Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 11
Understanding The Combined Effects Of The Knowledge Of HIV/AIDS Prevention Methods On Condom Use: A Case Of Njombe And Tanga Regions Of Mainland Tanzania
Authors Aloni M, Mbago MCY, Sichona FJ
Received 4 April 2019
Accepted for publication 16 October 2019
Published 30 October 2019 Volume 2019:11 Pages 265—274
DOI https://doi.org/10.2147/HIV.S210758
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Mbwiga Aloni,1 Maurice CY Mbago,2 Francis J Sichona2
1Department of Mathematics, Physics and Information Technology, Mkwawa University College of Education (MUCE), Iringa, Tanzania; 2Department of Statistics, University of Dar es Salaam (UDSM), Dar es Salaam, Tanzania
Correspondence: Mbwiga Aloni
College of Education, Mkwawa University, Iringa 2513, Tanzania
Tel +255 755 284 849
Email [email protected]
Aim: This study assesses how the combined effects of knowledge of the HIV/AIDS prevention methods (ie, abstinence (A), being faithful (B), condom use (C), and diagnosis or testing (D)) influence behavioral change in terms of condom use.
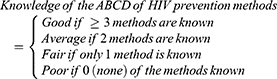
Methods: The study employed a cross-sectional design. Data were collected using a household survey conducted in 2017 in the Tanga and Njombe Regions of Tanzania through a structured questionnaire. The dependent variable was condom use during the last sexual intercourse. The main independent variable was knowledge of HIV prevention methods, referred to in this study as “knowledge of ABCD of HIV/AIDS prevention”. A respondent with knowledge of three or more of the ABCD was classified as having good knowledge of HIV prevention. Those with knowledge of two, one, or none of the ABCD were classified as having average, fair, and poor knowledge of HIV prevention methods, respectively. Data analysis included univariate analysis, bivariate analysis, and multivariate logistic regression analysis. The study included 660 respondents aged 15–64 years.
Results: The study indicates that the majority (52.2%) of the respondents had average knowledge of the HIV prevention methods. That is, they were knowledgeable of any two of the A, B, C, and D of HIV prevention methods. Condom use during the last sexual intercourse was reported by 46.5% of respondents. Multivariate analysis showed that condom use was 1.48-times more likely among respondents with good knowledge of ABCD of HIV/AIDS prevention than those with poor knowledge.
Conclusion: The predictive effect of knowledge of the HIV prevention methods on condom use was more visible when assessed in combination than when treated at A, B, C, and D in isolation. This suggests that successful behavioral change towards HIV/AIDS aversion requires dedicated efforts that promote comprehensive knowledge of all the methods through which the epidemic can be transmitted.
Keywords: combined knowledge of ABCD, condom use, high and low HIV/AIDS, prevalence regions, multivariate, Tanzania
Background
Knowledge precedes behavioral change. The necessary behavioral change required to prevent the spread of sexually transmitted infections (STIs), including Human Immunodeficiency Virus (HIV), is the knowledge about it that people need to have in order to reduce the chances of it being contracted especially through abstinence (A), being faithful to one uninfected partner who has no other partners (B), using a condom during sexual intercourse (C), and early HIV detection (D).1,2 A, B, and C focus on preventing the new HIV infection, while D focuses on the way of knowing one’s HIV status. In the fight against new HIV infections, simultaneous knowledge on methods of prevention and early virus detection is needed, especially when the campaign against HIV/AIDS focuses on getting to zero new HIV infections; zero discrimination, and zero AIDS related deaths is advocated.3
HIV is among the Lentivirus that causes chronic and deadly diseases in mammalian species including humans.4 When HIV is not diagnosed and treated early over time, it causes Acquired Immune Deficiency Syndrome (AIDS) in which the immune system begins to fail and permits other infections to intimidate the human body. In 2017, more than 36 million people were living with HIV around the world, and only 21.7 million people were receiving treatment. Moreover, more than 35 million people had died of AIDS globally.5 Although the proportion of people receiving Antiretroviral Therapy (ART) in Tanzania is as high as more than 90%, still 81,000 new cases of HIV infection were reported to arise in Tanzania.6
Properly consistent condom use during sexual intercourse has been advocated in order to reduce the new HIV infections. However, the use of a condom during sexual intercourse was reported to be very low, especially in sub-Saharan countries.7 In a study conducted by Norman8 only 19% of the respondents were reported to have used a condom at the last sexual intercourse. However, the main problem was on the techniques to use in order to maximize the proper use of the condom, particularly in regions with high HIV prevalence.
