Back to Journals » Open Access Journal of Sports Medicine » Volume 9
Ulnar collateral ligament injuries of the elbow in female division I collegiate gymnasts: a report of five cases
Authors Nicolette GW, Gravlee JR
Received 12 December 2017
Accepted for publication 8 May 2018
Published 7 September 2018 Volume 2018:9 Pages 183—189
DOI https://doi.org/10.2147/OAJSM.S159624
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Andreas Imhoff
Video S2 is an example of a Yurchenko vault and demonstrates the mechanism of injury for one of the gymnasts.
Views: 586
Guy W Nicolette, Jocelyn R Gravlee
University of Florida, Gainesville, FL, USA
Introduction: Elbow ulnar collateral ligament (UCL) injuries in gymnastics have not been well documented in the literature, in comparison to UCL injuries in baseball. Few studies have examined the mechanism and nonoperative management of this injury, and no studies to date have been published on incidence of injury and return to play recommendations in gymnastics.
Patient case review: A literature search was performed using PubMed to review articles from 1980 to 2016 that addressed the biomechanics of UCL injury in baseball and gymnastics, the anatomy of the elbow, injury rates, surgical vs non-surgical management, rehabilitation, and return to play recommendations for the sport of gymnastics. Five female collegiate gymnasts sustained UCL injury over a 3-year period. Electronic medical records for each case were thoroughly reviewed including imaging, surgical and non-surgical management, rehabilitation, and the progressive return to gymnastics.
Discussion: Four UCL injuries were confirmed by MRI to be avulsions at the distal insertion of the UCL and one was an avulsion at the proximal origin. While less than half of baseball players can return to competition with conservative management of these types of injuries, four out of five gymnasts were able to return to competition with nonoperative management. One gymnast opted to have reconstruction after a successful competition season. Time to return to play varied seemingly dependent on the severity of UCL injury and event.
Conclusion: In our case series, collegiate female gymnasts were able to return to participation with nonoperative treatment of the UCL. Their success in returning to competitive gymnastics may also depend on the event(s) in which they are trying to participate.
Strength of Recommendation Taxonomy: C.
Keywords: elbow ulnar collateral ligament, gymnastics, gymnast
Introduction
Elbow ulnar collateral ligament (UCL) injuries in gymnastics have not been well documented in the literature, in comparison to UCL injuries in baseball, which have been well studied.1–6 No previous studies have examined the mechanism, management, or return to play recommendations for UCL injuries in gymnastics. We report 5 consecutive cases at one institution, approved by the University of Florida institutional review board (IRB) (IRB201300169) as a retrospective chart review with a waiver of patient consent.
A bail is a release move when transitioning from the high bar to the lower bar, landing on the palms of the hands in a handstand position. A round-off is a move that begins much like a cartwheel but the gymnast pivots when his/her feet are in the air to land with both feet simultaneously facing the opposite direction from the start of the move. A dismount is when the gymnast leaves an apparatus by jumping and landing on his/her feet, often combined with other moves (flipping, turning, etc.).
Case 1
A 19-year-old female with no previous history of elbow pain presented for evaluation after performing a bail (an example of a bail Video S1) on the uneven bars during practice and sustaining a valgus load to the right elbow. Physical exam revealed medial elbow tenderness and pain with milking maneuver. MRI arthrogram revealed a complete tear at the insertion of the anterior band of the UCL off the sublime tubercle (Figure 1). She was braced for 4 weeks with an extension block initially and was gradually weaned from the brace over the following 2 weeks. She continued a rehabilitation program for the remainder of the season. She returned to basic gymnastics skills at 4 weeks, and successfully competed at her pre-injury level on the vault and uneven bars that season. At the end of her competitive season, she underwent UCL reconstruction due to continued pain and subjective instability. The athlete began light tumbling at 5 months post-operatively and was cleared for full participation 6 months after reconstruction.
