Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 15
Understanding Clinicians’ Perceived Barriers and Facilitators to Optimal Use of Acute Oxygen Therapy in Adults
Authors Cousins JL , Wark PAB , Hiles SA , McDonald VM
Received 20 May 2020
Accepted for publication 18 August 2020
Published 25 September 2020 Volume 2020:15 Pages 2275—2287
DOI https://doi.org/10.2147/COPD.S263696
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Joyce L Cousins,1– 3 Peter AB Wark,3,4 Sarah A Hiles,1,3 Vanessa M McDonald1,3,4
1School of Nursing and Midwifery, University of Newcastle, Newcastle, NSW, Australia; 2Faculty of Nursing, Avondale University College, Sydney, NSW, Australia; 3Centre of Excellence in Severe Asthma & Priority Research Centre for Healthy Lungs, Hunter Medical Research Institute, University of Newcastle, Newcastle, NSW, Australia; 4Department of Respiratory and Sleep Medicine, John Hunter Hospital, Newcastle, NSW, Australia
Correspondence: Vanessa M McDonald
Centre of Excellence in Severe Asthma & Priority Research Centre for Healthy Lungs, Hunter Medical Research Institute, The University of Newcastle, Newcastle, NSW 2305, Australia
Tel +61240420146
Fax +61240420046
Email [email protected]
Background: Supplemental oxygen is commonly administered to patients in acute care. It may cause harm when used inappropriately. Guidelines recommend prescription of acute oxygen, yet adherence is poor. We aimed to identify barriers and facilitators to practicing in accordance with the evidence-based Thoracic Society of Australia and New Zealand (TSANZ) oxygen guideline, and to determine the beliefs and attitudes relating to acute oxygen therapy.
Methods: A national cross-sectional survey was conducted. The survey consisted of 3 sections: (1) introduction and participant characteristics; (2) opinion/beliefs, knowledge and actions about oxygen therapy and other drugs; and (3) barriers and facilitators to use of the TSANZ guideline. Convenience sampling was employed. A paper-based survey was distributed at the TSANZ Annual Scientific Meeting. An online survey was emailed to the TSANZ membership and to John Hunter Hospital’s clinical staff.
Results: Responses were received from 133 clinicians: 52.6% nurses, 30.1% doctors, and 17.3% other clinicians. Over a third (37.7%) were unaware/unsure of the oxygen guideline’s existence. Most (79.8%) believe that oxygen is a drug and should be treated as one. Most (92.4%) stated they only administered it based on clinical need. For four hypothetical cases, there was only one where the majority of participants identified the optimal oxygen saturation. A number of barriers and facilitators were identified when asked about practicing in accordance with the TSANZ guideline. Lack of oxygen equipment, getting doctors to prescribe oxygen and oxygen being treated differently to other drugs were seen as barriers. The guideline itself and multiple clinician characteristics were considered facilitators.
Conclusion: There is discordance between clinicians’ beliefs and actions regarding the administration of oxygen therapy and knowledge gaps about optimal oxygen therapy in acute care. Identified barriers and facilitators should be considered when developing evidence-based guidelines to improve dissemination and knowledge exchange.
Keywords: acute oxygen therapy, prescription, COPD
Introduction
Oxygen therapy is commonly used in the acute care setting. Australian data suggest that up to 24% of all inpatients1 and up to 79%2 of those admitted with acute exacerbations of Chronic Obstructive Pulmonary Disease (AECOPD) receive oxygen therapy. In years 2017–2018, there were more than 4.3 million overnight admissions to public and private hospitals in Australia,3 with up to one million of these patients potentially receiving oxygen therapy. Chronic Obstructive Pulmonary Disease (COPD) admissions totaled 64,4953 in the same year, with up to 79% of these patients (50,951) potentially receiving oxygen therapy. While oxygen therapy is a key component in the treatment of patients hospitalized with an AECOPD,4,5 its use is not always optimal6–8 and has the real potential to cause harm.9–11 Meta-analysis has shown that liberal administration of oxygen therapy to acutely unwell adults increases mortality, with the relative risk of in-hospital death increasing by 25% for every one percent increase in peripheral oxygen saturation (measured by pulse oximeter [SpO2]).12 In COPD these outcomes are even more marked, with a 58% reduced risk of death in patients who receive titrated oxygen therapy.10 These data highlight the importance of appropriate prescription, monitoring and administration of oxygen therapy. International guidance recommends the prescription of oxygen therapy,9 yet poor adherence to these recommendations has been highlighted.13
