Back to Journals » Advances in Medical Education and Practice » Volume 9
U.S. medical school curricula on working with medical interpreters and/or patients with limited English proficiency
Authors Himmelstein J, Wright WS , Wiederman MW
Received 1 June 2018
Accepted for publication 24 July 2018
Published 28 September 2018 Volume 2018:9 Pages 729—733
DOI https://doi.org/10.2147/AMEP.S176028
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Jessica Himmelstein, William S Wright, Michael W Wiederman
Department of Biomedical Sciences, University of South Carolina School of Medicine Greenville, Greenville, SC, USA
Purpose: The United States has an increasing population of individuals with limited English proficiency (LEP). Language access is a right for individuals with LEP in the health care system. As such, it is important for medical providers to be appropriately trained to work with individuals with LEP. Therefore, the purpose of this study was to describe curricula offered by United States medical schools to teach medical students to work with medical interpreters and/or patients with LEP.
Methods: An electronic survey was sent in March 2017 to administration at the 147 Liaison Committee on Medical Education® accredited medical schools as of November 7, 2016. The survey consisted of the following question: “As part of your medical school’s curriculum, are students provided specific instruction addressing how to work with medical interpreters and/or patients with limited English proficiency (LEP)?” with different follow-up questions for schools that responded “Yes” vs “No”.
Results: Responses were received from 26% (38/147) of medical schools. Among schools responding to the survey, 76% (29/38) offered a curriculum that provides instruction of how to work with medical interpreters and/or patients with LEP. Of schools that provide instruction, teaching methods included didactic sessions (34% [10/29]) and standardized patient experiences (34% [10/29]). In addition, 76% (22/29) offer training in the first 2 years of medical school and 28% (8/29) offer training in the third and fourth years of the curriculum. Sixty-two percent (18/29) of respondents that offered a formal curriculum have been administering a formal curriculum for ≤10 years.
Conclusion: The majority of the responding medical schools offer formal instruction of how to work with medical interpreters and/or patients with LEP. Most schools started this type of instruction in the last 10 years with most instruction occurring in the first 2 years of an undergraduate medical curriculum.
Keywords: health resource, culturally competent care, health services administration, education, survey
Introduction
Over the past several decades the population in the United States has become more diverse. According to the 2000 US Census data, 18% (47.0 million) of the total population aged ≥5 reported speaking a language other than English at home. This represents a 39% relative increase from 1980 when only 11% (23.1 million) of the total population reported speaking a language other than English at home.1 The 2000 US census also revealed that the “proportion of the population aged 5 and over who spoke English less than “Very well” grew from 4.8 percent in1980, to 6.1 percent in 1990, and to 8.1 percent in 2000”.1 Illustrating that from 1980 to 2000, the population in the United States defined to have limited English proficiency (LEP) had a relative increase of 41%.
In 2010, the American Community Survey (ACS) Report became the primary source for language data in the United States because language would no longer be asked on the decennial census.2 The most recent ACS report (2011) shows some unique changes from the trend noted in 2000. From the previous report, there was a 3% absolute increase in individuals who spoke another language other than English at home.2 “Of 291.5 million people aged 5 and over, 60.6 million people (21% of this population) spoke a language other than English at home.”2 Of those who spoke another language, about 22.4% were defined as limited English proficient in that they either did not speak English well or did not speak English at all.2 These data suggest there has been an overall increase in the proportion of individuals who speak another language other than English at home but those individuals with LEP has increased only slightly during that same timeframe.
As the population demographics in the United States have changed with growing numbers of immigrants, fatal breakdowns in patient–provider communication elevated language access for individuals with LEP as a fundamental right.3 Federal mandates, such as including language access as part of Title VI of the 1964 Civil Rights Act and Executive Order 13166, that mandate language services be provided for individuals with LEP were established4–6 to address the breakdowns in communication.
Now when non-English-speaking patients enter the health care system, it is standard of care that they are provided language access by an interpreter.7 Interpretation services are to be provided to patients in their language of preference by an interpreter, either in-person or via video or telephone. Ways to improve consistency in requesting these services and their proper use are areas of continued research.8–11
Considering that language access is a right for individuals with LEP, it is important for the next generation of medical providers to be appropriately trained to work with this population. A study that surveyed medical students’ preparedness to work with medical interpreters found that only “twenty percent of medical students reported being very well or well prepared to care for LEP patients”.12 The study additionally revealed that “skill level working with interpreters, prevalence of LEP patients seen, and training year were correlated (P<0.001) with LEP preparedness”.12 In another study, medical students who function as emergency medical technicians reflected often on “providers” inability to effectively manage communication barriers resulting from cultural and/or language differences”.13
Much advancement has been made to better prepare students to work with LEP individuals;14 however, little is known about the types of curricula that medical schools are currently offering to prepare their students. The purpose of this study was to survey United States medical schools to describe the type of curriculum offered to teach medical students to work with medical interpreters and/or patients with LEP.
