Back to Journals » International Medical Case Reports Journal » Volume 13
Unusual Missed Diagnosis of Foreign Body: A Case Report
Authors Chowdhary S, Garg P, Sawhney V , Pandya A, Sambhav K, Gupta S
Received 22 January 2020
Accepted for publication 8 April 2020
Published 19 May 2020 Volume 2020:13 Pages 187—190
DOI https://doi.org/10.2147/IMCRJ.S246924
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Somya Chowdhary,1 Pooja Garg,2 Vivek Sawhney,2 Abhijit Pandya,2 Kumar Sambhav,3 Shailesh Gupta2
1Bascom Palmer Eye Institute, University of Miami, Miami, FL, USA; 2Specialty Retina Centre, Coral Springs, FL, USA; 3Department of Ophthalmology, University of Florida, Jacksonville, FL, USA
Correspondence: Shailesh Gupta
Specialty Retina Centre, Coral Springs, FL 33067, USA
Tel +1561 322-3588
Email [email protected]
Background: Penetrating intraorbital foreign body (IOFB) is usually associated with high-velocity trauma forces around the eye. IOFB injury to globe or optic nerve is considered a surgical emergency; an immediate diagnosis and management plan is generally indicated.
Methods: A case report (design). The patient was a 78-year-old male presented with diminution of vision of the right eye following a high-velocity injury. The patient was noted to have a closed globe injury with associated retinal detachment and vitreous hemorrhage. An initial orbital CT scan did not reveal any IOFB, despite and intact globe. However, repeat a CT head and orbit scan revealed an intracranial magnetic foreign body lodged in the right frontal lobe.
Conclusion: A CT scan of the brain and paranasal sinuses should be obtained along with a CT orbit in case of high-velocity orbital/ocular trauma.
Keywords: intraorbital foreign body, IOFB, intracranial foreign body, CT scan, retinal detachment
Introduction
Penetrating intraorbital foreign body (IOFB) is a rare cause of ocular or cranial trauma. It commonly occurs among young people and is usually associated with high-velocity trauma forces around the eye, such as occupational injuries and simpler injuries like daily household chores and gunshot wounds.1 An IOFB injury to the globe or optic nerve, is considered a surgical emergency, and an immediate diagnosis and management plan is generally indicated.2 Reliable imaging information is necessary to preoperatively plan the reconstruction of functional areas, and future rehabilitation. A computed tomography (CT) scan is considered the gold standard in imaging modality for metallic foreign bodies.3 However, CT findings can vary. It is imperative to maintain a high index of suspicion in to avoid misdiagnosis.3 To avoid missing the diagnosis, careful evaluation and detailed imaging of the globe and surrounding structures, including the brain and paranasal sinuses, is indicated.
We present a rare case of household orbital trauma with a large IOFB which led to marked visual impairment, despite an intact globe. What added to the value of this case was an unusual normal orbital CT scan that initially misled the physicians.
Methods
Case Report
Written informed consent was provided by the patient to have the case details and any accompanying images published. Institutional approval was not required to publish the case details. The patient was a 78-year-old African-American male who presented with diminution of vision of the right eye over the previous 24 hours. He stated that something went into his right eye while he was mowing the lawn. He was alert and neurologically intact. The signs of traumatic right eye injury was bullous sub-conjunctival hemorrhage and lid edema on the medial aspect of upper lid. He was a known diabetic and hypertensive. On examination, his visual acuity was hand movements in the right eye and 20/30 in left eye (best corrected visual acuity). He was found to have relative afferent pupillary defect (RAPD) in the right eye. There was no restriction of extraocular movements in both eyes. Slit lamp evaluation showed a bullous sub-conjunctival hemorrhage in the right eye, the posterior limit of which could not be defined. The cornea was clear in both eyes with an intact anterior chamber and no evidence of inflammation. There were cortical cataracts of both eyes. Intraocular pressure on applanation tonometer was 14 and 18 mm Hg in the right and left eye respectively. There was no view of a right eye fundus examination. The left eye fundus examination revealed mild non-proliferative diabetic retinopathy changes with grade I hypertensive retinopathy and trace epiretinal membrane.