In New South Wales public hospitals, a “Between the Flags” system is used with the “Standard Adult General Observation” (SAGO) chart to aid in recognizing and responding to clinical deterioration.14 This safety system requires clinicians to initiate a clinical review when an SpO2 falls below 95% unless altered call criteria are documented.15 In 2015, the Thoracic Society of Australia and New Zealand (TSANZ) released their first evidence-based guideline on the use of oxygen therapy for acute oxygen use in adults,16 using the National Health and Medical Research Council grading system, which was founded on evidence base, consistency of evidence, clinical impact, generalizability, and applicability.16 Both the TSANZ and British Thoracic Society (BTS) advocate for oxygen as a treatment for hypoxemia and not breathlessness, and advise that it should be prescribed to a target oxygen saturation range of 88%-92%9,16 in those with COPD or other chronic respiratory conditions where respiratory failure could be suspected. However, they differ in their recommendations around the target oxygen saturation range for those without COPD. The BTS recommended a target range between 94% and 98%9 and the TSANZ recommended a target range of 92%-96%.16 Data from the 2018 systematic review and meta-analysis by Chu et al12 support the recommendations of the 2015 TSANZ guideline for oxygen to be titrated to a maximum SpO2 of 96% but also recommend further research is needed to precisely define oxygen therapy strategies that maximize benefits and minimize harm. These data further add to the growing literature demonstrating that indiscriminate administration of oxygen increases mortality, and supports conservative administration of oxygen therapy across a broad range of acutely ill patients.12
Understanding clinicians perceived barriers or facilitators to the optimal use of acute oxygen therapy is necessary. With this in mind, our aims were to; determine the knowledge, beliefs and attitudes relating to acute oxygen therapy and prescription across a range of clinicians and to identify barriers and facilitators to practice in accordance with evidence-based guidelines.
Methods
Design
A national cross-sectional survey design was employed to explore the knowledge, attitudes, and beliefs on the use of an evidence-based guideline and identify potential barriers and facilitators to practicing in accordance with this guidance.
Setting and Data Collection
Convenience sampling was employed. Participants were invited to complete an online or paper-based survey. Participants were approached using a variety of methods, including email dissemination commencing in September 2016 to relevant clinical members of the TSANZ, and the John Hunter Hospital, Newcastle Australia. Participants were encouraged to forward the survey on to any clinicians that they felt may be interested in completing it. The survey remained open until September 2017. A paper version of the survey was also distributed at the 2017 TSANZ Annual Scientific Meeting during appropriate COPD sessions. A study-specific locked collection box was placed at the TSANZ stand to allow collection of anonymous surveys.
Participants
Clinicians (registered or enrolled nurses, doctors, physiotherapists, and paramedics/ambulance workers) who were 18 years old or older and who worked in an acute care hospital or emergency services were invited to participate.
Measures
We surveyed knowledge, attitudes, beliefs, and barriers and facilitators of use of an evidence based-guideline: the 2015 TSANZ guideline for acute oxygen use in adults, “Swimming between the flags”.16 Following a review of previously designed and validated instruments to investigate barriers and facilitators,17–19 no single instrument was deemed suitable for use in this study as they did not explore knowledge. Therefore, permission was sought and given to amend a previously validated instrument by Peters et al.20
The survey consisted of three sections to provide structure and enhance participants’ navigation.21,22 Sections one and two were developed based on a review of the available literature while section three utilized the amended instrument by Peters et al.20 Content and face validity for the entire survey were evaluated by a panel of eleven clinicians. Following this review, minor amendments were made.
The three sections were:
- Introduction and participant characteristics: This involved a brief introduction, links to participant information leaflet and the TSANZ guideline, and five closed-ended questions about the participant’s demographic data, professional role and experience. It also included one open-ended question about the participant’s main area of clinical practice.
- Opinion/beliefs, knowledge and actions about oxygen therapy and other drugs: Questions were informed by the aims of this study and a review of the literature on oxygen therapy that identified knowledge around the delivery of oxygen therapy is suboptimal, the prescription of oxygen therapy is poor and there is room for improvement in the accuracy of oxygen administration and monitoring.13 Therefore, 11 closed-ended questions explored the opinions/beliefs, knowledge and actions of clinicians about the use and prescription of oxygen therapy in the acute care setting. Clinicians were also asked about their beliefs and actions regarding various other drug therapies (oxygen therapy, IV fluids, antibiotics, paracetamol and salbutamol) to explore similarities or differences when working with these treatments. Following this were four hypothetical patient scenarios, where participants were asked to indicate the target saturation level from 5 multiple-choice options for each of the patient cases listed (see Table 3 for case scenarios given). Participants were then asked an open-ended question on their thoughts about giving oxygen therapy for dyspnea.