Materials and methods
Survey methods
The survey was sent to United States medical schools that had preliminary, provisional, or full accreditation through the Liaison Committee on Medical Education® (LCME®) as of November 7, 2016. Each LCME-accredited school’s website was then reviewed and an individual contact was selected that was either at the senior associate dean or associate dean level for academic affairs, medical education, or curriculum. A solicitation email message was sent to these individuals (N=147) on March 14, 2017; within the message was a link to the electronic survey hosted at SurveyMonkey®. A subsequent reminder message was sent 1 week later with the schools being given 3 weeks to respond.
The survey consisted of the following initial question: “As part of your medical school’s curriculum, are students provided specific instruction addressing how to work with medical interpreters and/or patients with limited English proficiency (LEP)?” If such a curriculum was offered, follow-up questions focused on describing the curriculum and its evaluation and feedback. If a curriculum was not offered, the following question was asked to determine need at the school: “Do you think there is a need for that type of educational session at your institution? Please describe why or why not.” The survey was voluntary and anonymous, allowing respondents to only disclose their medical institution, region, and/or state if desired.
Ethical approval
The study was reviewed and exempted by the University of South Carolina Institutional Review Board as it was determined Not Human Research due to methodology.
Results
Demographics
A total of 147 surveys were sent and 38 schools (26% response rate) completed the survey. The 38 respondents represented medical schools from each region of the country. Table 1 presents school responses by Association of American Medical Colleges Group on Educational Affairs regions.15 A total of 23 states were represented by at least one medical school with a maximum of three schools in one state. Four of the 38 participants did not specify their medical school institution or specific state; however, one did specify the region.
Schools offering interpreter and/or LEP curricula
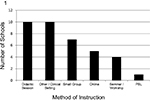
Of the 38 respondents, 29 (76%) stated that their institutions did offer a curriculum intended to prepare students to work with medical interpreters and/or patients with LEP (Table 1). The method of instruction used to train students to work with medical interpreters and/or patients with LEP is presented in Figure 1. Learning sessions were usually led by a medical provider or an individual from language services geared to provide training to the entire class and/or within small-group sessions.
Ten schools responding (34%) offer a curriculum to prepare students to work with medical interpreters and/or LEP stated that their institution offered a standardized patient experience for students to practice working with patients with LEP and medical interpreters (Table 1). The format of these sessions varied in format where students practice one-on-one working with interpreters to small-group sessions where students work with interpreters together.
Figure 2 presents the number of years that a school has administered a curriculum designed to teach medical students to work with medical interpreters and/or patients with LEP. Of those schools with such a curriculum, 18 (62%) have been offering a formal curriculum for ≤10 years.
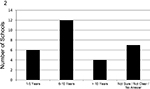  | Figure 2 Number of years a school has been administering a curriculum to teach medical students to work with medical interpreters and/or patients with limited English proficiency (n=29). |
Curriculum to train students to work with interpreters and/or patients with LEP is offered by 15 schools in year 1, 16 schools in year 2, 10 schools in year 3, and 2 schools in year four with 1 school not providing the curricular year. Two schools (7%) train students in all four years of the curriculum, one school (3%) trains students in 3 years, seven schools (24%) train students in 2 years, and 19 schools (66%) offer training in 1 year.
Seventeen schools responding (59%) report some type of evaluation of the specific sessions related to working with medical interpreters and/or patients with LEP while 12 schools (41%) do not have evaluations of the content taught.
Fourteen schools responding (48%) report positive student feedback regarding curricular instruction specific to medical interpreters and/or patients with LEP while two schools (7%) report mixed student feedback. Eleven schools (38%) either did not provide feedback from students or did not have feedback from students. Two schools (7%) report feedback from students is used to make changes to content and teaching; however, there is no clarification if the feedback is positive or negative.
Schools that do not offer interpreter and/or LEP curricula
Nine respondents (24%) stated their institution did not offer any curriculum intended to prepare students to work with medical interpreters and/or patients with LEP (Figure 1). These respondents were asked whether they thought there was a need for this type of educational curriculum, and answers varied widely. Six schools (67%) agreed that this type of training is needed. Some reported having it available as optional coursework, or at least discussing the topic in third-year coursework, but it was still not part of the formal curriculum. Time constraints were listed as the major barrier to incorporating this type of training into the formal curriculum. Those respondents who did not see a need for this type of training in medical school curricula stated reasons that included having a large student population that was bilingual (primarily English and Spanish) and/or that this type of training may be better suited at resident level.
