Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 15
Uptake of HIV Self-Testing and Associated Factors Among Female Sex Workers at Non-Governmental HIV Testing Facilities in Debre Markos and Bahir Dar Towns, Northwest Ethiopia, 2022
Authors Nibret Eskezia B, Tafere Y, Aschale A, Abebe Moges N
Received 22 August 2022
Accepted for publication 12 May 2023
Published 5 June 2023 Volume 2023:15 Pages 279—291
DOI https://doi.org/10.2147/HIV.S385526
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Baleh Nibret Eskezia,1 Yilkal Tafere,2 Abiot Aschale,2 Nurilign Abebe Moges2
1Debre Markos Comprehensive Specialized Hospital, Debre Markos, Ethiopia; 2Department of Public Health College of Health Sciences, Debre Markos University, Debre Markos, Ethiopia
Correspondence: Abiot Aschale, Email [email protected]
Background: Human immunodeficiency virus self-testing (HIVST) is universally accepted as an HIV testing option to achieve the United Nations Agency for International Development first 95 goal by 2030. HIV testing coverage through voluntary counseling and testing and provider initiated testing and counseling is low among female sex workers (FSWs). However, there is no evidence on the level of HIVST among FSWs in the study area.
Objective: To assess the uptake of HIVST and associated factors among FSWs at non-governmental facilities in Debre Markos and Bahir Dar towns, Northwest Ethiopia, 2022.
Methods: An institution-based cross-sectional study design was employed. A total of 423 study participants were selected by systematic random sampling technique. The data were collected using a structured and pre-tested questionnaire; entered into EpiData version 3.1 and exported to SPSS version 25 for analysis. An adjusted odds ratio (AOR) with a 95% confidence interval (CI) was estimated to assess the strength of association between independent variables and dependent variable. Bivariable logistic regression was done for each variable and those with a P-value of < 0.25% were selected for multivariable analysis. Finally, P-value < 0.05% was declared statistically significant.
Results: The magnitude of HIVST uptake among FSWs was 59.3%. Time since engagement of sex work > 5 years [AOR 2.16 (95% CI: 1.158– 4.013)], age of first sexual debut > 19 years [AOR 3.23 (95% CI: 2.045– 5.093)], previous urban residence [AOR 3.99 (95% CI: 2.58– 6.18)], good knowledge towards HIVST [AOR 1.78 (95% CI: 1.066– 2.964)], education status being college and above [AOR 5.6 (95% CI: 3.12– 9.30)] were significantly associated factors.
Conclusion: HIVST uptake among FSWs was 59.3% which is lower than expected at national level. Educational status, age at first sexual debut, knowledge towards HIVST, and time since engagement in sex work were significantly associated with HIVST uptake.
Keywords: HIV self-testing, female sex worker, Ethiopia
Introduction
Human immunodeficiency virus self-testing (HIVST) is a process in which a person performs a rapid HIV test and interprets the result in a private setting. It is focused on high-risk populations to increase uptake and frequency of testing.1 Increasing coverage of HIV testing, early detection of HIV and initiation of antiretroviral therapy (ART) significantly reduces HIV morbidity and mortality and improves the quality of life for people living with HIV while reducing the risk of HIV transmission.2–4 Similarly, awareness of one’s negative HIV serostatus is important for prioritizing prevention strategies, especially in the context of increasing availability of pre-exposure prophylaxis (PrEP).5,6
The World Health Organization (WHO) recommends frequent HIV testing in female sex workers (FSWs) to increase engagement of HIV prevention services and reduce the risk of transmission.1 HIV self-testing is universally accepted as an innovative strategy complementing existing HIV testing services to achieve the UNAIDS 95-95-95 goals by 2030.5 HIV self-testing can potentially overcome barriers to HIV testing uptake and accessibility by testing on the individual, increasing confidentiality and allowing members of marginalized and stigmatized groups to test in settings of privacy, safety, and dignity.7