- Barriers and facilitators to using the TSANZ “Oxygen guideline for acute oxygen use in adults”16 This section included three open ended questions to allow for the expression of opinions and thoughts and the remaining 28 questions comprised of a three or five point Likert Scale to indicate levels of agreement to the 28 statements that explored barriers and facilitators to using the TSANZ oxygen guideline using a previously validated instrument by Peters et al.20 The original instrument by Peters et al20 was developed to identify barriers for implementing innovations and categorized the 28 questions into four domains and identified broad categories where either a barrier or facilitator may exist, including; innovation (the guideline), context, patient and health care practitioner. Accordingly, barriers and facilitators of the TSANZ guideline use were categorized into these four domains (Survey S1).
 |
Table 1 Demographic Data |
 |
Table 2 Selected Exemplars for the Question “What are Your Thoughts About Giving Oxygen for Dyspnoea” |
 |
Table 3 Case Scenarios |
Ethics approval was gained from the Hunter New England Human Research Ethics Committee (Reference: 16/04/20/4.03) and the University of Newcastle, Human Research Ethics (Approval: H-2016-0222). Participation was voluntary and completion inferred consent, with participants able to access further information on the project via an online link.
Data Analysis
Stata 11, V.14 (Stata Corporation, College Station, Texas, USA) software was used for analyzing survey quantitative data. Normally distributed variables are reported as mean (SD) and non-normal variables as median (interquartile range). Frequencies and percentages (%) described the categorical data. Chi-squared and Fisher’s exact tests were used to investigate associations between categorical data as appropriate. P values of less than 0.05 were considered statistically significant.
The 5-point Likert scale responses were combined in the categories “strongly disagree” and “disagree” and “strongly agree” and “agree” to analyze the results in three response categories to facilitate visual interpretability.
Frequency content analysis was used to code qualitative responses to the free text questions.
Results
Section 1: Participants
Surveys were completed by 133 participants. More than a third (37.7%) indicated that they were not aware or were unsure if they were aware of the existence of the TSANZ guideline on oxygen therapy. Basic demographic data are presented in Table 1.
Section 2: Beliefs and Actions of Clinicians
Overall, most clinicians (79.8%) believed that oxygen therapy is a drug and should be treated like other drugs. Fewer (14.3%) believed that it was a drug but should not be treated like other drugs and less than four percent (3.4%) believed that it was not a drug. Few respondents (2.5%) believed that it was not a drug but should be treated as one. No significant differences were seen between the four professional groups (p=0.074). Most clinicians (92.4%) said that they only give oxygen therapy based on clinical assessment. Almost six percent (5.9%) stated that they either always give oxygen therapy for those who are short of breath, or that they know it does not help everyone, but it helps most so they always administer it. Less than two percent (1.7%) stated they never give oxygen for dyspnea. No significant differences were seen between the four professional groups (p=0.194). Free text responses to the question “what are your thoughts about giving oxygen for dyspnea” were received from 110 participants. During content analysis, five themes emerged (Table 2) which concurred with the quantitative data. The largest number of responses (81 of 110) from clinicians suggesting that “clinical assessment and titration to saturations was required” prior to giving oxygen therapy to a patient. Clinicians also identified that there were “other alternatives to oxygen therapy” for dyspnea, and that oxygen worked as a “placebo” for many patients. Several clinicians responded that administration of oxygen “Does not help” dyspnea and that instead, it may cause harm while fewer clinicians suggested that giving oxygen for dyspnea “May help a patient.”
Participants were asked to list how important they believed (beliefs) the detailed prescription of oxygen was and asked to indicate how often they administer (actions) oxygen when no prescription was written. They were also asked to do the same for four other medications, IV fluids, antibiotics, paracetamol and salbutamol. Figure 1 illustrates that overall clinicians' beliefs match their actions when it comes to IV fluid and antibiotic prescription and administration. Almost 100% agreed that a detailed prescription (Figure 1: 97% for IV fluids and 98% for antibiotics) was very important and most (Figure 1: 75% and 92%, respectively) said they never administered these without a prescription. However, the beliefs and actions differ when examining the responses for paracetamol, oxygen and salbutamol. Most (Figure 1: 81%-paracetamol; 87%-salbutamol; 72%-oxygen) believe that a detailed prescription is very important for these three medications, fewer said that they never administered these without a prescription (Figure 1: 52%; 56% and 21%, respectively). In other words, many administer these medications when there was no prescription written. In the case of oxygen therapy, 72% stated that they believed that a prescription was very important; however, nearly 80% stated that they either always or sometimes gave oxygen even without a prescription.
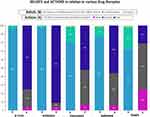 |
Figure 1 Beliefs and actions in relation to various drug therapies. |
Knowledge Related to Oxygen Therapy
Participants were asked to indicate the target saturation level for four hypothetical patient scenarios (Table 3). Overall, the only scenario where a patient’s optimal saturation was identified by more than 50% of the participants was that of “Mr Riley”, who was clearly identified as a COPD patient. More than two-thirds (69.6%) of the participants identified the recommended saturation range (88–92%). The optimal saturation target was identified by approximately a quarter of participants for the remaining scenarios.