In the fight against HIV/AIDS worldwide, scholars through research-based evidence have emphasized the abstinence method, especially for people who are not yet married.9,10 However, this method has been challenging as in many societies people undermine the importance of abstinence and some of the claims have been related to biological factors such as an increase in hormonal level, especially at puberty, that eventually causes increased sexual desire and sex drive.11,12 It is, however, dangerous for the young people who begin sexual intercourse at early age as their chances of using a condom is low due to limited knowledge as compared to the experienced sexual partners.13
Marital union, whether formal or informal, does not guarantee the protection of new HIV infection, except when partners avoid having sexual intercourse outside the union. Although, faithfulness is being regarded as a primary measure to combat new HIV infection,14 the problems arise in managing the faith of the sexual encounter. Studies have reported that faithfulness has increased the risk of HIV infection when no conditions are imposed to guide effective faithfulness.15,16 The highest possibility of acquiring new HIV is having unprotected sex with the person whose HIV status is unknown.
Special intervention programs for promoting condom use are widespread. A study conducted in Indiana among high-risk female adolescents showed that 54% of the clients who returned after 6 months reported an increase in use of condoms, but most clients remained inconsistent users.17 The use of condoms for the prevention of HIV/AIDS was found to be influenced by individual, socio-cultural, and external factors. Unlike abstinence, that is, to avoid sexual intercourse and practicing mutualmonogamy, the use of a condom has a higher chance of protecting against new HIV infection than any other prevention technique.18
Early diagnosis of HIV/AIDS provides a well-timed access to ART, and better handling of extra infections in the efforts towards improving the patient outcomes as well as the quality of living. Persons living with HIV who are diagnosed can be linked to healthcare centres and receive treatment to reduce morbidity. However, when it is known that your sexual partner is HIV positive, it is very likely to stop you having sexual intercourse for fear of being infected. This, for those who are in a marital union, tends to heighten their self-confidence in the use of condoms during sexual intercourse. The use of condoms has been reported to be mostly requested by women when their sexual partners are known or suspected to have an STI, including HIV.19 When quantifying the benefits of diagnosing HIV/AIDS to persons living with HIV who are aware and unaware of infection in the US, it was revealed that those who were unaware of their infection were 3.5-times more likely to have unprotected sexual intercourse than those who are aware.20 The extent to which awareness of HIV status reduces new HIV infection can help in guiding strategies aimed to ensuring more people are diagnosed with HIV status prior to engagement in risky sexual intercourse.
There exists widespread knowledge of A, B, C, and D of HIV/AIDS prevention methods among males and females aged 15–49 years in Tanzania. Indeed, the statistics from Tanzania HIV and Malaria Indicator Survey (THMIS) show that 69% and 77% of women and men, respectively, believe that chances of acquiring HIV can be reduced by using a condom during sexual intercourse, while 84% and 87% of women and men, respectively, know that the chances of transmitting HIV can be reduced by having sexual intercourse with one uninfected partner who has no other partners.21 In examining methods of HIV prevention independently, the proportion of those with knowledge of A, B, and C in 2017 was as high as 91%, 88%, and 74%, while less than 50% of respondents were knowledgable on early detection as a primary method of HIV prevention in Abuja-Nigeria.22
The Tanzania Demographic and Health Survey (TDHS), in its assessment of the combination of knowledge using two primary methods of HIV prevention, reported that more than 70% of respondents know both methods (use of condom and being faithful to one uninfected partner who has no other partners) minimize the chances of transmitting new HIV infection.23Also, knowing the HIV status of yourself and your sexual partner prior to having risky sexual intercourse can lessen the likelihood of spreading the new HIV infection. The THMIS conducted in 2011–2012 revealed that 79% of women and 84% of men said that a woman is justified in asking the use of a condom if she knows her husband has an STI.18 Although, the relationship between STI detection and the knowledge of ABCD in isolation have been identified,23 the research studies on the existence of a combined knowledge of ABCD of HIV prevention through condom use among women and men aged 15–64 years in high and low HIV prevalence regions of mainland Tanzania is novel. Thus, the present study addressed the role of combined knowledge of ABCD of HIV prevention on condom use in the Njombe and Tanga regions of Tanzania.