Increasing uptake of HIVST is critical to reducing the incidence of HIV and improving access to treatment and support for seropositive people. Those who know their seropositive status are less likely to engage in sexually risky behavior, which helps reduce the risk of HIV transmission.1,8 HIVST is universally accepted as an emerging tool to increase the uptake of HIV testing in high-risk populations.8 Many countries globally have policies supporting HIVST among key populations, which could decentralize and increase the frequency of HIV testing and create an alternative service delivery model.1,7
Globally, HIV prevalence among FSWs is 26 times greater than the general population.9 Their vulnerability is increased due to the high likelihood of being economically vulnerable, unable to negotiate consistent condom use, experiencing violence, criminalization, marginalization, socio-cultural, legal, and other factors that adversely affect their capacity to protect themselves from the risk of HIV infection.5,10 The prevalence of HIV among FSW in Ethiopia was 10%.11 Globally, 25% of people living with HIV (PLHIV) have yet to be diagnosed and this figure is 21% in Ethiopia.11,12 Due to the nature of their work, infected FSWs have a higher risk of spreading HIV among the population along with other STIs.12 Female sex workers were not as receptive to utilizing public facilities for HIV testing.10
The underperformance of HIV counseling and testing is a significant barrier to HIV prevention and care among FSWs.13 Therefore, HIVST is universally accepted as it would help to increase enrolment of female sex workers for HIV prevention, treatment, and care by complementing the existing strategy.1 In Ethiopia, HIV counseling and testing (VCT) and provider-initiated testing and counseling (PITC) were the primary means of providing HIV testing.14
There is a major gap between voluntary HIV testing coverage and what is required. Interventions aiming to increase uptake of HIV testing in sex workers include providing outreach services, peer education, availability of clinical services, building the capacity of health facilities with necessary resources, such as HIV test kits and STI treatment, and involvement of private sectors.1,15 To increase uptake to HIVST, a new self-testing strategy is currently being implemented,1 but the uptake of self-testing for HIV and the factors associated with it is understudied in Ethiopia. Therefore, this study was undertaken to determine the uptake and associated factors of HIVST and to recommend expanding HIVST as a complementary testing option.
As far as the authors searched, there was no adequate globally estimated figure for HIV self-testing among FSWs. According to Ethiopian epidemiological data, limited targeting intervention for FSW, including access to HIV-related information, was reported.16 A study conducted by USAID in Ethiopia showed only 42% of FSWs were accessed by the program, which implies the continued existence of unaddressed interventions for FSWs, including HIV testing and counseling.17
The magnitude of uptake of HIVST among FSWs in Nigeria, Senegal, and Malawi showed 70.4%,18 74.5%,2 and 76.5%,3 respectively and a study done in South Africa revealed that HIVST uptake was 64.5%.19 In Tanzania self-testing uptake was 62.7%.5
Justification of the Study
Even though Ethiopia is working to reduce new HIV infections in accordance with the worldwide vision to end AIDS by 203020 and the general public has improved HIV screening status, with a potential drop in HIV prevalence, female sex workers’ requirements, such as HIV testing and other intervention strategies, have not been well addressed.21 Female sex workers refused to test for HIV in public facilities.10 As a result, HIV self-testing complemented the existing policy by helping to boost the enrolment of female sexual workers in HIV prevention, treatment, and care.1 It makes a greater contribution to the UNAIDS testing aim of reaching the first 95% to complement and accelerate universal access to HIV prevention, treatment, and care. The commonest rationales for using HIV self-testing as a testing option were that it decreased stigma and discrimination and promoted autonomy and confidentiality better than facility testing done by health-care providers. The barriers for not testing were lack of knowledge, economic constraints, perception of inaccurate test results, and lack of pre- and post-test counseling.5
The uptake of HIVST among FSWs in Ethiopia is unclear. As a result, the goal of this study is to assess HIVST uptake and identify associated factors among FSWs in non-governmental HIV testing and counseling facilities in the towns of Debre Markos and Bahir Dar.