A B-scan ultrasound evaluation of the right eye revealed vitreous hemorrhage, macula off retinal detachment without any evidence of an intraocular foreign body or traction on retina. No retinal break was appreciated on the B scan. A spectral domain optical coherence tomography (SD-OCT) was not possible in the right eye and in the left eye old focal laser scars, infero-nasal retinal folds and an epiretinal membrane were noted. A review of systems was normal without any evidence of a focal neurological deficit.
An orbital CT scan done prior to the visit to our facility, in an outside emergency facility revealed no intraocular/intraorbital foreign body, no disruption of the orbital wall but vitreous hemorrhage in the right eye (Figure 1A–C).
Based on our initial evaluation and radiological results blunt ocular trauma was thought to be responsible for such a presentation. The patient was informed of their condition and the need for globe exploration and the possible need of repair of retinal detachment. The patient agreed to the surgery and emergency surgery was performed after the appropriate consent was obtained. The patient underwent globe exploration with pars plana vitrectomy for the repair of a retinal detachment, along with endolaser and silicon oil infusion. During the globe exploration there was no evidence of any intraocular/intraorbital foreign body or globe dehiscence, but a small graze wound to the nasal side of the globe was present. This led the clinician to investigate further.
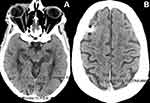
The history of a high-velocity injury, the presence of a bulbar conjunctival hemorrhage without the posterior defined limit, and the intra-operative graze wound on the nasal side of the globe led the clinician to re-investigate the neuroimaging to be able to understand the exact etiology of the subject’s vitreous hemorrhage and retinal detachment. A repeat orbital CT scan along with a CT scan of the brain and sinuses was obtained (Figure 2A and B). To our surprise an intracranial magnetic foreign body lodged in the right frontal lobe was noted. The patient was referred for an emergency neurosurgical evaluation, and he underwent urgent neurosurgical intervention for the removal of the intracranial foreign body.
It appears that a magnetic foreign body must have entered the right nasal orbit outside the muscle cone while the paient was mowing the lawn and it traversed to the frontal lobe where it became lodged. The foreign body was initially missed on the orbital CT scan done in the outside facility.
Discussion
The clinical manifestation, management, and outcomes of orbital foreign bodies vary based on the material of the foreign body.4 Orbital traumas that are associated with direct or indirect optic nerve injury should be considered a surgical emergency. In such cases, early removal of the foreign body is indicated, so high clinical suspicion, cautious physical examination, choosing suitable imaging modalities and protocols are essential to prevent misdiagnosis.5 A proper radiological assessment of such cases may sometimes be challenging to the radiologist and the clinician.
Of all the ocular injuries, intra-orbital foreign bodies may be present in 10–17% of cases.6 Magnetic Resonance Imaging (MRI) is contraindicated for an initial evaluation when intraorbital/intraocular metallic foreign bodies are suspected and ultrasonography B scan is not indicated in cases of globe rupture. A radiographic X-ray examination would have very low sensitivity for soft tissue injuries to orbital contents, so is rarely done now.
CT imaging is the diagnostic tool of choice for initial evaluation of cases with ocular/orbital trauma as its sensitivity in detecting foreign bodies has been reported to be around 100%.7 A CT scan also help in excluding the orbito-cranial extension, and diagnosing orbital wall fractures.