Case 2
A 20-year-old female with a 1-month history of elbow pain presented for evaluation after over-rotating a difficult dismount on the uneven bars during practice. The athlete did not hyperextend her right elbow, although she did have a valgus load at this joint. Physical exam revealed medial elbow tenderness and pain with milking. Valgus malalignment was more prominent on the affected side with the elbow in extension, but no laxity was present. MRI arthrogram revealed a partial tear of the UCL at the distal insertion on the sublime tubercle (Figure 2). Of note, there was also evidence of an old proximal UCL injury with dystrophic mineralization. Because there was no gross laxity, the athlete was taped for practice and competition rather than braced and underwent rehabilitation for the remainder of the season. She returned to basic gymnastics skills in 10 days and eventually returned to her pre-injury level, competing on the uneven bars and balance beam that season.
Case 3
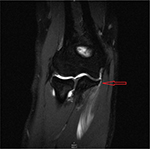
A 19-year-old female with a history of elbow pain presented for evaluation after feeling a “pop” in her right elbow while performing a round-off onto the springboard on vault during practice (a properly performed round-off example is shown in Video S2). Her lead elbow was forced into extension with a valgus load when the injury occurred. Physical exam revealed medial elbow tenderness and pain with milking maneuver. Valgus malalignment was more prominent on the affected side in extension, but no laxity was present. MRI revealed a complete tear of the UCL at the sublime tubercle (Figure 3). She was braced for 4–6 weeks (with an extension block initially) and underwent a rehabilitation program for the remainder of the season. She returned to basic gymnastics skills in 6 weeks and competed at her pre-injury level on the vault that season. At the athlete’s 12-week follow-up, she reported no pain, but complained of a lack of stability with some maneuvers. Since she was able to perform all of her required elements in the gym, she was advised to continue conservative treatment and taping during activity.
Case 4
A 19-year-old female with no history of elbow pain presented for evaluation after hyperextending her left elbow while performing a bail on the uneven bars. Physical exam revealed medial elbow pain with extension and with milking maneuver. Valgus laxity was evident on examination. MRI revealed a high-grade partial tear of the UCL at the proximal origin (Figure 4). Of note, there was also evidence of a remote avulsion injury at the sublime tubercle. The distal fibers of the UCL were intact. She was braced for 6 weeks (including gradual progression out of the brace in the final 2 weeks) with full range of motion and underwent a rehabilitation program for the remainder of the season. She returned to basic gymnastics skills at 4 weeks and competed at her pre-injury level on the vault and floor exercise that season.
Case 5
An 18-year-old female with a 1-month history of elbow pain presented for evaluation after hyperextending her right elbow while performing a bail on the uneven bars. Physical exam revealed pain with extension and with milking maneuver. No laxity was evident on initial examination. MRI revealed complete tear of the UCL at the sublime tubercle (Figure 5). She was braced for 8 weeks (with an extension block initially) and underwent a rehabilitation program. She returned to basic gymnastics skills at 12 weeks but had continued pain and laxity and was unable to compete at her pre-injury level during practice. She was offered surgery but declined. Soon after she broke team rules and was dismissed from the team. Upon exit physical 5 months after injury, she was pain-free with full range of motion and there was no subjective instability with daily activities.
Discussion
The prevalence of UCL injuries in gymnasts is not known. There are three retrospective studies in the literature that discuss surgical outcomes in gymnasts with UCL injury but include sample sizes of 2–4 gymnasts and are not specific about return to play.7–9 One case report has been published on a gymnast with a boney avulsion of the UCL in the elbow after a dislocation.10 Much more, however, is known about UCL injuries of the elbow in the throwing athlete.