Conceptual Framework
The conceptual framework utilized in this study supports a literature review that specifies the contribution of multiple factors of uptake of HIV self-testing (Figure 1).
 |
Figure 1 A conceptual framework that is adapted from a literature review on uptake of HIV self-testing and associated factors among female sex workers in Debre Markos and Bahir Dar towns, 2021.5,13,18,22 |
Methods and Materials
Study Area and Period
The research was carried out at non-governmental facilities in the towns of Debre Markos and Bahir Dar. Debre Markos is located in the Amhara Regional State’s East Gojjam zone, 299 kilometers north of Addis Ababa, while Bahir Dar is the capital of the Amhara National Regional State, 564 kilometers north of Addis Ababa. According to reports from the towns of Debre Markos and Bahir Dar in 2021, the total population of Debre Markos was 138,996, with 74,224 females, while the entire population of Bahir Dar was around 339,683, with 166,445 females. Mapping was used to identify hotspot areas for FSWs, and 1056 FSWs visited in the recent two months at both Debre Markos and Bahir Dar non-governmental facilities (drop-in centers). Drop -in centers are safe places in which FSWs get HIVST services in Debre Markos and Bahir Dar towns.
This study was conducted from December 1, 2021 to January 30, 2022.
Study Design
An institutional-based cross-sectional study design was employed.
Population
Source Population
All FSWs in Debre Markos and Bahir Dar Towns.
Study Population
All females who self-identify as sex workers and have received HIV counseling in Debre Markos and Bahir Dar non-governmental facilities in the previous three months.
Eligibility Criteria
Inclusion Criteria
Female sex workers who identified as sex workers who are 18 years and older who attend the drop in centers during the study period.
Exclusion Criteria
Female sex workers who are not registered in the Drop in Centers (temporary visitors) were excluded.
Sample Size Determination
Since there s no previous study on HIV self-testing among FSWs in Ethiopia, the sample size was determined by a single population proportion formula using a 50% proportion of uptake of HIV self-testing with 5% level of precision and 95% confidence interval (CI).
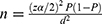 = (1.96)2 (0.5)(0.5)/(0.05)(0.05) =384
= (1.96)2 (0.5)(0.5)/(0.05)(0.05) =384
Where, n= required sample size
Zα/2 critical value for normal distribution at 95% CI which equals
1.96 (Z value at alpha = 0.05)
Marginal error = 0.05
q = 1-p =0.5
p- The proportion of uptake of HIV-self testing 50%
Then by adding 10% non-respondents which is 38.416=39
The total sample size was 423.
Sampling Procedure
The sample was taken from a non-governmental health -care facility’s registration book using a systematic random sampling technique (network of charitable association of HIV -positive people for health and development). A total of 1056 FSWs visited one of the non-governmental health facilities in the last two months. A total of 300 FSWs from Debre Markos and 750 FSWs from Bahir Dar.
Based on this, a total of 423 FSWs were chosen after determining the sampling interval from each facility (k=N/n).
The sample from facility (F1)= n1=N1(n/N)
n1=sample from facility (X)
N1=population from facility X
n= Total sample
N1= Total population (sex worker)
Sample from Debre Markos Facility (n1)= 306(423/1056)
Total sample from DM = 123
Therefore K1= N/n for facility (1)≤306/123=K=2
From Debre Markos facility 123 sample was drawn every 2 interval.
Sample from Bahir Dar Facility2 (n2)=750(423/1056)
K2= N/n, Total sample from BDR =300
For facility (2) (Bahir Dar) ≤750/300= k=2
From Bahir Dar facility 300 sample was drawn every 2 interval (as shown in Table 1).
 |
Table 1 Sample Size Calculation for Assessment of Uptake of HIV Self-Testing and Associated Factors Among Female Sex Workers in Debre Markos and Bahir Dar Towns, Northwest Ethiopia, 2022 |
From Table 1 the maximum sample size with 10% non-response rate was 313. Therefore, the largest optimal sample size was 423 for this study.