Methodology
Study Design And Sampling
The study employed a cross-sectional design. The data were collected through the use of structured questionnaires. Njombe and Tanga regions were selected purposively based on their HIV prevalence rate of high and low, respectively, when compared with other regions in mainland Tanzania as reported by Tanzania HIV and Malaria indicator survey of 2011–2012.20 Purposive sampling was also applied to downscale regions to districts with high and low rates of HI prevalence. In each district, stratified sampling was used to select two wards for the study. The wards were categorized into urban and rural. In each stratum, simple random sampling was used to pick one ward for the study and, in each ward; simple random sampling was used to identify the villages/streets where respondents were obtained.
Study Area And Study Population
The current study was done in two districts of Tanzania with high and low HIV prevalence, namely Makete and Lushoto districts in Njombe and Tanga regions, respectively. The HIV prevalence data at both regional levels indicated that Makete and Lushoto districts in the Njombe and Tanga region were among the most and least affected districts with HIV pandemic with their prevalence of 14.8% and 1.8%,21 respectively. Despite a significant difference on the rate of HIV prevalence, both districts seem to have a comparable weather but with a slight difference in terms of socio-economic activities that people in the two districts are engaged in. Studies also have reported that more than 96% of residents in both districts are living in rural areas, and ~ 90% of the households depend primarily on the under-developed smallholder agricultural production characterised by the use of inferior agricultural tools such as hand hoes and reliance upon traditional rain-fed cropping methods. The main food crops grown in both districts include maize, beans, Irish, and round potatoes. The other sources of income of the people in both districts are the livestock and forestry products.24,25 Respondents in this study were selected using simple random sampling from a list of all households obtained from the village executive officer (VEO). Respondents participated were males and females aged 15–64 years.
Variables And Statistical Analysis
The outcome variable for this study was condom use. Condom use was assessed at the last sexual intercourse by each respondent.19 Condom use was considered to have occurred if either a male or female condom was used during the recent sexual intercourse. This variable consisted of two categories of “Yes” if a condom was used or “No” if a condom was not used at the last sexual intercourse.
The main independent variable was knowledge of ABCD of HIV prevention methods. This variable was constructed using the following questions with respect to the ABCD methods: could people reduce the chance of getting HIV/AIDS by not having sexual intercourse at all? By having one uninfected sex partner who has no other partners? By using a condom every time they have sex? By testing/diagnosing the HIV/AIDS status? Each of these individual knowledge variables forming the “ABCD” was binary with codes of “1” and “0” for responses “YES” and “NO”, respectively. That is to say, the correct knowledge on any one of the ABCD was assigned a score of “1” and an incorrect knowledge was given a score of “0” for computational purposes. In answering the questions, a respondent who said “YES” to at least any three aspects of the ABCD was considered as having good knowledge of the “ABCD” of the HIV prevention methods. Average knowledge was considered as knowledge of any two of the ABCD. Fair knowledge referred to the knowledge of any one of the ABCD. Finally, absence of knowledge of all the four components of ABCD was considered as poor knowledge.
The scores ranged from “0” (if the respondent did not have knowledge of any of the ABCD), to “4” (if the respondent had knowledge of all the ABCD). Since the observed frequencies of respondents with knowledge of all ABCD were small, their frequencies were combined with those having knowledge of any three of ABCD. Finally, a variable representing the knowledge of the “ABCD” of HIV prevention methods was constructed with four categories, as presented mathematically below.
Other independent variables included in the present study were the sex of the respondent, age, the status of the respondent, alcohol consumption, the highest level of education attained, the region of residence, and socio-economic wellbeing.
Data Analysis
The study used both descriptive and analytical analysis. In the descriptive analysis, frequency distribution tables and charts were presented in order to examine the characteristics of the study variables. Cross-tabulation of condom use by combined knowledge of the ABCD of HIV prevention and other independent variables was performed. Pearson’s Chi-square test was used to test the significance of associations between each pair of cross-tabulated variables.
