient Information Leaflet on Oro-Dental Care During Radiotherapy
Authors Bacher H , Schweyen R , Kuhnt T, Leplow B, Hey J
Received 28 May 2020
Accepted for publication 21 July 2020
Published 28 September 2020 Volume 2020:14 Pages 1751—1759
DOI https://doi.org/10.2147/PPA.S262471
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Helene Bacher,1 Ramona Schweyen,1 Thomas Kuhnt,2 Bernd Leplow,3 Jeremias Hey1
1Department of Dental Prosthetics, University Hospital Halle/Saale, Halle (Saale), Germany; 2Clinic for Radiotherapy, University Hospital Leipzig, Leipzig, Germany; 3Institute of Psychology, Institute for Therapy and Health Research (IFT-Nord), Martin Luther University Halle-Wittenberg, Halle/Saale, Germany
Correspondence: Helene Bacher
Department of Dental Prosthetics, University Hospital Halle/Saale, Magdeburger Straße 16, Halle (Saale) 06112, Germany
Tel +49 345 557 3787
Fax +49 345 557 3779
Email [email protected]
Purpose: A patient information leaflet (PIL) on oral and dental care during radiotherapy was tested whether and at which time during therapy it would be helpful to increase the knowledge about the therapy and the resulting side effects and the management of these. Additionally, the participants’ subjective perception of being well informed about the topic was examined.
Participants and Methods: Surveys were conducted in August 2018–April 2019, at the University Hospitals Halle and Leipzig (Germany). The study population consisted of patients who were treated with radiotherapy in the head and neck region. Half of them received access to the PIL. The survey was conducted with three different versions of a printout questionnaire, which covered the relevant topics at three different times of therapy. The time the participants were surveyed depended on the time of their first therapy appointment. The items of the questionnaires tested their concrete knowledge and assessed the subjective perception of the level of information received.
Results: Of the 81 participants who received the PIL, 93.8% read it and 92.1% of them considered it helpful. The sample comprised 181 participants aged 32 to 85 years (M = 62.9), of which 135 were males, 42 were females, and 4 were unspecified. Evaluation showed a difference of 4.7%; 18.5%; and 13.6% in correct answers between subjects with and without access to the PIL before, during, and after the therapy, respectively. The assessment of the participants’ personal information level was independent of their access to the PIL (chi-squared test, p = 0.89).
Conclusion: Having access to the PIL increased participants’ ability to answer the questionnaires correctly. Access to the PIL had no influence on the subjective feeling of being well informed.
Keywords: patient education, cancer, survey, oral hygiene, therapy, patient satisfaction
Introduction
Malignant tumors in the head and neck region are among the most frequent forms of malignant tumors, with approximately 17,500 new cases per year in Germany.1 Treatment options include surgical resection, radiation, chemotherapy, or a combination of these. Radiotherapy takes place either curatively, as a pre- or postoperative supplement, or as palliative therapy. This high-dose radiation in the head and neck area is often associated with side effects in the oral cavity.2
The most common short-term adverse effects are mucositis, reduced salivary flow, loss of taste sensitivity, an increased risk of candida infestation of the oral mucosa, and trismus. In the long term, atrophy of the epithelium and xerostomia are to be expected. Secondarily, there is an increased risk of caries due to reduced salivary flow and radiation damage to enamel and dentin; and a change in diet to carbohydrate-rich, soft, cariogenic food. The change in diet can be caused by reduced salivary flow, inflamed and pain-sensitive mucous membranes, and altered taste perception. In addition, the healing of defects in the oral cavity decelerates and the risk of osteoradionecrosis is highly increased. This is the most severe side effect. To reduce the risk of osteoradionecrosis, an extensive preliminary dental examination is performed. In subsequent dental pre-treatments, teeth that present a risk are rehabilitated or, if necessary, removed.
Furthermore, side effects of radiotherapy in the head and neck area can be minimized by implementing correct usage of radiation splints, following recommended oral hygiene practices, and ensuring adequate nutrition.3 Comprehensive patient education regarding the effects and the possible side effects of radiation therapy and how to manage them, as well as the importance of a dental pre-treatment before a planned radiotherapy in the head and neck area forms the basis for all subsequent therapeutic interventions.