Study Variables
Dependent variable: HIV self-testing uptake
Independent variables: Socio-demographic factors including age, educational status, religion, previous occupation, previous residence and living arrangement and Behavioral factors including alcohol use, drug use, condom use, chat chewing, number of clients engaged last week, time since engagement in sex, Perceived risk of HIV infection and age of first sexual debut, and Knowledge towards HIV self-testing, Knowledge towards PrEP were independent variables.
Operational Definitions
Alcohol use: use of any amount and any type of alcohol at least once during the last 3 months.24,25
Khat chewer: an individual is considered as a chewer if she had chewed at least once in the last 3 months.26
Knowledgeable towards HIV self-testing:- Each correct response scored 1 point and each incorrect and non-response scored 0 points. The overall score ranged from a minimum of 0 to a maximum of 10. Those who had a mean score of 5 points and above were categorized as having a high level of knowledge and those who had a mean score of below 5 were categorized as having a low level of knowledge.27
Data Collection Procedure and Instrument
Data Collection Instrument
An Amharic version of a structured questionnaire was used to collect data. The questionnaires were written in English first, then translated into Amharic. The questionnaire was accompanied by socio-demographic and behavioral parameters, as well as HIV self-test related knowledge and perceptions. Uptake of HIV self-testing is confirmed if female sex workers test on their own or with the help of peers and report to the facility, which is referred to as uptake of HIV self-testing.
Data Collection Procedure
Two public health supervisors and four clinical nurses were recruited for this study and given two days of training on the study objectives, relevance, informed consent and information confidentiality, respondent rights and interview technique. A non-governmental health institution in Finote Selam town was used to pre-test the questionnaire on 5% of the overall sample size. Face-to-face interviews with each respondent was used to collect data.
Data Quality Control
Pre-tested questionnaires were used to collect data by well-trained data collectors. Data were reviewed for completeness and internal consistency on a daily basis by supervisors and the primary investigator. The data were then double-checked for completeness before being entered for analysis. They were then entered into EpiData 3.1 and exported to SPSS.
Data Processing and Analysis
Data were entered into EpiData version 3.1 before being exported to the Statistical Package for Social Science (SPSS) version 25 software for further processing and analysis. Text descriptions and tables were used to describe the relevant findings of the study. Bivariable logistic regression was used to select the candidate variable for multi-variable logistic regression analysis. Those independent variables with a p-value of 0.25 or less in the bivariable logistic regression were included in the multi-variable logistic regression to get the adjusted effect of each covariate. An adjusted odds ratio (AOR) with a 95% CI was estimated to assess the strength of the association between the independent variables and the dependent variable. Variables with a p-value less than 0.05 in the multi-variable logistic regression analysis were considered statistically significant and independent predictors of HIV self-testing uptake. In final multivariable models, the level of multicollinearity were checked and fitted using the variance inflation factor.
Ethical Considerations
Ethical approval was received from the Debre Markos University, health science college institutional research ethics review committee with ethical letter number HSC/R/C/Ser/PG/Co/46/11/14 and then this written letter was given to the women, youth, and children affairs offices in Bahir Dar and Debre Markos to secure their consent. Each participant who were 18 years old and older, gave their informed consent after clearly presenting the study’s objectives, benefit, and risk, as well as their right to decide whether or not to participate in the study. Written informed consent was obtained. The study participants were volunteers and informed in the research based on the Declaration of Helsinki.
For the sake of confidentiality, their names have been omitted. The respondents were interviewed in a secure place.