Multivariate analysis was conducted using logistic regression. Selection of variables in the multivariate analysis was based on the evidence that the contribution of each variable to the overall model is statistically significant. This was determined by using the log-likelihood ratio test. The effect of each independent variable on condom use is indicated by the adjusted odds ratio (OR) for each variable relative to the reference category.
Ethical Considerations
The University of Dar-es-salaam Research Coordinating Committee approved the research protocols. All household visits and questionnaires in this study were conducted with individual informed consentand the involvement of each respondent was voluntarily. All participants signed an informed consent form before the interview. For participants below age 18 years of age, consent was sought from their parents or legal guardians. During the field work, data was managed very securely and confidentially. Access to the data forms was limited to a few staff.
Results
Characteristics Of The Study Sample
The study involved 660 male and female participants aged 15–65 years. At least one third (33.6%) of the respondents were in the age range 15–24 years. Those aged 25–34 years constituted 29.4% of the sample. The percentages of respondents for those aged 35–44 and 45–54 years were 18.8% and 10.8%, respectively (see Table 1). With regards to sex, 55.8% were females and 44.8% were male respondents. Regarding their residences, the high proportion (63.3%) of the respondents was from Makete district and 36.7% were living in Lushoto district. With regard to the religious affiliation of the respondents, 62% were Christians and 38% were Muslims. More than fifty percent (54.7%) of the respondents were found to be married or cohabiting and the proportion of never married respondents were 15.6% and 29.7% respectively.
 |
Table 1 Distribution Of The Study Participants And Knowledge Of ABCD Among Male And Female Respondents In Lushoto And Makete Districts Of Tanzania |
On level of education, the study found the majority (47.3%) of respondents constituted secondary or higher education. Those with primary education constituted 44.8%, and about 8% had never been to school. The proportion of respondents who mentioned business as their main economic activity was 20.8%, while 2.4% of the respondents were not involved in any socio-economic activities. On the knowledge of ABCD, the majority (52.2%) were found to have average knowledge, those considered to have poor and good knowledge of ABCD constituted 12% and 26.7% of the participants, respectively (see Table 1).
Incidence Of Condom Use
The findings in Figure 1 show that the overall proportion of condom use at last sexual intercourse amounted to 46.5%. A higher rate percentage (47.6%) was in Makete district and a lower percent (44.0%) was in Lushoto district.
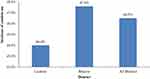 |
Figure 1 Incidence of condom use at the last sexual intercourse by District of residence in Tanzania, 2017 (Source: Field Data, 2017). |
Knowledge Level Of A, B, C And D
The data on knowledge of abstinence (A), being faithful (B), condom use (C), and diagnosis of HIV (D) is presented in Figure 2. Thus, 92.4% of respondents reported that they knew that people could reduce their chances of getting HIV infection by not having sexual intercourse (ie, abstinence), whereas 75.5% of the respondents reported to have the knowledge that people can reduce their chances of getting HIV/AIDS by having one partner who is not infected with HIV and has no other partners. With regards to the use of condoms during sexual intercourse, respondents who reported to have the knowledge that the use of a condom can reduce the chances of acquiring HIV comprised 83.7% of the respondents. Knowledge of undergoing HIV testing upon which people can reduce chances of getting HIV by understanding the HIV status of their sexual partners prior to sexual intercourse was reported by 81.6%.
 |
Figure 2 Knowledge of A, B, C, and D to respondents in Lushoto and Makete District in Tanzania, 2017 (Source: Field Data, 2017). |
Factors Associated With Condom Use
There was a significant association between the knowledge of the ABCD of HIV prevention methods and condom use at the last sexual intercourse (p=0.037). The proportion of respondents who reported to use condoms during sexual intercourse within the last 12 months prior to this study was 56.3%, including those with good knowledge of ABCD. It was also that 44.1%, 47.1%, and 37.9% were for those with average, fair, and poor knowledge of ABCD, respectively.
It was also observed that respondents in the age groups 25–34 and 15–24 years formed 51.2% and 49.5% of those reported to have used a condom during their last sexual intercourse, respectively (p=0.009). Similarly, the respondents aged 55–64 years who formed the lowest proportion of 19.4% reported to use a condom during their last sexual intercourse.