Review of anatomy, biomechanics, and comparison to throwers
Anatomy
As with most joints, stability of the elbow relies on passive and active stabilization. The joint capsule and bony structure provide varying amounts of stability depending on elbow position, but the primary passive stabilizers of the elbow are ligamentous. The anterior bundle of the UCL is the primary valgus restraint, particularly in flexion. At 20–70 degrees of flexion, the UCL supplies about 50% of the elbow joint stability.11–14 In full extension, the UCL contributes to only 33% to joint stability, with the remainder splits equally between the capsule and bone.13–15 The radial head provides some valgus stability, particularly in an elbow with attenuation of the UCL.14 Additionally, the radius takes the majority (~60%) of the axial load in extension and even more in the flexed and pronated position.15,16 The olecranon also provides passive valgus restraint, particularly in extension.17
The dynamic valgus stabilizers of the elbow are the flexor carpi ulnaris and the flexor digitorum superficialis, which has shared fibers with the underlying anterior bundle of the UCL. Their relative contribution to valgus stability of the elbow is debated but appears to be small.15,18
Baseball vs gymnastics
The biomechanics of pitching have been studied extensively,11,19–25 whereas in gymnastics, only one author26 has attempted to document ground reaction forces during a back handspring. Fleisig et al showed 64 nM mean elbow valgus stress per baseball pitch in highly skilled adult pitchers,22 while Feltner and Dapena showed 100 nM mean valgus stress in collegiate baseball players.20 Koh et al measured gymnasts producing an average mean valgus stress of 18 nM during the back handspring, but also commented that valgus forces might be equivalent to throwers when normalized for body mass.26 The back handspring in gymnastics is a basic skill that is used in three of the four events (vault, balance beam, and floor exercise) as a transition move, and thus performed multiple times during practice and competition. However, there are numerous skills in gymnastics that may contribute to UCL load that have not been studied, compared with baseball where the throwing mechanism is the primary action that contributes to UCL load. Another obvious difference is sex, given that an overwhelming majority of subjects in studies of baseball throwers are males. Increased carrying angles (ulno-humeral angles) have been shown to be a risk factor in non-traumatic ulnar neuropathy,27 and while there are measurable increases in carrying angle in females compared to males, Goldfarb et al felt these to be of minimal clinical impact.28 It has also been shown that carrying angle increases during childhood years and seems to plateau at ages 14–15 years, but the clinical significance of this is also unknown especially as it relates to UCL injuries.29,30
A large volume of literature describes the involvement and injury pattern of the UCL in throwing athletes.1,11,20,22,26,31–33 Briefly, the late cocking/early acceleration phase of throwing puts a significant, repetitive valgus load on the elbow.11,15,34 Injured throwers are found to have chronically attenuated UCLs with majority (up to 87%) of torn in the midsubstance.35 By contrast, the most common area for UCL injury in gymnastics is not known. One recent article reported the appearance of a degenerative UCL with intrasubstance tears near the humerus in a cohort of three gymnasts.8 However, the mean age of the gymnasts in that study was 15.3 years compared to 19.0 in our series. Four out of the five gymnasts in our study had an acute tear at the UCL distal insertion, while only one had an acute tear at the proximal origin. Interestingly, there were two gymnasts with evidence of an old injury – one occurring at the distal insertion and one occurring at the proximal origin. In our case series, no patient had a midsubstance ligament tear.
Some throwers also have evidence of flexor-pronator injury at the time of surgery.6,35 This repetitive valgus overload can also be responsible for a traction ulnar neuritis, posteromedial impingement, and radiocapitellar damage, all likely being secondary to attenuation of the UCL.33 There was no evidence of such injuries in the five gymnasts studied.
We lack biomechanical data depicting elbow UCL strain forces in gymnastics, but the mechanism of ulnar collateral injury in this group of athletes is drastically different than that in throwing sports. Gymnasts have repetitive upper extremity axial loading, performed with the elbow in near-full extension. Throwers do not experience axial loading but rather sustain repetitive valgus strain, typically in 70–100 degrees of flexion.