Results
Socio-Demographic Characteristics
The details of socio-demographic characteristics of respondents is shown in Table 2. A total of 423 respondents participated in the study with response rate was 100%. From the total, 235 (55.6%) of female sexual workers were aged 25–30 years, while 103 (24.3%) were aged 18–24 years.
 |
Table 2 Socio-Demographic Characteristics of Female Sex Workers at Non-Governmental Health-Care Facilities in Debre Markos and Bahir Dar Towns, Ethiopia, 2022 |
Knowledge Characteristics
In terms of HIV self-testing, 244 (57.7%) of the respondents are knowledgeable, while 179 (42.3%) are not. Similarly, 219 (51.8%) of the respondents are knowledgeable about pre-exposure prophylaxis, while 204 (48.2%) are not.
Behavioral Characteristics
Regarding to first sexual debut 264 (62.4%) FSWs had first sexual encounter when they were 19 years old or above, whereas 159 (37.6%) had their first sexual encounter when they were 18 years old or younger.
The number of sexual clients for 169 (40%) FSWs at last week was only one, and 76 (18%) FSWs had three or more sexual clients. In addition, 64 (15.1%) FSWs used alcohol and 359 (84.9%) did not use alcohol.
From the total, 109 (25.8%) female sex workers used drugs; and 70 (16.5%) of female sex workers had sexual intercourse after drug use. More than half, 271 (64.1%) FSWs have positive perceptions towards risk of HIV infections, but,152 (35.9%) FSWs have negative perceptions (Table 3).
 |
Table 3 Behavioral Characteristics of Female Sex Workers at Non-Governmental Health-Care Facilities in Debre Markos and Bahir Dar Towns, Ethiopia, 2022 |
Uptake of HIV Self-Testing
This study showed that the magnitude of HIV self-testing uptake was 251 (59.3%; CI: 54.3–63.9%.
Bivariable and Multivariable Regression Analysis
In the bivariable logistic regression analysis, previous resident, educational status, previous occupation, knowledge towards HIV-self testing, knowledge to pre-exposure prophylaxis, time since engagement in sex work, perception of risk of HIV infection, khat chewing, drug use, living arrangement, age of first sexual debut, time since engagement in sex work, and number of clients engaged last week were selected in bivariable with P ≤ 0.25 cut-off point (Table 4).
 |
Table 4 Bi- Variable Logistic Regression Analysis Result, of Factors Associated with Uptake of HIV Self-Testing at Debre Markos and Bahir Dar Towns, Among Female Sex Workers, 2022 (N=423) |
In the final model, knowledge towards HIVST, perception of risk of HIV infection, previous resident, educational status, time since engagement in sex work and age of first sexual debut were identified as associated factors with HIVST uptake.
FSWs who had their first sexual encounter at the age of 19 years or above are three times more likely to uptake HIVST [AOR 3.23 (95% CI: 2.05–5.09)] than 18 years or lower.
FSWs with previous urban origin were four times more likely to uptake HIVST than those who had lived in rural areas [AOR 3.95 (95% CI: 2.9–6.2)]. Those who have good knowledge of HIVST were nearly two times more likely to uptake HIVST [AOR 1.78 (95% CI: 1.07–2.96)] than those who have poor knowledge. FSWs with a college and above education level are more than five times to uptake HIVST [AOR 5.6 (95% CI, 3.12, 9.30)] than those with a lower education level.
FSWs who were engaged as a sexual worker five years and above were more than two-fold times more likely to uptake HIVST [AOR 2.16 (95% CI: 1.16, 4.01)] when compared with less than five years. FSWs with good perception to risk of HIV infection were more than three-fold times more likely to be tested than those with poor perceptions [AOR 3.34 (95% CI: 2.18–4.96)] (Table 5).