As for marital status, a significant relationship (p=0.001) was observed with the use of a condom during the last sexual intercourse. The proportion was 40% of the married or cohabiting respondents who reported to have used a condom during their last sexual intercourse. This was found to be 47.9% and 57% for the ever and never married respondents, respectively. The percentage of those reported to have not used a condom at their last sexual intercourse varied by level of education. For example, respondents who had never been to school were the highest proportion of non-condom users during their last sexual intercourse, and this formed 75%. The rate of condom use was, however, similar among respondents with primary and higher education (48% vs 48.6%) (p=0.012)
Condom use during the last sexual intercourse was observed to depend (p<0.001) on the number of sexual partners in the last 12 months. It was also observed that the majority of respondents (71.8%) who had more than one sexual partner outside the marriage and used a condom during their last sexual intercourse was higher compared to those who had only one sexual partner outside the marriage (58.8% of the respondents). Interestingly, those with no sexual partner outside the marriage who used a condom during the last sexual intercourse were formed 39.1% of the respondents (see Table 2).
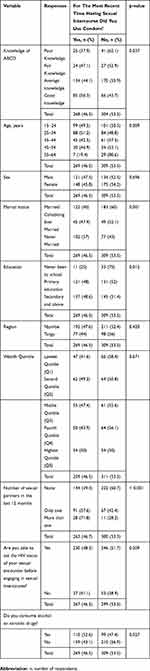 |
Table 2 Bivariate Analysis Of Factors Associated With Condom Use |
It was also indicated that the higher proportion (52.6%) of respondents who consumed alcohol or narcotic drugs affirmed to have used a condom during their last sexual intercourse as compared to those who were not consuming alcohol or narcotic drugs (43.1%) (p=0.027).
Variables which were not significantly associated with condom use included sex of respondents (p=0696), region of residence (p=0.420), wealth status (p=0.671), and being able to ask the HIV status of the sexual encounter prior to engaging in sexual intercourse (p=0.209) (see Table 2).
Multivariate Logistic Regression Of Factors Associated With Condom Use
The data analysed in the multivariate logistic regression model of condom use revealed that, upon controlling other factors, respondents with good knowledge of ABCD of the HIV prevention methods were significantly (1.48-times) more likely to use a condom at the last sexual intercourse than those with poor knowledge of ABCD (OR=1.48, 95% CI=1.25–1.91, p=0.026).
On marital status, the findings showed that the odds of never married respondents who reported to use a condom during their last sexual intercourse were significantly (1.36-times) more likely than married or cohabiting respondents in the use of a condom during the last sexual intercourse (OR=1.36, 95% CI=1.21–1.63, p<0.001). Similarly, evidence on the likelihood of respondents who reported to have used a condom during their last sexual intercourse was presented on the ever married (divorced and widow) respondents. These respondents, who reported to have used a condom in their last 12 months prior to the present study, were 44% less likely compared to respondents who were married or cohabiting (OR=0.56, 95% CI=0.32–0.98, p=0.041).
It was also found that the number of sexual partner respondents reported to have excluded husband/wife was considered to be covariate with close-response relationship with the use of condom in such a way that the more the number of sexual partner, the higher the odds of condom use (one sexual partner: OR=0.29, 95% CI=0.23–0.75, p=0.001) and more than one sexual partner: (OR=0.50, 95% CI=0.13–0.63, p=0.002) (Table 3).
 |
Table 3 Multivariate Logistic Regression Of The Effect Of Independent Variable On Condom Use |
Discussion
The isolated knowledge of A, B, C, and D in the univariate analysis shows delayed sexual debut (abstinence) and condom use during sexual intercourse was pronounced by 92.4% and 83.7% as a method of HIV/AIDS prevention. This abstinence rate is high, compared to the 84% and 87% of women and men, respectively, reported by 2011–2012 THMIS. The expected mechanism for a high rate of abstinence and condom use as obtained in the present study is that, since the HIV prevalence was reported to be high in Njombe district, the Government and Non-government programs such as Mama Mkubwa26–28 and USAID KizaziKipya29 have invested their efforts heavily in order to create awareness and service uptake for HIV control in the area. This may have contributed to greater knowledge of HIV prevention methods observed among individuals.