Discussion
To our knowledge, this is the first study to survey medical schools nationally for curricula that focus on working with an interpreter or individuals with LEP. Of schools that responded, most medical schools reported having some form of formal curriculum to address this educational need/opportunity for this population. Of schools that did not offer any formal curriculum, most stated a desire to implement this curriculum but found difficulties incorporating it within the tight time constraints of the current curriculum. A few schools reported having a large bilingual student population and therefore did not see the need for this instruction. Training of students to work with medical interpreters and/or patients with LEP is important as it has been reported that the “use of professional interpreters is associated with improved clinical care” and “appear to raise the quality of clinical care for LEP patients to approach or equal that for patients without language barriers”.16
In the majority of institutions that do offer a formal curriculum to train medical students to work with medical interpreters and/or patients with LEP, it was interesting to see the variety of teaching modalities offered, primarily in the first 2 years of medical training. Most teaching modalities are not formally evaluated, so their true effectiveness is unknown. However, one important finding was that the institutions that provided opportunity for students to practice working with medical interpreters and patients with LEP were some of the better evaluated and better received sessions based on feedback by medical students. These findings suggest the importance of not only informing students of the importance of language services and language-concordant care but also allowing them to practice this either individually or within a small group setting.
Most schools responding to the survey have started offering a curriculum to teach medical students to work with medical interpreters and/or patients with LEP in the last10 years (Figure 2). This is an encouraging and important finding given the increase in individuals who speak a language other than English at home,1 and patient care is improved with the use of interpreters.16
One advantage of this survey is that it is a low-cost method to determine the extent of curriculum offered in medical education to address a need of training students to work with medical interpreters and/or patients with LEP. A limitation to this study is the small response rate to the survey. Additionally, selection bias could have led to a higher percentage of institutions that self-report offering this type of curriculum, since those who do not offer this curriculum may be less likely to self-report.
Conclusion
As the population in the United States becomes increasingly diverse, it is important that future medical providers are trained to meet the growing needs of this population through appropriate language services. Our data show that most medical schools responding to the survey train students to work with medical interpreters and/or individuals with LEP. Future studies should target medical school curricula in specific geographic regions and effectiveness of teaching pedagogies when training medical interpreters and/or patients with LEP.
Author contributions
JH is responsible for conceptualization of project, survey development, data acquisition, and preparation of manuscript. WSW is responsible for list of target individuals within each medical school, data analysis, and preparation of manuscript. MW is responsible for survey development, data acquisition, and revision of manuscript. All authors agree to be accountable for all aspects of the work. All authors have reviewed and approved the final draft of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Shin HB, Bruno R. Language use and English-speaking ability: 2000; census 2000 brief. 2003C2KBR-29. | ||
Ryan C. Language use in the United States: 2011. American Community Survey Reports. 2013;22:1–16. | ||
Price-Wise G. Language, culture, and medical tragedy: The case of Willie Ramirez. Health Affairs Blog. 2008. | ||
Title VI of the civil rights act of 1964: Title 42 - the public health and welfare. The United States Department of Justice Web site. Available from: https://www.justice.gov/crt/title-vi-1964-civil-rights-act. Accessed April 27, 2018. | ||
Clinton WJ. Improving access to services for persons with limited English proficiency. Executive order 13166, 2000. | ||
Perkins J. Ensuring Linguistic Access in Health Care Settings: An Overview of Current Legal Rights and Responsibilities. Washington, DC: Kaiser Commission on Medicaid and the Uninsured; 2003. | ||
The National CLAS Standards. U.S. Department of Health and Human Services Office of Minority Health Web site; 2016. Available from: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=2&lvlid=53. Accessed April 27, 2018. | ||
Kim EJ, Kim T, Paasche-Orlow MK, Rose AJ, Hanchate AD. Disparities in hypertension associated with limited English proficiency. J Gen Intern Med. 2017;32(6):632–639. | ||
Patel DN, Wakeam E, Genoff M, Mujawar I, Ashley SW, Diamond LC. Preoperative consent for patients with limited English proficiency. J Surg Res. 2016;200(2):514–522. | ||
Brooks K, Stifani B, Batlle HR, Nunez MA, Erlich M, Diaz J. Patient perspectives on the need for and barriers to professional medical interpretation. R I Med J. 2016;99(1):30–33. | ||
Njeru JW, Boehm DH, Jacobson DJ, et al. Diabetes outcome and process measures among patients who require language interpreter services in Minnesota primary care practices. J Community Health. 2017;42(4):819–825. | ||
Rodriguez F, Cohen A, Betancourt JR, Green AR. Evaluation of medical student self-rated preparedness to care for limited English proficiency patients. BMC Med Educ. 2011;11:26. | ||
Russ-Sellers R, Blackwell TH. Emergency medical technician training during medical school: benefits for the hidden curriculum. Acad Med. 2017;92(7):958–960. | ||
Vela M, Fritz C, Jacobs EA. Establishing medical students’ cultural and linguistic competence for the care of Spanish-speaking limited English proficient patients. J Racial Ethn Health Disparities. 2016;3(3):484–488. | ||
Association of American medical colleges (AAMC): Group on educational affairs. Available from: https://www.aamc.org/members/gea/. Accessed May 8, 2018. | ||
Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727–754. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.