Discussion
This study showed that the magnitude of HIVST among FSW was 59.3% with CI 54.3–63.9%. This is lower than some other studies conducted in Africa(70.4% in Nigeria,18 74.5% in Senegal,2 76.5% in Malawi3 and 64.5% in South Africa).19 HIVST uptake among FSW is considerably lower than the national requirement that was planned to be 95% based on UNAIDS 95-95-95 goals.5 Furthermore, the result is consistent with a study conducted in Tanzania, which was 62.7%.3,4 The difference might be due to variation in study area and population characteristics. Duration of engagement on sex work for five years or more has been positively associated with HIVST uptake which is comparable with a study conducted in Addis Ababa on HIV testing uptake among female sex workers.11 The possible explanation may that the duration of time of sexual involvement increased the opportunity to access of HIV prevention methods and risk perception increased.11
Female sex workers with age of first sexual encounter at 19 years old and above had three times higher HIVST uptake as compared with 18 years old and below. Similarly, a study conducted in Tanzania showed that FSWs with a first sexual encounter at below 18 years old were less likely associated with HIVST as compared with those who had a sexual encounter at 19 years and older.5 This is consistent with a study conducted in Gambia. The possible reasons might be older adults are more knowledgeable on HIV issues, high HIV testing service exposure and autonomous in decision making than youths.5,28
Those who had good knowledge towards HIVST were nearly two times as likely to use HIV self-testing. A study conducted in Rwanda showed that good knowledge towards HIVST was three times as likely to have HIVST uptake. The possible reason for this may be due to more clients are at high education level which resulted in better health-seeking behavior.29,30
Regarding to Perception of risk of HIV infection, FSWs with good perception towards risk of HIV infection were three times as likely to uptake HIV self-testing as compared with those who have poor perception and this showed that good risk perception towards HIV/AIDS helped to improve HIVST uptake. Similarly, another study in Singapore showed that those who had good perception of risk of HIV infection were more likely to uptake HIVST as compared with poor perception of risk of HIV infection.31
This study showed that those who had college and above educational level were more than five-fold times more likely to self-test for HIV as compared with secondary and below level of education. Similar studies in Kenya,32 Malawi3 and China23 on HIV self-testing uptake showed that the more educated respondents were more likely to be tested than less/non educated. Additionally, a study in Thailand revealed that those with a secondary certificate or higher education level were more likely to be aware and to self-test for HIV than those with less or no education. The possible reason for this might be that when the level of education increased, level of perception about HIVST, and willingness to be tested for HIV by self increased.14,18,33
Previous urban residents were positively associated with HIVST uptake. A study carried out in Zimbabwe revealed that urban residents had positive associations with HIV self-testing uptake.14 The possible reason might be that urban residents have easy access to information about HIVST and havie more self-confidence than rural residents.
Strength
This study tried to assess HIV self-testing uptake among female sex workers using strong methods for recruitment, a relatively large sample size of a population that’s hard to reach, and a rich survey dataset.
Limitation
Due to the nature of the data, clients might be subjected to recall bias. The study design was cross-sectional that is purely quantitative. It is better to be conducted with a mixed study design. This study was conducted in only two non-governmental institutions in Debre Markos and Bahir Dar towns. This means the study findings cannot be generalized to other parts of the country.
Conclusion
In this study, HIVST uptake among FSWs is considerably lower than the national requirement that was planned to be 95% based on UNAIDS 95-95-95 goals.
Educational status, age at first sexual debut, knowledge towards HIVST, perception of risk of HIV infection, previous resident, time since engagement in sex work were significantly associated factors of HIVST uptake.
Recommendation
Health Care Workers should prepare fear appeal messages regarding HIV and distribute for FSWs with poor risk perceptions to HIV/AIDS. Other methods also need to be used to increase knowledge of FSWs about HIVST uptake. Researchers should do further qualitative studies because the nature of the research title requires qualitative data that cannot be addressed by only quantitative study.
Abbreviations
ART, Anti-Retroviral Therapy; DC, Data Collector; DIC, Drop in Centre; EDHS, Ethiopian Demographic Health Survey; EPHIA, Ethiopian Population based HIV Impact Assessment; ERC, Ethical Review Committee; FSW, Female Sexual Worker; HCT, HIV Counseling and Testing; HIV, Human Immunodeficiency Virus; HIVST, Human Immunodeficiency Virus Self-Testing; HTS, HIV Testing Service; PrEP, Pre-Exposure Prophylaxis; STI, Sexual Transmitted Infection; UNFPA, United Nations Population Fund survey; UNAIDS, United Nations Agency for International Development; WHO, World Health Organization.