The independent effect of the knowledge of the ABCD of HIV/AIDS prevention was examined in the multivariate logistic regression analysis. A key finding in this was that the higher the knowledge of ABCD of HIV prevention methods, the higher the odds of condom use at the last sexual intercourse. Specifically, respondents with good knowledge of ABCD of HIV prevention methods were significantly and independently 1.48-times more likely than those with poor knowledge to have used a condom during their last sexual intercourse. This effect was adjusted for age, marital status, education attainment, the number of sexual partners, and whether or not the respondents consumed alcohol and/or narcotic drugs.
This entails that, since people can be knowledgeable of HIV/AIDS, its transmission modes, and ways to mitigate its spread, there can also be a greater likelihood that they feel the urge to be careful in their sexual relationships by taking protective measures such as condom use, among others. This is crucial, noting that, as the war against the HIV epidemic advances globally, massive gain will largely depend on everyone taking responsibility being accountable to their sexual behaviors. This finding is consistent with a recent study in Mozambique which found that knowledge of HIV–positive status (a proxy for testing) is associated with more frequent condom use,30 and several others,31,32 thus corroborating the known positive correlation between health knowledge and health practice.33 It is also argued that knowledge is imperative for social transformation and has been considered as a key factor in enhancing decision-making among individuals.34
Although there is evidence on the presence of negative association between knowledge of HIV transmission pathways and behavior change35,36 yet, there should be strategies that will promote the knowledge on ABCD of HIV prevention methods as one of the key mechanisms towards behavioral change for greater HIV risk aversion.
The properly consistent use of condoms during sexual intercourse was reported to be associated with protection against HIV infection,37 and a significant proportion of married and cohabiting respondents in the study area were at risk of contracting new HIV infection and unintended pregnancies. This also corroborates the findings of the present study which indicate that, among respondents who were in union, 60% did not use a condom during the last sexual intercourse. The likelihood of condom use during the last sexual intercourse was higher among never married respondents compared to married and cohabiting respondents, possibly due to good knowledge of ABCD and specifically knowledge on condom use. Similarly, the odds of using a condom were lower among ever married respondents as compared to married or cohabiting respondents. This may have occurred possibly due to the presence of relevant knowledge of ABCD to the married/cohabiting respondents and this eventually results in preventing both new HIV infection and other STIs.
It was also observed that the odds of condom use increased proportionally with an increase in the number of sexual partners respondents reported to have in the last 12 months prior to this study. The respondents who reported to have more than one sexual partner constituted almost 1-fold of the odds of condom use when compared with respondents who have never had multiple partners. The odds of condom use during the last sexual intercourse experience was higher among respondents who reported to have more than one sexual partner when compared with those who reported to have not experienced multiple sexual partners in the last 12 months. This is probably due to knowledge adaptations as gained about the spread and prevention of HIV/AIDS, as those with more than one sexual partner were assumed to be sexually experienced and hence have knowledge on some aspects of ABCD. This outcome is contrary to other studies.34,38 The differences in observation could be due to knowledge differences on ABCD.
Strengths And Limitations
Considering that this was a cross-sectional study, no causal inferences may be drawn from these findings because of lack of temporality. It is also important to note that all pieces of information were self-reported without any possibility for objective verification. Reporting bias may also have affected this study because of the sensitivity of the issues assessed.
However, all precautionary measures were taken to minimize the limitations. The data collectors were trained, after which a pre-test was followed. The tool was then revised based on the findings from the pilot survey and the best data collectors were sent to the field for data collection. The data collection exercise was well supervised. Data analysis employed the best techniques – multivariate modeling. Unlike other studies, the knowledge questions were assessed in combination, rather than looking at each one in isolation. This enabled detection of their combined effect, an effect which was missed in individual variables.
Conclusion
Knowledge of the ABCD of HIV prevention methods is a key and crucial among individuals, especially when the campaign against HIV/AIDS is geared to end the new infections. This would largely promote condom use for HIV prevention among people of the target population. Given that formal education attainment improves condom use, it is important that the government should design programs that will spearhead the war against HIV/AIDS, while promoting the deeper understanding and sharing of relevant knowledge about the HIV/AIDS transmission pathways, especially through efforts geared towards the attainment of formal education.