The amount of elbow valgus stress force generated by gymnasts doing axial loading skills also appears to differ from throwers. The valgus force across the UCL during a back handspring is the only gymnastics skill that has been studied, and so the overall stress on the UCL of a gymnast daily during practice and competition is unknown. The back handspring is considered a basic transition skill in gymnastics and is performed hundreds of times a day. With most elite gymnasts having started gymnastics by the age of 5–6 years, and competing upward of 15 years, the UCL undergoes repetitive stress daily during critical periods of growth and development. Mandated pitch counts help to minimize chronic injury to the medial elbow in baseball, but there are no such limitations in gymnastics. It is thus unclear why more UCL injuries in gymnasts have not been reported. Perhaps there might be less UCL injury in gymnastic participation because of the increased bony stability in extension (passive stabilization). Additionally, with the skills that gymnasts do on their hands, there may be more radiocapitellar loading in pronation, which has been shown to increase articular contact and therefore provide better bony stability of the joint.16
Anecdotally, a significant percentage of throwers have some elbow pain prior to final UCL injury. Three of our gymnasts reported elbow pain prior to injury; two had chronic changes to the UCL. It is difficult to conclude whether previous elbow pain and injury in our cases had any influence on the final UCL injury. No previous studies on gymnasts are available to shed light on this point, but it might suggest the need for a higher level of suspicion in working up the gymnast with medial elbow pain.
Management of UCL Injury
Nonoperative management of UCL injury has not had favorable outcomes in overhead throwing athletes. A 2001 study, for example, showed only 42% of throwers returning to previous activity level at 25 weeks.36 However, in 2010, Dodson et al showed that nine of 10 UCL-injured National Football League quarterbacks returned to play after nonoperative treatment with a mean return to play at 26 days, highlighting the differences of UCL injury and recovery in non-baseball throwers.37
Since 1981, most studies looking at operative treatment of the UCL have involved male subjects.1,36,38 One retrospective case series involving 19 female athletes (4 gymnasts) reported favorable outcomes after surgical intervention repair vs reconstruction, but was not specific about the details of return to play for the gymnasts included in the study.9 Savoie et al retrospectively evaluated 60 athletes (2 gymnasts) undergoing UCL repair and concluded that primary repair of proximal or distal UCL tears was an acceptable option for non-professional athletes.7 A retrospective chart review on 55 adolescent athletes (3 gymnasts) with a mean age of 17.6 years with UCL insufficiency reported that one gymnast was able to return to her previous high-school level of gymnastics, while the other two gymnasts were not able to return to the sport after UCL reconstruction.8
In our series, four of five gymnasts returned to Division I competition for the remainder of their season with nonoperative management. (Table 1) They all underwent a structured rehabilitation protocol that focused on range of motion, followed by strength progression of the scapular stabilizers, rotator cuff, and the forearm flexor/extensor masses once pain free. Sport-specific strengthening exercises such as push-ups in a handstand were also included later in the rehabilitation process to add the axial loading component of the sport.
  | Table 1 Case summary table Abbreviations: FROM, full range of motion; UCL, ulnar collateral ligament. |
However, the athletes in this series also had varying degrees of UCL injury. Cases 1 and 3 had full thickness tears and ultimately appeared not to have enduring pre-injury stability, despite returning for one season. Case 5 also likely would have ultimately needed reconstruction to return to play, but other circumstances prevented return to competition. The one athlete unable to return to competition at all had the highest grade injury by MRI. Not surprisingly, Cases 2 and 4 with lower grade injuries returned to basic skills and full competition more quickly than those with higher grade injury. Lastly, gymnasts at this level can be event specialists, and so there may be differences in the success of returning to this sport depending to which event(s) the athlete is attempting a return (much like a position player versus a pitcher in baseball). Perhaps skills on the uneven bars create larger loads on the UCL than the skills performed on the other three events, making it more challenging to return to the uneven bars after injury. Further biomechanical study is also warranted. It is unclear whether the carrying angle has any impact on the risk for UCL injury.