Acknowledgments
The authors would like to thank the study participants and data collectors for making the research possible by participating in the research and their commitment in the process of data collection. Finally the authors would like to express their gratitude to Debre Markos University for providing the opportunity to perform this research.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. WHO. HIV Self-Testing and Partner Notification; 2016.
2. Lyons CE, Coly K, Bowring AL, et al. Use and acceptability of HIV self-testing among first-time testers at risk for HIV in Senegal. AIDS and Behavior. 2019;23(2):130–141. doi:10.1007/s10461-019-02552-2
3. Johnson C, Neuman M, MacPherson P, et al. Use and awareness of and willingness to self-test for HIV: an analysis of cross-sectional population-based surveys in Malawi and Zimbabwe. BMC. 2020;20:1–13.
4. Martinez Perez G, Steele SJ, Govender I, et al. Supervised oral HIV self-testing is accurate in rural KwaZulu-Natal, South Africa. Trop Med Int Health. 2016;21(6):759–767. doi:10.1111/tmi.12703
5. Vara PA, Buhulula LS, Mohammed FA, Njau BJAR. Therapy. Level of knowledge, acceptability, and willingness to use oral fluid HIV self-testing among medical students in Kilimanjaro region, Tanzania: a descriptive cross-sectional study. BMC. 2020;17(1):1–10.
6. Tonen-Wolyec S, Batina-Agasa S, Muwonga J, Mboumba Bouassa R-S, Kayembe Tshilumba C, Bélec L. Acceptability, feasibility, and individual preferences of blood-based HIV self-testing in a population-based sample of adolescents in Kisangani, Democratic Republic of the Congo. PLoS One. 2019;14(7):e0218795. doi:10.1371/journal.pone.0218795
7. Chanda MM, Ortblad KF, Mwale M, et al. HIV self-testing among female sex workers in Zambia: a cluster randomized controlled trial. PLoS Med. 2017;14(11):e1002442. doi:10.1371/journal.pmed.1002442
8. Council A, Espinoza Castro VM, Abiad A. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV. The Journal of Organic Chemistry. 2021;86(1):693–708. doi:10.1021/acs.joc.0c02318
9. UNAIDS. Global HIV Statistics Fact Sheet, 2021; 2021.
10. Damtew M. Factors Influencing The Uptake Of HIV Services By Female Sex Workers In Ethiopia. BMC. 2017;1:453.
11. Lisecki SR, Solomon S, Kassa G, King EJ; Lisecki SR, Solomon S, Kassa G, King EJ. Factors associated with recent HIV testing uptake and HIV-positive serostatus among female sex workers in Addis Ababa, Ethiopia. Glob Public Health. 2022;17(3):431–443. doi:10.1080/17441692.2020.1868015
12. Staveteig S, Croft TN, Kampa KT, Head SKJ. Reaching the ‘first 90’: gaps in coverage of HIV testing among people living with HIV in 16 African countries. PLoS One. 2017;12(10):e0186316. doi:10.1371/journal.pone.0186316
13. Shava E, Manyake K, Mdluli C, et al. Acceptability of oral HIV self-testing among female sex workers in Gaborone. Botswana. 2020;15(7):e0236052.
14. Federal HIV/AIDS Prevention and Control Office FMoH. Guidelines for HIV Counselling and Testing in Ethiopia. Adis Ababa; 2007.
15. Federal HIV/AIDS Prevention and Control Office FMoH. HIV Prevention in Ethiopia National Road Map 2018-2020 FINAL_FINAL.pdf; 2018.