Section 3: Barriers and Facilitators
Barriers where respondents agreed or strongly agreed with the statement in greater proportions to those who disagreed have been listed in Table 4. Similarly, facilitators where respondents disagreed or strongly disagreed with the statement in greater proportions to those who agreed are also listed in Table 4. Barriers to implementing the guideline included lack of available equipment (i.e. correct oxygen equipment), difficulties in getting doctors to prescribe oxygen therapy, identification that oxygen was not treated with the same care as other drugs and poor administration and monitoring of oxygen therapy by nurses were all identified as barriers to guideline implementation. While similar numbers of clinicians read and remembered the guideline (41%) when compared to those who stated that they did not read or remember the guideline (46%). This is a similar result to an earlier question that asked whether participants were aware of the guideline, where 38% stated that they were not aware or were unsure if they were aware of the guideline (Table 1). The number of clinicians who indicated that they had not read or remembered the guideline do present as a barrier.
 |
Table 4 Barriers and Facilitators to Practicing in Accordance with the TSANZ Guideline |
The guideline itself (innovation) and multiple clinician (care provider) characteristics were considered facilitators to implementing the TSANZ oxygen guideline (Table 4). These clinician characteristics identified that respondents believed that they did not resist working with protocols, did not have difficulty in changing their routines or did not find it difficult to work with the guideline because they had not been involved in setting up the practice change (84%, 81% and 69%, respectively). They also demonstrated agreement with the guideline itself by disagreeing with the statement “an SpO2 level of 92% is too low for most patients” and that “It is difficult to provide evidenced-based care to patients who are acutely short of breath who appear to need more oxygen than the guideline recommends.” (77% and 56%, respectively). However, when asked if they believed that parts of the guideline were incorrect 49% indicated that they were unsure by neither agreeing or disagreeing with the statement and 50% disagreeing with the statement. The majority felt that the guideline concepts were consistent with their training and that they were adequately trained (76% and 72%, respectively).
When asked if organizational policies prevent the use of the guideline, clinicians were asked to give an example if they agreed or strongly agreed with the statement. Fewer (22%) clinicians agreed or strongly agreed with the statement than disagreed or strongly disagreed (30%). Of those who agreed, 20 clinicians offered further detail and examples. The most common response related to organization’s use of the “Standard Adult General Observation” (SAGO) chart and “Between the flags” protocols. The SAGO chart requires initiation of a clinical review if an SpO2 ≥95% is not maintained. This does not align with the current recommendations provided by the TSANZ who advocate to maintain an SpO2 above 92% for most patients. Clinicians' comments highlight the difficulties experienced in using the SAGO chart. Examples of these comments are highlighted in Table 5.
 |
Table 5 Selected Exemplars for the Question “if You Agree or Strongly Agree That Organizational Policies Prevent the Use of This Guideline, Please Give an Example.” |
Discussion
Findings from this study identify that clinicians believe that oxygen is a drug and should be treated like other drugs. It is importantly demonstrated however that knowledge around the most appropriate oxygen saturation levels for patients with a variety of medical conditions is suboptimal and should be improved. This study identified several barriers and facilitators to the utilization of this evidence-based guideline. Many of these barriers and facilitators related to the clinicians themselves while the guideline itself was seen to be a facilitator to adoption. Both the “context of care” (equipment available) and the “patient” (patients who do not know what their diagnosis is) were seen as a barrier.
Appropriate oxygen delivery like any health-care practice requires the utilization and uptake of evidence-based guidelines. Effective translation of evidence into clinical practice requires an understanding of the barriers and facilitators23 and this study may assist in providing guidance on how to best facilitate the translation of this commonly used therapy into clinical practice to ultimately improve patient outcomes.
This national study has demonstrated that knowledge about the TSANZ guideline content was sub optimal. There is scope for improvements in disseminating this evidence to clinicians and promoting its existence and importance. Most clinicians believed that oxygen is a drug and should be treated like other drugs. Our data demonstrate a shift in attitudes towards administering oxygen for dyspnea when compared to other studies.24,25 While the use of oxygen for dyspnea appears to be less common, efforts to educate those who continue to use it as a treatment for dyspnea alone needs to continue. Free text responses revealed that several clinicians believe that oxygen is useful as a placebo or that it may help the patient. A previous qualitative study26 identified that oxygen was used by clinicians as a cure-all. Like our findings, “anxiety” or its use as a placebo was commonly cited as a reason for giving oxygen.
