Back to Journals » Neuropsychiatric Disease and Treatment » Volume 12
Two-year prognosis after residential treatment for patients with alcohol dependence: three chief guidelines for sobriety in Japan
Authors Cho T , Negoro H, Saka Y, Morikawa M, Kishimoto T
Received 23 April 2016
Accepted for publication 17 June 2016
Published 5 August 2016 Volume 2016:12 Pages 1983—1991
DOI https://doi.org/10.2147/NDT.S111230
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Taro Kishi
Tetsuji Cho,1,2 Hideki Negoro,3 Yasuhiro Saka,1 Masayuki Morikawa,1,2 Toshifumi Kishimoto2
1Mie Prefectural Mental Care Center, Tsu-Shi, Mie, 2Department of Psychiatry, Nara Medical University School of Medicine, Kashihara, Nara, 3Faculty of Education, Nara University of Education, Nara, Japan
Background: In Japan, the three chief traditional guidelines for sobriety (3CGS) are regular medical checkups, participation in self-help groups, and pharmacotherapy with antidipsotropics. However, the official record of the origins of 3CGS is not clear. The aim of this current study was to assess 3CGS by an examination of the prognosis of patients with alcohol dependence 2 years after their discharge from a residential treatment program.
Subjects and methods: The association between subjects’ abstinence from alcohol and their regular medical checkups, participation in self-help groups, and treatment with antidipsotropics were prospectively examined. Two years after discharge, the relationship between the 3CGS compliance and abstinence rates was investigated as the primary outcome. In addition, the following were examined as secondary outcomes: the time taken till the first drink after discharge, whether the participants were readmitted to residential treatment, the number of days to readmission, the number of heavy drinking days, and recovery.
Results: A total of 98 patients participated. The perfect and partial abstinence rates for patients who followed all the principles of 3CGS were significantly higher than those for patients who followed no guidelines (P<0.05 and P<0.01, respectively). The perfect abstinence rates for patients who had continued attending checkup sessions (P<0.001) and who were taking antidipsotropics (P<0.05) were significantly higher than those for patients who did not follow these components of 3CGS. However, the perfect abstinence rates were not higher for patients who had continued to participate in self-help groups. In addition, the perfect abstinence rate was statistically associated with regular medical checkups (adjusted odds ratio =5.33, 95% confidence interval =1.35–21.0) and participation in self-help groups (adjusted odds ratio =3.79, 95% confidence interval =1.17–12.3).
Conclusion: This study, reports the effectiveness of 3CGS for the first time. The recovery rate of alcoholics 2 years after discharge from residential treatment was examined. However, due to the chronic nature of alcoholism, further studies are required to investigate the efficacy of 3CGS beyond 2 years.
Keywords: alcohol dependence, three chief guidelines for sobriety (3CGS), disulfiram, self-help group, recovery
Introduction
Alcohol dependence, which is characterized by “loss of control”, is a chronic relapsing disorder similar to diabetes or hypertension.1 It has a considerable component of genetic susceptibility and is also influenced by environmental factors.2 Therefore, long-term maintenance therapy is very important. We should recognize redrinking by alcoholics as a symptom such as relapse in cancer or re-injury of a joint sprain. In addition, we have to take into account not only the abstinence from alcohol but also the recovery of quality of life. The prognosis of alcoholism is more influenced by social–psychological factors of the patient than by therapeutic interventions.3 The first study4 about the prognosis of alcoholism in Japan found that a good prognosis was related more strongly to social factors than physical factors. In particular, the continuation of therapy was strongly related to a good prognosis. However, there are only a few studies in Japan on the factors associated with a good prognosis.
The three chief traditional guidelines for sobriety (3CGS) in Japan are regular medical checkups, participation in self-help groups, and therapy with antidipsotropics.5 3CGS have been extensively used in the treatment of alcohol dependence in Japan.
However, the official record of the origins of 3CGS is not clear. Prospective evidence to support these guidelines has been obtained abroad, but they have not been extensively studied in Japan.
With regard to the first guideline, alcoholics tend to discontinue attending medical checkups. Baekeland and Lundwall6 reported that 57%–75% of outpatients dropped out before the fourth consultation. In addition, Scivoletto et al7 reported that a half or more number of patients stopped attending consultations within several months, and only 16% continued attending checkup sessions for 1 year after the first consultation. On the other hand, continuing to attend medical checkups is strongly related to a good prognosis.8
Similarly, in Japan, more than half of the patients with alcoholism stopped attending medical checkups within 6 months, and only 21.1% of patients were seen 1 year after their first consultation.9 Japanese patients with alcoholism who continued therapy had a significantly higher rate of abstinence after 1 year, indicating that continued attendance of checkup sessions is strongly related to abstinence.4
Many studies support the usefulness of the second guideline, participation in self-help groups. For example, the rate of abstinence of those who participate in alcoholics anonymous (AA) is approximately twice that of those who do not participate in any self-help group.10 In Japan, research has supported the usefulness of Dansyukai (a traditional Japanese self-help group). Suzuki3 reported that membership in Dansyukai had a significant impact on treatment outcome. In addition, Nishikawa11 reported that continued participation in self-help groups is related to a significantly higher rate of continuing to attend checkup sessions.