However, the extensive and precisely coordinated time schedule required for reducing or eliminating malignant tumor tissue often limits the time available for extensive consultation, dental examination, and treatment prior to cancer therapy. Furthermore, the consultation for a dental intervention is often not based on personal motivation, but rather on the necessity imposed by the planned radiotherapy. In this situation, it is difficult to sensitize the patient appropriately to the difficulties associated with the intraoral side effects of radiotherapy their association with dental care and to encourage them to adopt appropriate oral hygiene. Additionally, patients are often skeptical about the need for the preliminary dental examination and treatment.
Comprehensive patient education reportedly increases compliance and patient satisfaction.4 This is difficult to achieve in the abovementioned context, given that the ability of patients to process information from medical consultations is generally limited.5,6 In particular, the dental consultation typically occurs while patients are experiencing substantial psychological stress, which reduces the intake and retention of essential information.7
The information and instructions related to the dental education interview pertain to all stages of treatment, and thus, much of the information should be retained over a long period of time to enable its recall at the relevant time. Numerous clinical studies have shown that the amount of information that is received can be increased by using written material.8 Current guidelines recommend the evaluation of written informative material together with patients.8,9 However, whether written information is also beneficial for the concrete increase in knowledge in patients who require dental education prior to cancer therapy has not yet been evaluated.
The present study aimed to investigate a) whether, and at which time-point during therapy, the use of a patient information leaflet (PIL) could increase the knowledge regarding oral and dental care among patients undergoing radiotherapy for cancer. Furthermore, b) whether the participants feel better informed by reading the PIL in addition to the medical consultation was of interest.
Materials and Methods
The study protocol was approved by the medical faculty’s ethics committee at the Martin Luther University Halle-Wittenberg (reference number 2017–119), and the study was conducted in accordance with the Declaration of Helsinki (2013) and based on the conduct of medical research in accordance with ethical principles.
Materials
PIL
The contents of the PIL were defined by a panel of experts, consisting of radiotherapists, oral and maxillofacial surgeons, and dentists from the university hospitals of Halle/Saale and Leipzig, and were evaluated according to their relevance. The content and graphic design were determined according to current guidelines and pre-evaluated with unaffected subjects in a previous study.10
The PIL was designed to provide information relevant to all periods of radiotherapy in the head and neck area.
Questionnaires
All questionnaires were designed using a template structured to facilitate collection of general information from participants. Participants were asked to state their age, sex, and their educational level (response option from four different options). In addition, answering the question related to access to the leaflet was requisite. Furthermore, the participants were asked to evaluate the statement: “I feel well informed about the topic in question” on the basis of the possible answers “Completely untrue,” “Rather untrue,” “I am not able to judge,” “Rather true,” “Completely true.” The overall aim was also to assess the extent to which the participants felt generally informed, independently of the access to the PIL. In addition, the group of participants who received the PIL were asked if they read the PIL and were asked to evaluate it as “helpful” or “not helpful,” if applicable. Three different versions of the questionnaire (A–C) were developed to test the gain in knowledge achieved by reading the PIL (Table 1). They covered topics relevant to the present status of therapy. The items were presented in a format that could be answered as “correct” or “incorrect.”
 |
Table 1 Characteristics of the Questionnaires |
Participants
The participants were divided into three groups with inclusion criteria according to the timing of the survey: Group A included patients who had been scheduled for radiotherapy in the head and neck region at the time of the survey, but who had not yet undergone dental pre-treatment. Group B included patients who were in at least the 4th week of radiotherapy in the head and neck region at the time of the survey. Group C included patients whose head and neck radiotherapy had been completed at least 4 weeks prior to the examination. The exclusion criteria for all patients were having previous radiotherapy in the head and neck region, and severely reduced physical or psychological function. Only patients who had reached the age of eighteen and were able to consent were included. A written declaration of consent after receiving verbal and formal information about the aims and methods of the study and the randomization process was a prerequisite for participation in the study. As per sample size calculation (t-tests - Correlation: Point biserial model) at least 21 participants were required per group.