There were variations between clinicians’ beliefs and actions for the different drug therapies listed. Both IV fluids and antibiotics were treated similarly. This was not true for the other drugs. Both paracetamol and salbutamol are “over the counter” medications in Australia. They are also considered “nurse-initiated medications” in many acute care settings and must be administered and documented according to hospital policy. Oxygen therapy is also considered a “nurse-initiated medication”; however, its administration does not require documentation on a medication chart and this may, in part, explain why beliefs and actions do not match for the use of oxygen therapy. These comparative data provide insightful knowledge about the perception of oxygen in comparison with other commonly used medications in the acute care setting.
Previous studies exploring beliefs and actions in critical care areas27–29 have demonstrated variability in oxygen therapy practice. Small et al30 compared the use and misuse of oxygen compared to antibiotics in an inpatient cohort in 1990 and demonstrated that oxygen therapy was not prescribed or administered with the same care as that given to antibiotics. Highlighting that this is a longstanding problem with little change in behavior over time. Most clinicians in our study rated the importance of a written prescription as very high for all the medications listed. It is not clear why differences exist between the different drug groups with respect to clinician actions, but not for clinician beliefs. It is possible that because both IV fluids and antibiotics are prescription-only medications, there is appropriate reluctance to administer these without a valid prescription. In addition, clinicians may administer oxygen therapy (without a prescription) to improve oxygenation in patients who are hypoxic. Many studies have shown that the prescription of oxygen is poor31–34 and to withhold oxygen therapy when it is needed, due to a lack of a valid prescription would be poor practice and potentially negligent. Oxygen however does need to be treated with the same consistency as other medications (i.e. paracetamol, intravenous fluids).
Gaps in knowledge were identified in relation to the optimal target saturation level (based on the TSANZ guideline) for fictitious patient scenarios. For the COPD patient scenario, our results were similar to those found by O’Driscoll et al35 where 65.6% of clinicians correctly identified a target saturation range of 88–92%. For the case where the patient is admitted with asthma, the TSANZ guideline16 recommends a range of 92–96% in “other acute medical conditions” but also states “there is an evidence base for titration of oxygen therapy to a target SpO2 range of 93–95% in acute severe asthma … ” (p1188). The options listed in the survey were 88%-92%, 90%-94%, >92%, >94% and >95%. Of these >94% is the only one that is reflective of the background evidence presented in this guideline by the TSANZ. Yet only a quarter of respondents chose this response. The final case scenario was an 81-year-old obese man who smoked, placing him at risk of hypercapnia. Most clinicians did not identify that this patient was at risk of carbon dioxide (CO2) retention and chose saturations levels that may have resulted in him receiving too much oxygen. We acknowledge that there are no specific recommendations that discuss obesity (aside from identifying that obesity hyperventilation syndrome is associated with chronic respiratory failure) or smoker status in the TSANZ guideline.16 However, the BTS advises that those with morbid obesity be treated in a similar manner to those with COPD.9 This is a potential area where further guidance could be given. Considering that more than 31% of Australians are obese,36 with a growing trend towards an overweight and obese society, further education on the pulmonary risk factors associated with obesity is prudent.
Across all four case studies, the average response rate that most closely reflected the TSANZ guideline was 37%. This is significantly lower than the average reported by O’Driscoll et al.35 Clinicians in their study achieved an average correct answer rate of 70%. Authors acknowledged that clinicians in the areas surveyed may have been better informed than was typical due to a drive to optimize oxygen therapy locally.35 A number of previous studies37–39 have demonstrated gaps in knowledge of health-care staff in relation to various aspects of oxygen therapy. Johnson et al40 examined the TSANZ oxygen guideline, listing 15 individual areas where knowledge would be necessary to provide best care to patients receiving oxygen therapy. While this paper was directed at nursing staff, it would not be unreasonable to draw parallels to other clinical specialties. All health-care professionals who administer, monitor or care for patients who require oxygen therapy should have a high level of skill and knowledge when using oxygen, particularly considering the large number of patients who receive this therapy.1,2 Efforts to improve knowledge and skill are a priority.
We recognize that the educational background and expertise vary greatly between different clinical groups and consideration of these differences may be prudent when guideline development and dissemination is undertaken to provide more specific and focused information. Producing guideline documents that target various clinical groups and stakeholders by providing discipline-specific summaries (as the Stroke Foundation41 of Australia have done) could be considered.
Most barriers and facilitators uncovered in this study fell under the ‘care provider’ category, highlighting that efforts to improve the uptake of this and other guidelines should focus on clinicians themselves. Barriers related to difficulties in getting doctors to prescribe oxygen therapy and in getting nurses to administer and monitor those with oxygen therapy. It was also identified that oxygen was not considered or treated with the same care as other drugs. Cousins et al13 have previously highlighted the low rates of oxygen prescription and discussed the challenges for increasing prescription rates in clinical practice. Heartshorne et al42 demonstrated sustained improvements in rates of oxygen prescription during their pilot study that utilized multiple methods designed to improve practice. Similar strategies need to be implemented across Australia to encourage change in doctor’s prescription practices and improve administration and monitoring by nursing staff.