Conclusion
The forces across the elbow UCL in gymnastics and baseball may be similar; however, the mechanism of injury is not. This may explain the difference in injury patterns between baseball and gymnastics. Furthermore, the axial loading component in gymnastics seems to add to the stability of the joint, which may play an important role in a gymnast’s ability to the return to pre-injury levels without operative intervention, especially with partial UCL injury. It also appears that some gymnasts may be able to return to competition with full thickness injury; however, there may not be enduring return to pre-injury level and these gymnasts likely warrant stronger consideration for reconstruction at some point.
Management and return to play decisions for UCL injuries of the elbow in gymnastics are complex and involve a thorough evaluation and grading of the injury. It is also important to understand what event(s) the athlete is expecting to return to as some events may cause more stress to the UCL than others. An initial trial of nonoperative management with a structured rehabilitation program seems to be a reasonable approach in the sport of gymnastics.
Disclosure
The authors report no conflicts of interest in this work.
References
Azar FM, Andrews JR, Wilk KE, Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med. 2000;28(1):16–23. | ||
Bruce JR, Hess R, Joyner P, Andrews JR. How much valgus instability can be expected with ulnar collateral ligament (UCL) injuries? A review of 273 baseball players with UCL injuries. J Shoulder Elbow Surg. 2014;23(10):1521–1526. | ||
Ciccotti MG, Atanda A Jr, Nazarian LN, Dodson CC, Holmes L, Cohen SB. Stress sonography of the ulnar collateral ligament of the elbow in professional baseball pitchers: a 10-year study. Am J Sports Med. 2014;42(3):544–551. | ||
Hechtman KS, Zvijac JE, Wells ME, Botto-van Bemden A. Long-term results of ulnar collateral ligament reconstruction in throwing athletes based on a hybrid technique. Am J Sports Med. 2011;39(2):342–347. | ||
Jones KJ, Conte S, Patterson N, ElAttrache NS, Dines JS. Functional outcomes following revision ulnar collateral ligament reconstruction in Major League Baseball pitchers. J Shoulder Elbow Surg. 2013;22(5):642–646. | ||
Koh JL, Schafer MF, Keuter G, Hsu JE. Ulnar collateral ligament reconstruction in elite throwing athletes. Arthroscopy. 2006;22(11):1187–1191. | ||
Savoie FH 3rd, Trenhaile SW, Roberts J, Field LD, Ramsey JR. Primary repair of ulnar collateral ligament injuries of the elbow in young athletes: a case series of injuries to the proximal and distal ends of the ligament. Am J Sports Med. 2008;36(6):1066–1072. | ||
Jones KJ, Dines JS, Rebolledo BJ, et al. Operative management of ulnar collateral ligament insufficiency in adolescent athletes. Am J Sports Med. 2014;42(1):117–121. | ||
Argo D, Trenhaile SW, Savoie FH 3rd, Field LD. Operative treatment of ulnar collateral ligament insufficiency of the elbow in female athletes. Am J Sports Med. 2006;34(3):431–437. | ||
Grumet RC, Friel NA, Cole BJ. Bony avulsion of the medial ulnar collateral ligament in a gymnast: a case report. J Shoulder Elbow Surg. 2010;19(7):e1–e6. | ||
Loftice J, Fleisig GS, Zheng N, Andrews JR. Biomechanics of the elbow in sports. Clin Sports Med. 2004;23(4):519–530, vii–viii. | ||
Morrey BF. Acute and chronic instability of the elbow. J Am Acad Orthop Surg. 1996;4(3):117–128. | ||
Morrey BF, An KN. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983;11(5):315–319. | ||
Morrey BF, Tanaka S, An KN. Valgus stability of the elbow. A definition of primary and secondary constraints. Clin Orthop Relat Res. 1991;(265):187–195. | ||