Methods
Surveys were conducted in August 2018–April 2019, at the Clinic for Dental Prosthetics, Clinic for Radiotherapy of the University Hospital Halle/Saale, and Clinic for Radiotherapy of the University Hospital Leipzig. The total number of participants was informed by a regular medical consultation. Half of the participants also received the PIL as a source of information. The division of the participants in groups was randomized according to the time of the first consultation prior to the planned radiotherapy. The PIL was handed out to all participants between December 2018 and March 2019, irrespective of the study schedule. The participants received the PIL from the treating radiotherapist independently of the medical consultation before being referred for a preliminary dental examination. The group assignment was randomized according to the time period of the survey. If the participants contacted the treating radiotherapist after or within the period of provision of the PIL, they could be assigned to the group “Access to the PIL.” Participants who made an appointment before the period of provision of the PIL, could not have access to the PIL and were assigned to the group “No Access to the PIL.” Participants were interviewed following the appointment for the manufacture of the radiation mask (Group A), within the 6 weeks of radiation treatment (Group B), or at or after the first follow-up appointment after completion of radiation therapy at the University Clinic for Radiotherapy at Halle and Leipzig (Group C). At the time of the survey, the participants were asked about their access to the PIL and divided into the subgroups: “Access to the PIL” and “No Access to the PIL.” To leave the handling of the PIL as uninfluenced as possible by the course of the study, the participants were unaware at the time of receiving the PIL that its information could be queried at a later point in time as part of a survey. At the time of the interview, the participants were informed that there was a trial PIL being conducted in a randomized fashion. They were given the opportunity to participate in the survey and were informed that this would require the completion of a questionnaire. The PIL was provided to all patients who decided not to participate. After confirming participation in the study, the group that initially had no access to the PIL was given access to the PIL. Questionnaires were distributed after comprehensive clarification of all aspects of the study and obtaining voluntary written consent from the participants. Depending on the current status of radiotherapy, participants received questionnaire version A (prior to radiotherapy), B (during radiotherapy), or C (aftercare of radiotherapy). This questionnaire was provided to all participants in A4 format as a printout and was to be completed in handwriting. The completed questionnaire could be returned anonymously at any time within the following two weeks. No personal data were collected. Participants were informed that due to the complete anonymization, it was no longer possible to withdraw after submitting the completed questionnaire. The questionnaire was issued and collected by a person unrelated to the treatment process.
Statistical Evaluation
The data were digitized and evaluated using SPSS (IBM, Ehningen, Germany) and Microsoft Excel (Microsoft, Redmond, WA, USA). The Kolmogorov–Smirnov test, with significance correction according to Lilliefors, was performed to test for normal distribution. Depending on the normal distribution and the type of variable (categorical, metric), the chi-squared test, the Mann–Whitney U-test, and the Kruskal–Wallis test were used to calculate the significance of differences. A p-value below 0.05 was considered significant.
Results
Descriptive Statistics
The characteristics of the investigated study population are shown in Tables 2 and 3. The mean age of the participants was 62.9 years and ranged from 32 to 85 years. There were 135 males (74.5%) and 42 (23.2%) females from a total of 181 participants, and 4 (2.2%) did not specify their sex.
 |
Table 2 Number of Participants per Group |
 |
Table 3 Grouping According to Educational Levels of the Participants |
Evaluation of the PIL
Of the participants who received the PIL, 93.8% read it. Of these, 92.1% considered the PIL to be helpful. Table 4 shows the assessment of the PIL by the different groups. The proportion of participants who read the received PIL was higher in Groups B and C than in Group A (chi-squared test, p = 0.15).
 |
Table 4 Use and Assessment of the PIL by the Participants Who Had Access to the PIL |
Assessment of Personal Information Level by Participants
Regardless of whether they had received the PIL, most of the participants evaluated the statement “I feel well informed about the subject in question” as “Rather true” or “Completely true” (Figure 1). The assessment of their personal information level was independent of their access to the PIL (chi-squared test, p = 0.89).
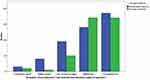 |
Figure 1 Assessment of personal information level by the probands. |
Knowledge Gained from the PIL
The average percentage of correctly answered items for all questionnaires of the participants who did not have access to the PIL was 61.19%. The groups who had access to the PIL had a higher mean percentage of correctly answered questions in all participant groups. The largest difference between the groups with and without access to the PIL was found in Group B (Table 5).
 |
Table 5 Average Percentage of Correctly Answered Items According to PIL Access |
The topic area covering the handling of prostheses during radiotherapy had the lowest mean percentage of correctly answered items in both groups. The largest mean percentage of correctly answered items occurred in the field of handling radiation splints. The largest differences between the groups were found in the topics “Prevention of mucosal burning” and “Dry mouth” (Table 6).