Most clinicians believe that they are adequately trained, which would facilitate the implementation of the TSANZ guideline. However, these results are not necessarily supported by the answers given in the clinical scenarios. Nonetheless, almost a quarter of surveyed clinicians believe they had not been or were unsure if they were adequately trained in the use of oxygen therapy and that the concepts within the TSANZ guideline differed from those taught during basic training. This points to areas for improvement in clinician training at both the undergraduate and postgraduate levels. Most staff agreed that this guideline was a good starting point for self-study, and consideration could be given to developing structured and intentional learning material that may facilitate guideline dissemination and contribute towards staff learning activities and the accumulation of the mandatory continuing professional development points required for ongoing health professional registration in Australia. This is an important point when considering implementation of new knowledge. Merely providing information is not enough. Guidelines require a multifaceted dissemination pathway for adequate uptake,43 and focus needs to be placed on this aspect of knowledge exchange.
Most barriers and facilitators aligned across the professional groups. There were a number of exceptions worth noting; both nurses and doctors indicated that nurses do not administer or monitor oxygen with enough care; however, paramedics and physiotherapists disagreed with this statement. This is not a surprising finding considering nurses and doctors would have more day to day involvement in ensuring the patients under their care are receiving appropriate oxygen therapy. The second barrier where there was discordance among the professional groups was to the statement “It is difficult to provide evidence-based care to patients who do not know what their diagnosis is.” Overall, 44% agreed while 40% disagreed with this statement; however, far more doctors disagreed with this statement (52%) when compared to those who agreed (32%). Considering doctors are responsible for the diagnosis of a patient’s medical condition, a patient’s inability to state their diagnosis understandably does not appear to provide a barrier to treatment for doctors. Items to note where differences were demonstrated for the facilitators between the clinical groups were with the statement “The TSANZ oxygen guideline … does not fit into my ways of working in practice.” Paramedics indicated that they neither agreed nor disagreed when compared to other clinicians who disagreed. The second item where differences were demonstrated where with the statement “working with the TSANZ guideline … is too time consuming.” Nurses and physiotherapists disagreed with this statement while the majority of doctors and paramedics responded that they neither agreed nor disagreed indicating that they were unsure about this question (Table S1 – Supplement 1).
This study has strengths and limitations. To our knowledge, it is the only Australian study that has captured views from a variety of clinical groups and explored the beliefs and attitudes to the prescription of oxygen therapy and the barriers and facilitators for using the TSANZ oxygen guideline. We acknowledge that health-care professional education, expertise and perspectives vary greatly between specialties and that the generic nature of the survey may have missed pertinent data relating more specifically to individual professional groups. However, each of these specialties administers and/or prescribes oxygen therapy in clinical settings in Australia and we believe that questions were broad enough to capture beliefs and attitudes of these different clinicians, and where differences exist these have been highlighted. While the small cohort presents limitations, particularly in that it may not be representative of clinicians views outside of Australia or those who work outside of respiratory medicine, the large body of evidence related to poor practice in relation to oxygen therapy suggests that these views may be more widely spread that what we have been able to capture.
Our data support those of other studies that have demonstrated that there is scope to improve the knowledge of various factors in relation to oxygen therapy and the appropriate amounts of oxygen that are administered to various patient groups. Clinicians overwhelmingly believed that oxygen was a drug and should be treated like other drugs. However, many did not treat oxygen with the same level of care or caution as they did other commonly used medications like antibiotics or IV fluids. Further studies in this area would shed light on why such wide variations exist in relation to the actions of clinicians when administering different medications.
Disclosure
Joyce L Cousins reports this research was supported by an Australian Government Research Training Program Scholarship. Sarah A Hiles’ salary has previously been supported by grants from GSK and AstraZeneca awarded to the University of Newcastle, outside the submitted work. Vanessa McDonald reports grants, personal fees from GSK, grants, personal fees from AstraZeneca, and personal fees from Menarini, outside the submitted work. The authors report no other potential conflicts of interest in this work. The abstract of this paper was accepted for oral poster presentation at the TSANZSRS Annual Scientific Meeting 2020 (postponed due to COVID-19). The abstract was published online as “TSANZ20 Poster Abstracts” in Respirology: https://onlinelibrary.wiley.com/doi/abs/10.1111/resp.13778.