Acknowledgments
We sincerely express our heartfelt thanks to the participants involved in this study; the data collectors, regional commissioners of Tanga and Njombe, District Council administrations, and ward executive officers for their support during data collection exercise. We also extend our gratitude to the management of Mkwawa University College of Education for funding this study. An earlier draft of this paper was first presented as a poster at the 5th Tanzania Health Summit held in Dar es salaam, Tanzania from November 13–14, 2018. Inputs received from the members of the summit were incorporated for improvements. We also extend our sincere appreciation to Amon Exavery, the Research and Learning Coordinator of People Acting in Community Together in Tanzania (PACT) for proofreading an earlier draft of this paper.
Disclosure
The authors of this paper declare that they have no competing interests in this work.
References
1. Marrazzo JM, Cates W. Interventions to prevent sexually transmitted infections, including HIV infection. Clin Infect Dis. 2011;53(suppl_3):S64–S78. doi:10.1093/cid/cir695
2. Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR recommendations and reports: morbidity and mortality weekly report Recommendations and reports. Morb mort week rep.2015;64(RR–03):1.
3. Haghdoost A, Karamouzian M. Zero new HIV infections, zero discrimination, and zero AIDS-related deaths: feasible goals or ambitious visions on the occasion of the world AIDS day? Int J Prev Med. 2012;3(12):819. doi:10.4103/2008-7802.104850
4. Van Tulleken CR Characterisation of Lentiviral Vpr Function and Mechanism. 2017.
5. UNAIDS GA. Global AIDS Update 2016. Geneva, Switzerland: World Health Organization Library; 2016.
6. Tanzania T. Tanzania HIV Impact Survey 2016/2017. Tanzania Commission for AIDS; 2017.
7. Maticka-Tyndale E. Condoms in sub-Saharan Africa. Sex Health. 2012;9(1):59–72. doi:10.1071/SH11033
8. Norman LR. Predictors of consistent condom use: a hierarchical analysis of adults from Kenya, Tanzania and Trinidad. Int J STD AIDS. 2003;14(9):584–590. doi:10.1258/095646203322301022
9. Lindskog A, Durevall D Education and HIV: Evidence from Botswana. 2018.
10. Costa FM, Jessor R, Donovan JE, Fortenberry JD. Understanding early initiation of sexual intercourse in adolescence. In: Problem Behavior Theory and Adolescent Health. Springer, Cham. 2017:325–349.
11. Hayes CD. Risking the Future: Adolescent Sexuality, Pregnancy, and Childbearing. Vol. 1. National Academies; 1987.
12. Santelli JS, Kantor LM, Grilo SA, et al. Abstinence-only-until-marriage: an updated review of US policies and programs and their impact. J Child Adolesc Health. 2017;61(3):273–280. doi:10.1016/j.jadohealth.2017.05.031
13. Donenberg GR, Bryant FB, Emerson E, Wilson HW, Pasch KE. Tracing the roots of early sexual debut among adolescents in psychiatric care. J Am Acad Child Adolesc Psychiatry. 2003;42(5):594–608. doi:10.1097/01.CHI.0000046833.09750.91
14. Jacobson M, Marquez C, Luetkemeyer A Comprehensive, up-to-date information on HIV/AIDS treatment and prevention from the University of California San Francisco.
15. Painter TM, Diaby KL, Matia DM, et al. Faithfulness to partners: a means to prevent HIV infection, a source of HIV infection risks, or both? A qualitative study of women’s experiences in Abidjan, Côte d’Ivoire. Afr J AIDS Res. 2007;6(1):25–31. doi:10.2989/16085900709490396
16. Wenzel SL, Henwood B, Harris T, Winetrobe H, Rhoades H. Provider perceptions on HIV risk and prevention services within permanent supportive housing. AIDS Care. 2017;29(10):1331–1335. doi:10.1080/09540121.2017.1330533
17. Assenga EN Factors influencing young people’s preventive actions against human immunodeficiency virus infections in Tanzania. 2009.