Alcid JG, Ahmad CS, Lee TQ. Elbow anatomy and structural biomechanics. Clin Sports Med. 2004;23(4):503–517, vii. | ||
Morrey BF, An KN, Stormont TJ. Force transmission through the radial head. J Bone Joint Surg Am. 1988;70(2):250–256. | ||
An KN, Morrey BF, Chao EY. The effect of partial removal of proximal ulna on elbow constraint. Clin Orthop Relat Res. 1986;(209):270–279. | ||
Lin F, Kohli N, Perlmutter S, Lim D, Nuber GW, Makhsous M. Muscle contribution to elbow joint valgus stability. J Shoulder Elbow Surg. 2007;16(6):795–802. | ||
Chu Y, Fleisig GS, Simpson KJ, Andrews JR. Biomechanical comparison between elite female and male baseball pitchers. J Appl Biomech. 2009;25(1):22–31. | ||
Feltner M, Dapena J. Dynamics of the shoulder and elbow joints of the throwing arm during a baseball pitch. Int J Sports Biomech. 1986;2(4):235–259. | ||
Fleisig G, Chu Y, Weber A, Andrews J. Variability in baseball pitching biomechanics among various levels of competition. Sports Biomech. 2009;8(1):10–21. | ||
Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23(2):233–239. | ||
Fleisig GS, Barrentine SW, Zheng N, Escamilla RF, Andrews JR. Kinematic and kinetic comparison of baseball pitching among various levels of development. J Biomech. 1999;32(12):1371–1375. | ||
Pappas AM, Zawacki RM, Sullivan TJ. Biomechanics of baseball pitching. A preliminary report. Am J Sports Med. 1985;13(4):216–222. | ||
Sisto DJ, Jobe FW, Moynes DR, Antonelli DJ. An electromyographic analysis of the elbow in pitching. Am J Sports Med. 1987;15(3):260–263. | ||
Koh TJ, Grabiner MD, Weiker GG. Technique and ground reaction forces in the back handspring. Am J Sports Med. 1992;20(1):61–66. | ||
Chang CW, Wang YC, Chu CH. Increased carrying angle is a risk factor for nontraumatic ulnar neuropathy at the elbow. Clin Orthop Relat Res. 2008;466(9):2190–2195. | ||
Goldfarb CA, Patterson JM, Sutter M, Krauss M, Steffen JA, Galatz L. Elbow radiographic anatomy: measurement techniques and normative data. J Shoulder Elbow Surg. 2012;21(9):1236–1246. | ||
Yilmaz E, Karakurt L, Belhan O, Bulut M, Serin E, Avci M. Variation of carrying angle with age, sex, and special reference to side. Orthopedics. 2005;28(11):1360–1363. | ||
Balasubramanian P, Madhuri V, Muliyil J. Carrying angle in children: a normative study. J Pediatr Orthop B. 2006;15(1):37–40. | ||
Cain EL Jr, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38(12):2426–2434. | ||
Dines JS, Jones KJ, Kahlenberg C, Rosenbaum A, Osbahr DC, Altchek DW. Elbow ulnar collateral ligament reconstruction in javelin throwers at a minimum 2-year follow-up. Am J Sports Med. 2012;40(1):148–151. | ||
Hariri S, Safran MR. Ulnar collateral ligament injury in the overhead athlete. Clin Sports Med. 2010;29(4):619–644. | ||
Ben Kibler W, Sciascia A. Kinetic chain contributions to elbow function and dysfunction in sports. Clin Sports Med. 2004;23(4):545–552, viii. | ||
Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74(1):67–83. | ||
Rettig AC, Sherrill C, Snead DS, Mendler JC, Mieling P. Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes. Am J Sports Med. 2001;29(1):15–17. | ||
Dodson CC, Slenker N, Cohen SB, Ciccotti MG, DeLuca P. Ulnar collateral ligament injuries of the elbow in professional football quarterbacks. J Shoulder Elbow Surg. 2010;19(8):1276–1280. | ||
Vitale MA, Ahmad CS. The outcome of elbow ulnar collateral ligament reconstruction in overhead athletes: a systematic review. Am J Sports Med. 2008;36(6):1193–1205. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.