 |
Table 6 Average Percentage of Correctly Answered Items According to Main Topic |
Applicability of the PIL
The mean percentage of correctly answered items in participants without access to the PIL differed according to education (Kruskal–Wallis-test, p=0.30), with participants in Group 4 having the highest mean percentage of correctly answered items and participants in Group 1 having the lowest. The largest difference in the average percentage of correctly answered items between participants with and without access to the PIL was seen in Group 2 and in Group 4 (Table 7).
 |
Table 7 Average Percentage of Correctly Answered Items According to Educational Level |
Discussion
Use and Assessment of the PIL by Participants
Most participants (93.8%) who received the PIL read it, and 92.1% considered it to be helpful. This extensive use of written material among patients treated with radiotherapy in the head and neck region were also reported in other studies.11–13 The time of the survey had no significant association on this result. Most of the participants read the PIL before the preliminary dental examination and used it in the further course of therapy. Nevertheless, the proportion of participants who said they had not read the PIL was higher in Group A than in the others. This suggests that the need for PIL is higher during and after radiotherapy than before it starts. The occurrence of side effects is a possible trigger for this increased interest in additional information.13 Additionally, Fitchett et al14 concluded that the side effects of radiotherapy in the head and neck area place a great psychological burden on patients and cause an increased need for information. Furthermore, the memory of the medical consultation within the scope of therapy planning is still present at the beginning of the therapy, whereas within a month of the consultation, the memory of information provided decreases.6,15 Consequently, it is plausible that the PIL could be used as a memory aid, particularly during the course of therapy. The additional use of the PIL to prepare for the doctor-patient consultation should be encouraged by the person providing the PIL, as this offers considerable advantages. Pre-informed patients are then able to ask specific questions and can improve their ability to follow the conversation.8,16,17
Knowledge Gained from the PIL
Within the Group of participants who exclusively relied on information from the doctor–patient conversation, a similarly large proportion of correctly answered items were found among all groups, that were divided according to the time-point during radiotherapy. These participants mainly considered that they were sufficiently informed, regardless of their lack of access to the PIL. This was in accordance with the results of other studies.4,18 The PIL contained the information that was discussed in the medical consultation, but in greater detail and with additional information and, possibly, information that may not have been relevant to the reader such as how to handle prostheses. The doctor–patient consultation forms an essential part of patient information and is preferred by most patients, because of its tailored nature, the confidential relationship with the doctor, and the opportunity to ask questions.16
In this study, written material did not improve the subjective assessment of the participants’ own level of information. However, participants who could additionally rely on information from the PIL on average answered a larger percentage of the items correctly. In other studies, written information in addition to the medical consultation positively influenced the communication of information.8 The difference in correctly answered items between the groups of subjects with and without access to the PIL was between 4.7% and 18.5% and averaged 11.91%. Compared to a similarly structured study by Humphris et al19 this mean value was lower. The main difference between the present study and that by Humphris et al depends on the sample. Humphris et al19 examined persons who were not directly affected by the topic of the written material, while we examined patients who were actually treated with radiotherapy in the head and neck area. When interviewing the affected patients, the generally overestimated long-term memory capacity for retaining information from a doctor-patient conversation can be further reduced in patients who are undergoing radiotherapy in the head and neck region and dealing with a marked physical and psychological burden.7,20
When differentiating the percentage of correctly answered items according to the time of the survey within the course of radiotherapy, there was a marked difference in the percentage of correctly answered items of participants with and without access to the PIL in Groups B and C, as compared to Group A. This may be related to the finding that a larger proportion of Group A who received the PIL did not read it. The diagnosis of the disease is often made in its advanced stage, so that those patients are unexpectedly confronted with a life-threatening disease, for which the therapy is often accompanied by disfiguring side effects in the facial area.7 In addition to the fear and uncertainty caused by this situation, there is an increased stress in view of the acute need for therapeutic intervention, which additionally involves transference of a large amount of information and clarification discussions. Prophylactic improvement of oral hygiene may seem to be of secondary importance to patients in this context. However, in a life situation characterized by anxiety, insecurity, and helplessness, informing oneself about the disease, its side effects, therapeutic options, and prophylactic interventions may assist in regaining a sense of control and self-determination. Patient satisfaction and compliance are closely linked to the information provided by the responsible physician.21 The connection between the prophylactic improvement of oral hygiene with long-term side effects should be addressed both during the educational interview and in the written information.