16. FHAPCO FHAPaCO. HIV/AIDS in Ethiopia, AN EPIDEMIOLOGICAL SYNTHESIS; 2014.
17. Overs C. Sex Workers, Empowerment and Poverty Alleviation in Ethiopia. IDS; 2014.
18. Iliyasu Z, Kassim RB, Iliyasu BZ, et al. Acceptability and correlates of HIV self-testing among university students in northern Nigeria. International Journal of STD & AIDS. 2020;31(9):820–831. doi:10.1177/0956462420920136
19. Kitenge MK, Laxmeshwar C, Bermudez Aza E, et al. Acceptability of unsupervised peer-based distribution of HIV oral self-testing for the hard-to-reach in rural KwaZulu Natal, South Africa: results from a demonstration study. PLoS One. 2022;17(3):e0264442. doi:10.1371/journal.pone.0264442
20. Sidibé M. Fast-Tracking the response to end the AIDS epidemic by 2030. 2014.
21. World Health Organization. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Recommendations for a Public Health Approach. World Health Organization; 2016.
22. Ortblad KF, Musoke DK, Ngabirano T, et al. HIV self-test performance among female sex workers in Kampala. Uganda. 2018;8(11):e022652.
23. Wang C, Tucker JD, Tucker JD, et al. Correlates of HIV self-testing among female sex workers in China: implications for expanding HIV screening. Journal of Metabolic and Bariatric Surgery. 2020;9(1):1–9. doi:10.17476/jmbs.2020.9.1.1
24. Bradley KA, Bush KR, Epler AJ, et al. Two Brief Alcohol-Screening Tests From the Alcohol Use Disorders Identification Test (AUDIT): validation in a Female Veterans Affairs Patient Population. Arch Intern Med. 2003;163(7):821–829. doi:10.1001/archinte.163.7.821
25. López MB, Lichtenberger A, Conde K, Cremonte M. Psychometric Properties of Brief Screening Tests for Alcohol Use Disorders during Pregnancy in Argentina. Revista brasileira de ginecologia e obstetricia. 2017;39(7):322–329. doi:10.1055/s-0037-1603744
26. Abate A, Tareke M, Tirfie M, Semachew A, Amare D, Ayalew E. Chewing khat and risky sexual behavior among residents of Bahir Dar City administration, Northwest Ethiopia. Ann Gen Psychiatry. 2018;17(1):26. doi:10.1186/s12991-018-0194-2
27. Vara PA, Buhulula LS, Mohammed FA, Njau B. Level of knowledge, acceptability, and willingness to use oral fluid HIV self-testing among medical students in Kilimanjaro region, Tanzania: a descriptive cross-sectional study. AIDS Res Ther. 2020;17(1):56. doi:10.1186/s12981-020-00311-1
28. Lisecki SR, Solomon S, Kassa G, King E. Factors associated with recent HIV testing uptake and HIV-positive serostatus among female sex workers in Addis Ababa, Ethiopia. Global Public Health. 2020;1:431.
29. a TD. HIV self-testing in Rwanda awareness and acceptability among male clinic.pdf. Heliyon. 2017;6(3):e035.
30. Volk JE, Lippman SA, Grinsztejn B, et al. Acceptability and feasibility of HIV self-testing among men who have sex with men in Peru and Brazil. International Journal of STD & AIDS. 2016;27(7):531–536. doi:10.1177/0956462415586676
31. Tan Y-R, Kaur N, Ye AJ, et al. Perceptions of an HIV self-testing intervention and its potential role in addressing the barriers to HIV testing among at-risk heterosexual men: a qualitative analysis. Sex Transm Infect. 2021;97(7):514–520. doi:10.1136/sextrans-2020-054773
32. Kelvin EA, George G, Mwai E, et al. A randomized controlled trial to increase HIV testing demand among female sex workers in Kenya through announcing the availability of HIV self-testing via text message. AIDS and Behavior. 2019;23(1):116–125. doi:10.1007/s10461-018-2248-5
33. Shafik N, Deeb S, Srithanaviboonchai K. Awareness and Attitudes Toward HIV Self-Testing in Northern Thailand. Lancent. 2021;18(3):852. doi:10.3390/ijerph18030852
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