Though CT scan is the imaging modality of choice, there are certain guidelines for the initial CT scan which should be followed in complex traumatic scenarios otherwise significant findings (like intracranial foreign body) would be missed. CT protocols can vary among institutions but certain basic imaging guidelines have been proposed. For orbital injuries, optimal protocol is a thin sliced CT scan with 1–2 mm cut though the orbit, performed with a helical CT. It has been found to be accurate for detection and localization of orbital metallic, glass and stone foreign bodies and can be used in guiding surgical management of these cases.8 Alternatively, a thin-section axial CT scan (0.625–1.25mm) of the orbit can be done with a multiplanar reformation.9 Some have proposed the use of a helical CT scan from frontal to the maxillary sinuses: 120 kVp, 100 mAs, 1.25 section thickness with 1.25 intervals and a pitch of 0.969, with image reconstruction in axial and coronal planes,10 while others have advocated the use of a multi-detector CT in the management of uncertain open globe injuries.11
Our case demonstrates that despite prompt radiological imaging and intervention, an IOFB was missed. It was only the high index of clinical suspicion which prompted ar repeat, extended imaging protocol which comprised of a CT scan of the brain, orbit, and paranasal sinuses. It revealed a metallic foreign body in the right frontal lobe. On presentation the patient's right eye was closed, with a globe injury with retinal detachment, vitreous hemorrhage and RAPD. This can happen due to the sheer velocity of the injury. After ocular and neuro-surgical intervention the patient had a good final outcome.
In conclusion, this case emphasizes the need to rely on the history, clinical presentation, and review of CT scan sections by the ophthalmologist with a multi-disciplinary approach. A CT scan of the orbit should be obtained, along with brain and paranasal sinuses, in cases of high-velocity orbital/ocular trauma.
Acknowledgments
No author received financial or material support for the research and the work. No author has financial or proprietary interest related to the research.
Disclosure
The authors declare no conflicts of interest.
References
1. Turliuc DM, Costan V, Cucu A, Costea CF. Intraorbital foreign body. Med Surg J. 2015;119(1):179–184.
2. Türkçuoğlu P, Aydoğan S. Intracranial foreign body in a globe-perforating injury. Can J Ophthalmol. 2006;41(4):504–505. doi:10.1016/S0008-4182(06)80017-7
3. Zhou DD, Niu K, Lu CW, Hao JL, Zhang BJ, Hui P. Missed diagnosis of an intraorbital foreign body of homemade fireworks origin: a case report. Case Rep Ophthalmol. 2015;6(3):448–452. doi:10.1159/000442584
4. Fulcher TP, McNab AA, Sullivan TJ. Clinical features and management of intraorbital foreign bodies. Ophthalmology. 2002;109(3):494–500. doi:10.1016/S0161-6420(01)00982-4
5. Hamilton A, Meena M, Lawlor M, Kourt G. An unusual case of intraorbital foreign body and its management. Int Ophthalmol. 2014;34(2):337–339. doi:10.1007/s10792-013-9786-7
6. Pinto A, Brunese L, Daniele S, et al. Role of computed tomography in the assessment of intraorbital foreign bodies. Semin Ultrasound CT MR. 2012;33(5):392–395. doi:10.1053/j.sult.2012.06.004
7. Patel SN, Langer PD, Zarbin MA, et al. Diagnostic value of clinical examination and radiographic imaging in identification of intraocular foreign bodies in open globe injury. Eur J Ophthalmol. 2012;22(2):259–268. doi:10.5301/EJO.2011.8347
8. Lakits A, Prokesch R, Scholda C, et al. Orbital helical computed tomography in the diagnosis and management of eye trauma. Ophthalmology. 1999;106(12):2330–2335. doi:10.1016/S0161-6420(99)90536-5
9. Kubal WS. Imaging of orbital trauma. Radiographics. 2008;28(6):1729–1739. doi:10.1148/rg.286085523
10. Sung EK, Nadgir RN, Fujita A, et al. Injuries of the globe: what can the Radiologist offer? Radiographics. 2014;3:764–776.
11. Hoffstetter P, Schreyer AG, Schreyer CI, et al. Multidetector CT (MD-CT) in the diagnosis of uncertain open globe injuries. Rofo. 2010;182(2):151–154. doi:10.1055/s-0028-1109659
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.