The frequency of medical consultations is lower, further on in the course of therapy and the information and recommendations for action are of practical use to the patients. The demand for comprehensive information, particularly in terms of dealing with the side effects that arise during the course of treatment, is high.11,17 The information from the PIL concerning topics such as “mucosal burning” and “dry mouth” could most likely be reproduced correctly in the questionnaires. Both topics refer to side effects of radiotherapy that severely affect the quality of life of patients. In other studies, it was found that the quality of communication between the doctor and patient is often reduced due to different priorities.14 This clarifies the importance of tailoring the content to the needs of patients when communicating information.17
The proportion of correctly answered items in topics such as “handling prostheses during radiotherapy” was low in both groups. These topics are not relevant for the entire group of participants. The interest of the reader plays a major role in the ability to recall information.21 Written information cannot be tailored to the individual case of each reader, but should include all relevant topics.8
Due to the complete anonymity of the participants, it is not possible to determine to what extent the study cohort was homogeneous regarding certain patient characteristics such as the psychological state of the patients, the intake of certain drugs, the aim of the radiotherapy (curative/palliative), or the tumor localization and size. These potential biases could not be excluded but may have influenced the performance of the participants in the study. Regarding the statistical evaluation of the results, this lack of patient data has a negative effect and limits the validity of the study. From a clinical perspective, it must be acknowledged that patients treated with radiotherapy in the head and neck region also represent a very inhomogeneous group. In further studies, the inclusion of more extensive patient data and the combination of psychological tests would be beneficial.
A further limitation of the present study was its reliance on the unprovable statement of the patients whether they read the PIL. In the future, this limitation could be circumvented through an online survey, which would record the number of times the respondents opened the online document. Furthermore, other sources of information may have had an influence on the answers to the questions. To what extent the patients had informed themselves about the topic cannot be reconstructed.
The PIL and the accompanying questionnaires were written in German. A good understanding of the language was assumed among the study participants, but this could not be evaluated due to the complete anonymization. To reach a larger share of the patient clientele, a multilingual version of the PIL is planned for the future.
The involvement of patients in the development and evaluation of written information material is an important prerequisite to ensure that its use in clinical practice is sustainable. Guidelines for the development of written information material require this clinical evaluation,8 which is often not realized due to the extensive time investment. The present study can be seen as an incentive and a guide for the clinical evaluation of such written information material.
Applicability of the PIL
Regardless of the educational level of the study participants, access to the PIL led to a higher average number of correctly answered items. The group of participants with a lower secondary school-leaving certificate benefited the most from access to the PIL. This group represents a large proportion of the patients in this study, and also the overall population of patients with head and neck tumors.22 The significance of these results is limited by the strongly varying group sizes according to the educational levels of the participants. Particularly small group sizes within the educational levels of the participants minimize the validity. This limitation could be avoided in a study with a larger sample.
The results of the study refer to German-speaking patients requiring radiotherapy in the head and neck region. It is conceivable that the results could be transferred to groups of test persons speaking other languages. Considering the increased stress exposure of patients receiving radiotherapy in the head and neck region compared to patients receiving radiation in other body regions, these results can only be transferred to other patient groups to a limited extent.
Conclusion
The present study clearly shows the benefit of written information material as a supplement to the doctor-patient consultation; as well as for educating patients on the management of dental and oral side effects of head and neck radiotherapy. Information on long-term side effects of the disease and how to deal with them can be obtained through the PIL at the relevant time. Nevertheless, further multi-center studies with larger patient cohorts and the additional inclusion and evaluation of further patient-related data are recommended. The intended effect on patient behavior regarding prophylaxis and therapy interventions of possible side effects should be investigated in further studies.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Federal Ministry of Health. Bericht zum Krebsgeschehen in Deutschland; 2016. Available from: https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/3_Downloads/K/Krebs/Krebsgeschehen_RKI.pdf.