References
1. Eastwood GM, Peck L, Young H, Prowle J, Jones D, Bellomo R. Oxygen administration and monitoring for ward adult patients in a teaching hospital. Intern Med J. 2011;41(11):784–788. doi:10.1111/j.1445-5994.2010.02286.x
2. Pretto JJ, McDonald VM, Wark PA, Hensley MJ. Multicentre audit of inpatient management of acute exacerbations of chronic obstructive pulmonary disease: comparison with clinical guidelines. Intern Med J. 2011;42(4):380–387. doi:10.1111/j.1445-5994.2011.02475.x
3. Australia Institute of Health and Welfare. Admitted Patient Care 2017–2018: Australian Hospital Statistics. Health Services Series No. 90. HSE 225. Canberra: AIHW; 2019.
4. GOLD. Global Strategy for the Diagnosis, Prevention, and Management of Chronic Obstructive Pulmonary Disease. (2019 Report). Global Initiative for Chronic Obstructive Lung Disease, Inc; 2019.
5. Yang IA, Brown JL, George J, et al. The COPD-X Plan: Australian and New Zealand Guidelines for the Management of Chronic Obstructive Pulmonary Disease 2019. Lung Foundation Australia; 2019.
6. Susanto C, Thomas PS. Assessing the use of initial oxygen therapy in chronic obstructive pulmonary disease patients: a retrospective audit of pre-hospital and hospital emergency management. Intern Med J. 2015;45(5):510–516. doi:10.1111/imj.12727
7. Roberts CM, Lopez-Campos JL, Pozo-Rodriguez F, Hartl S. European hospital adherence to GOLD recommendations for chronic obstructive pulmonary disease (COPD) exacerbation admissions. Thorax. 2013;68(12):1169–1171. doi:10.1136/thoraxjnl-2013-203465
8. Kelly AM, Holdgate A, Keijzers G, et al. Epidemiology, treatment, disposition and outcome of patients with acute exacerbation of COPD presenting to emergency departments in Australia and South East Asia: an AANZDEM study. Respirology. 2018;23(7):681–686. doi:10.1111/resp.13259
9. O’Driscoll B, Howard L, Earis J, et al.; on behalf of the British Thoracic Society Emergency Oxygen Guideline Group. BTS guideline for oxygen use in adults in healthcare and emergency settings. Thorax. 2017;72(Supp1):ii1–ii90.
10. Austin MA, Willis KE, Blizzard L, Walters EH, Wood-Baker R. Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trial. BMJ. 2010;341:c5462. doi:10.1136/bmj.c5462
11. Cameron L, Pilcher J, Weatherall M, Beasley R, Perrin K. The risk of serious adverse outcomes associated with hypoxaemia and hyperoxaemia in acute exacerbations of COPD. Postgrad Med J. 2012;88(1046):684–689. doi:10.1136/postgradmedj-2012-130809
12. Chu DK, Kim LHY, Young PJ, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. 2018;391(10131):1693–1705. doi:10.1016/S0140-6736(18)30479-3
13. Cousins JL, Wark PAB, McDonald VM. Acute oxygen therapy: a review of prescribing and delivery practices. Int J Chron Obstruct Pulmon Dis. 2016;11:1067–1075. doi:10.2147/COPD.S103607
14. Clinical Excellence Commission. Between the flags. 2020. Available from: http://cec.health.nsw.gov.au/keep-patients-safe/Deteriorating-patients/between-the-flags.
15. Clinical Excellence Commission. Standard adult general observation chart. patient safety programs [between the flags]. 2017. Available from: http://www.cec.health.nsw.gov.au/__data/assets/pdf_file/0012/258699/sago-221113-watermark.pdf.
16. Beasley R, Chien J, Douglas J, et al. Thoracic society of Australia and New Zealand oxygen guidelines for acute oxygen use in adults: ‘swimming between the flags’. Respirology. 2015;20(8):1182–1191. doi:10.1111/resp.12620
17. Eastabrooks CA. The Alberta Context Tool (ACT). 2007.
18. Funk SG, Champagne MT, Wiese RA, Tornquist EM. BARRIERS: the barriers to research utilization scale. Appl Nurs Res. 1991;4(1):39–45. doi:10.1016/S0897-1897(05)80052-7
19. McCormack B, McCarthy G, Wright J, Slater P, Coffey A. Development and testing of the Context Assessment Index (CAI). Worldviews Evid Based Nurs. 2009;6(1):27–35. doi:10.1111/j.1741-6787.2008.00130.x
20. Peters MAJ, Harmsen M, Laurant MGH, Wensing M. Ruimte Voor Verandering? Knelpunten En Mogelijkheden Voor Verandering in De Patiëntenzorg [Room for Improvement? Barriers to and Facilitators for Improvement of Patient Care]. Nijmegen: Centre for Quality of Care Research (WOK) Radboud University Nijmegen Medical Centre; 2002.