18. DeCarlo P Do condoms work? 1998.
19. Exavery A, Kanté AM, Jackson E, et al. Role of condom negotiation on condom use among women of reproductive age in three districts in Tanzania. BMC Public Health. 2012;12(1):1097. doi:10.1186/1471-2458-12-1097
20. Marks G, Crepaz N, Janssen RS. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. Aids. 2006;20(10):1447–1450. doi:10.1097/01.aids.0000233579.79714.8d
21. TACAIDS Z, NBS OCGS I.. Tanzania HIV/AIDS and Malaria Indicator Survey 2011–12. Dar es Salaam, Tanzania Dar es Salaam, Tanzania: Tanzania Commission for AIDS (TACAIDS), Zanzibar AIDS Commission (ZAC), National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), and ICF International; 2013.
22. Bibiana NE, Emmanuel PO, Amos D, Ramsey YM, Idris AN. Knowledge, attitude and factors affecting voluntary HIV counseling and testing services among women of reproductive age group in an Abuja Suburb community, Nigeria. Med J Zambia. 2018;45(1):13–22.
23. ICF Macro I. Tanzania demographic and health survey 2010. 2011.
24. NBS (National Bureau of Statistics). Population Distribution by Administrative Areas. National Bureau of Statistics, Ministry of Finance, Dar es Salaam - Tafuta na Google; 2013. Available from: https://www.google.com/search?source=hp&ei=YgSCXa7QNK-TlwTShLCgCg&q=24.%09NBS+%28National+Bureau+of+Statistics%29.+2013.+Population+Distribution+by+Administrative+Areas.+National+Bureau+of+Statistics%2C+Ministry+of+Finance%2C+Dar+es+Salaam&btnK=Tafuta+na+Google.
25. Council LD. Lushoto District Profile [Online]; 2016.
26. Anangisye WA. Bottlenecks in the access to primary education in Tanzania: the struggles of vulnerable school children in Makete District. KEDI J Educ Pol. 2011;8:2.
27. Mmasa J, Mbaula W
28. District M, Region I. Evaluation of Tahea supported “Mama Mkubwa” initiative. 2005.
29. Sikira AN, Sanga AP Community perception on male circumcision for HIV/AIDS prevention in Makete district. 2013.
30. Dokubo EK, Shiraishi RW, Young PW, et al. Awareness of HIV status, prevention knowledge and condom use among people living with HIV in Mozambique. PLoS One. 2014;9(9):e106760. doi:10.1371/journal.pone.0106760
31. Haddad LB, Tang JH, Krashin J, et al. Factors associated with condom use among men and women living with HIV in Lilongwe, Malawi: a cross-sectional study. BMJ Sex Reprod Health. 2018;44(1):1–12. doi:10.1136/bmjsrh-2017-101825
32. Sharma B, Nam E. Condom use at last sexual intercourse and its correlates among males and females aged 15–49 years in Nepal. Int J Environ Res Public Health. 2018;15(3):535. doi:10.3390/ijerph15030535
33. Dowell LJ. The relationship between knowledge and practice. J Educ Res. 1969;62(5):201–205. doi:10.1080/00220671.1969.10883815
34. Exavery A, Lutambi AM, Mubyazi GM, Kweka K, Mbaruku G, Masanja H. Multiple sexual partners and condom use among 10–19 year-olds in four districts in Tanzania: what do we learn? BMC Public Health. 2011;11(1):490. doi:10.1186/1471-2458-11-490
35. Fylkesnes K, Musonda RM, Kasumba K, et al. The HIV epidemic in Zambia: socio-demographic prevalence patterns and indications of trends among childbearing women. Aids. 1997;11(3):339–345. doi:10.1097/00002030-199703110-00012
36. Zambia Sexual Behavior Survey 1998 — MEASURE Evaluation. Available from: https://www.measureevaluation.org/resources/publications/tr-99-02. Accessed September 18, 2019.
37. Tarkang EE. Condom use and number of sexual partners among secondary school female students in an urban city of Cameroon. Rwanda J Health Sci. 2013;2(2):30–33. doi:10.4314/rjhs.v2i2.6
38. Mayaphi SH, Martin DJ, Olorunju SA, Williams BG, Quinn TC, Stoltz AC. High risk exposure to HIV among sexually active individuals who tested negative on rapid HIV tests in the Tshwane District of South Africa—the importance of behavioural prevention measures. PLoS One. 2018;13(2):e0192357. doi:10.1371/journal.pone.0192357
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