2. Sroussi HY, Epstein JB, Bensadoun R-J, et al. Common oral complications of head and neck cancer radiation therapy: mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Cancer Med. 2017;6(12):2918–2931. doi:10.1002/cam4.1221
3. Carvalho CG, Medeiros-Filho JB, Ferreira MC. Guide for health professionals addressing oral care for individuals in oncological treatment based on scientific evidence. Support Care Cancer. 2018;26(8):2651–2661. doi:10.1007/s00520-018-4111-7
4. Waller A, Forshaw K, Bryant J, Mair S. Interventions for preparing patients for chemotherapy and radiotherapy: a systematic review. Support Care Cancer. 2014;22(8):2297–2308. doi:10.1007/s00520-014-2303-3
5. Sandberg EH, Sharma R, Sandberg WS. Deficits in retention for verbally presented medical information. Anesthesiology. 2012;117(4):772–779. doi:10.1097/ALN.0b013e31826a4b02
6. Latorre-Postigo JM, Ros-Segura L, Navarro-Bravo B, Ricarte-Trives JJ, Serrano-Selva JP, López-Torres-Hidalgo J. Older adults’ memory for medical information, effect of number and mode of presentation: an experimental study. Patient Educ Couns. 2017;100(1):160–166. doi:10.1016/j.pec.2016.08.001
7. Lang H, France E, Williams B, Humphris G, Wells M. The psychological experience of living with head and neck cancer: a systematic review and meta-synthesis. Psycho-Oncology. 2013;22(12):2648–2663. doi:10.1002/pon.3343
8. Sustersic M, Gauchet A, Foote A, Bosson J-L. How best to use and evaluate patient information leaflets given during a consultation: a systematic review of literature reviews. Health Expect. 2017;20(4):531–542. doi:10.1111/hex.12487
9. Lampert A, Wien K, Haefeli WE, Seidling HM. Guidance on how to achieve comprehensible patient information leaflets in four steps. Int J Qual Health Care. 2016;28(5):634–638. doi:10.1093/intqhc/mzw077
10. Bacher H, Schweyen R,Vordermark D, Leplow B, Hey J. Development and Validation of an Information Leaflet on Oral Care for Irradiated Patients. Patient Prefer Adherence. In press 2020.
11. Jabbour J, Milross C, Sundaresan P, et al. Education and support needs in patients with head and neck cancer: a multi-institutional survey. Cancer. 2017;123(11):1949–1957. doi:10.1002/cncr.30535
12. Kim C, Dillon R, Nica L, Berthelet E, Keyes M, Hamilton SN. Information needs of patients diagnosed with head and neck cancer undergoing radiation therapy: a survey of patient satisfaction. J Cancer Educ. 2020. doi:10.1007/s13187-020-01719-z
13. Fletcher C, Flight I, Chapman J, Fennell K, Wilson C. The information needs of adult cancer survivors across the cancer continuum: a scoping review. Patient Educ Couns. 2017;100(3):383–410. doi:10.1016/j.pec.2016.10.008
14. Fitchett RC, Aldus EJ, Fitchett LR, Cross J. The lived experience of head and neck cancer patients receiving curative radiotherapy: a systematic review and meta-ethnography. Psycho-Oncology. 2018;27(9):2077–2086. doi:10.1002/pon.4790
15. Harada CN, Natelson Love MC, Triebel KL. Normal cognitive aging. Clin Geriatr Med. 2013;29(4):737–752. doi:10.1016/j.cger.2013.07.002
16. Pollock K, Moghaddam N, Cox K, Wilson E, Howard P. Exploring patients’ experience of receiving information about cancer: a comparison of interview and questionnaire methods of data collection. Health. 2011;15(2):153–172. doi:10.1177/1363459309360789
17. Schnitzler L, Smith SK, Shepherd HL, et al. What information is communicated by radiation therapists to patients during education sessions on the first day of treatment? Eur J Cancer Care (Engl). 2019;28(1):e12911. doi:10.1111/ecc.12911
18. Riedl D, Gastl R, Gamper E, et al. Cancer patients’ wish for psychological support during outpatient radiation therapy. Strahlenther Onkol. 2018;194(7):655–663. doi:10.1007/s00066-018-1288-0
19. Humphris GM, Field EA. The immediate effect on knowledge, attitudes and intentions in primary care attenders of a patient information leaflet: a randomized control trial replication and extension. Br Dent J. 2003;194(12):683–688. doi:10.1038/sj.bdj.4810283
20. Tarsia M. Implicit and explicit memory biases in mixed anxiety–depression. J Affect Disord. 2003;77(3):213–225. doi:10.1016/S0165-0327(02)00119-2
21. Ley P. Communicating with Patients — Improving Communication, Satisfaction and Compliance. Cheltenham: Stanley Thornes; 1998.
22. Conway DI, Brenner DR, McMahon AD, et al. Estimating and explaining the effect of education and income on head and neck cancer risk: INHANCE consortium pooled analysis of 31 case-control studies from 27 countries. Int J Cancer. 2015;136(5):1125–1139. doi:10.1002/ijc.29063
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