21. Czaja R, Blair J. Designing Surveys. A Guide to Decisions and Procedures.
22. Liamputtong P, ed. Research Methods in Health.
23. Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet. 2003;362(9391):1225–1230. doi:10.1016/S0140-6736(03)14546-1
24. Abernethy AP, Currow DC, Frith P, Fazekas BS. Prescribing palliative oxygen: a clinician survey of expected benefit and patterns of use. Palliat Med. 2005;19(2):168–170. doi:10.1177/026921630501900219
25. Barr RG, Celli BR, Martinez FJ, et al. Physician and patient perceptions in COPD: the COPD resource network needs assessment survey. Am J Med. 2005;118(12):
26. Kelly CA, Lynes D, O’Brien MR, Shaw B. A wolf in sheep’s clothing? Patients’ and healthcare professionals’ perceptions of oxygen therapy: an interpretative phenomenological analysis. Clin Respir J. 2018;12(2):616–632. doi:10.1111/crj.12571
27. Helmerhorst HJF, Schultz MJ, van der Voort PHJ, et al. Self-reported attitudes versus actual practice of oxygen therapy by ICU physicians and nurses. Ann Intensive Care. 2014;4(1):23. doi:10.1186/s13613-014-0023-y
28. Mao C, Wong DT, Slutsky AS, Kavanagh BP. A quantitative assessment of how Canadian intensivists believe they utilize oxygen in the intensive care unit. Crit Care Med. 1999;27(12):6. doi:10.1097/00003246-199912000-00033
29. Eastwood GM, Reade MC, Peck L, Baldwin I, Considine J, Bellomo R. Critical care nurses’ opinion and self-reported practice of oxygen therapy: a survey. Aust Crit Care. 2012;25(1):23–30. doi:10.1016/j.aucc.2011.05.001
30. Small D, Duha A, Wieskopf B, et al. Uses and misuses of oxygen in hospitalized patients. Am J Med. 1992;92:591–595. doi:10.1016/0002-9343(92)90775-7
31. Wijesinghe M, Shirtcliffe P, Perrin K, et al. An audit of the effect of oxygen prescription charts on clinical practice. Postgrad Med J. 2010;86(1012):89–93. doi:10.1136/pgmj.2009.087528
32. Gunathilake R, Lowe D, Wills J, Knight A, Braude P. Implementation of a multicomponent intervention to optimise patient safety through improved oxygen prescription in a rural hospital. Aust J Rural Health. 2014;22(6):328–333. doi:10.1111/ajr.12115
33. Holbourn A, Wong J. Oxygen prescribing practice at Waikato Hospital does not meet guideline recommendations. Intern Med J. 2014;44(12a):1231–1234. doi:10.1111/imj.12602
34. Walters G, Nadeem S. Improving acute oxygen prescription in a respiratory care unit. Qual Saf Health Care. 2009;18(6):512. doi:10.1136/qshc.2008.029561
35. O’Driscoll BR, Bakerly ND, Caress AL, et al. A study of attitudes, beliefs and organisational barriers related to safe emergency oxygen therapy for patients with COPD (chronic obstructive pulmonary disease) in clinical practice and research. BMJ Open Respir Res. 2016;3(1):e000102. doi:10.1136/bmjresp-2015-000102
36. Australian Bureau of Statistics. Overweight and obesity. 4364.0.55.001 - National Health Survey: first results, 2017–18; 2020. Available from: https://www.abs.gov.au/ausstats/[email protected]/Lookup/by%20Subject/4364.0.55.001~2017-18~Main%20Features~Overweight%20and%20obesity~90.
37. Esposito S, Brivio A, Tagliabue C, et al. Knowledge of oxygen administration, aerosol medicine, and chest physiotherapy among pediatric healthcare workers in Italy. J Aerosol Med Pulm Drug Deliv. 2011;24(3):149–156. doi:10.1089/jamp.2010.0850
38. Ganeshan A, Hon LQ, Soonawalla ZF. Oxygen: can we prescribe it correctly? Eur J Intern Med. 2006;17(5):355–359. doi:10.1016/j.ejim.2006.02.007
39. Smith GB, Poplett N. Knowledge of aspects of acute care in trainee doctors. Postgrad Med J. 2002;78(920):335–338. doi:10.1136/pmj.78.920.335
40. Johnson AM, Smith SMS. Respiratory clinical guidelines inform ward-based nurses’ clinical skills and knowledge required for evidence-based care. Breathe. 2016;12(3):257–266. doi:10.1183/20734735.010816
41. Stroke Foundation. Clinical Guidelines for Stroke Management. Melbourne Australia; 2019.
42. Heartshorne R, Cardell J, O’Driscoll R, Fudge T, Dark P. Implementing target range oxygen in critical care: a quality improvement pilot study. J Intensive Care Soc. 2019;1751143719892784.
43. Grol R. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care. 2001;39(8, Supplement 2):
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