The effectiveness of abstinence with using antidipsotropics has not been evaluated via double-blind, randomized controlled trials in Japan. In a questionnaire study12 in Japan, 86% of specialists responded that antidipsotropics should be taken for <1 year. However, research on the ideal duration of antidipsotropic usage is lacking. According to Japanese guidelines for the treatment of alcoholism and related disorders,13 “psychotherapy is more important than the effects of antidipsotropics, and there are many differences in the efficacy of antidipsotropics between facilities and researchers”. However, no mention is made of a recommended period of antidipsotropic usage. In addition, naltrexone, nalmefene, and acamprosate were not registered in Japan during the research period. Many reports support the effectiveness of disulfiram14–20 and cyanamide,21 but compliance to the administration regimen is also important.22 Diehl et al16 reported that disulfiram is more effective than acamprosate, particularly in patients with a long duration of alcohol dependence, and Berglund14 reported evidence from a meta-analysis of a possible additive effect for naltrexone as well as for aversive treatment (disulfiram) in alcohol dependence.
The aim of the current study was to assess 3CGS by an examination of the prognosis of patients with alcohol dependence 2 years after their discharge from a residential treatment program.
Subjects and methods
Participants
Subjects recruited for this prospective study were patients with alcohol dependence, who were diagnosed according to the criteria of the International Statistical Classification of Diseases, tenth revision,23 and the Diagnostic and Statistical Manual of Mental Disorders, fourth edition,24 and who were hospitalized in the Mental Care Center, Prefecture of Mie, Japan. Subjects were admitted between November 2007 and August 2008. Participants were recruited within 2 weeks of admission after a period of withdrawal symptoms. The exclusion criteria for this study were any of the following at the time of recruitment: severe episode of a depressive or manic mood, diagnosis of dementia, psychomotor excitement, compulsory admission, pregnancy, or severe liver, kidney, or cardiac dysfunction. Of the 117 patients who we attempted to recruit for this study, 15 fell under the exclusion criteria, two refused our request, and two dropped out after entry because they felt something troublesome to cooperate this research. A total of 98 patients participated. The mean term of residential treatment was 74.6 days (standard deviation [SD], ±28.7). In residential treatment, the participants received psychotherapy, pharmacotherapy, group therapy, kinesitherapy, and motivation enhancement therapy. To keep identities of the participants in the clinical settings, the participant could select to follow each chief guideline before discharge. Therefore, we decided to assign them to each chief guideline groups at their discharge.
To prospectively examine the association between subjects’ abstinence from alcohol and their attendance at medical checkups, participation in self-help groups, and treatment with antidipsotropics, we obtained permission to interview each participant by telephone 2 years after discharge, even if the participant had stopped attending medical checkups or had only irregularly attended. Participants were told that they could withdraw from the study at any time.
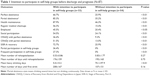
We were able to interview 74.5% of the original participants 2 years after discharge. Two subjects dropped out, eleven had unknown results, and 14 died. We excluded these 14 from the evaluation. However, we included them in the second analysis: the comparison of intention to participate in self-help groups before discharge and prognosis (Table 1) and antidipsotropics consumption before discharge and 2 years after discharge (Table 2). The mean age at death was 54.4 years (SD ±10.9).
Assessment of outcome
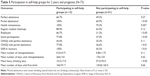
At baseline, we obtained information on age, sex, family medical history, educational level, age at first drink, age at onset of alcoholism, duration of drinking habit, first time in residential treatment or not, and cross-addictions. In addition, mean corpuscular volume as well as blood levels of aspartate aminotransferase, alanine aminotransferase, and gamma-glutamyl transferase was measured (carbohydrate-deficient transferrin was not registered in Japan). Participants were also tested for brain atrophy. Computed tomography scans were assessed by a trained psychiatrist and radiologist, and we recognized “positive brain atrophy” only if the opinions of both experts matched. Table 3 shows information about the participants upon admission to the study.
Before participants were discharged from residential treatment, we asked about their intentions to participate in self-help groups and checked whether they were taking antidipsotropics.
The criterion for continuation of medical checkup is at least once within a month. Two years after discharge, we investigated the relationship between 3CGS compliance and abstinence rates as the primary outcome. In addition, we examined the following as secondary outcomes: the time to first drink after discharge, whether participants were readmitted to residential treatment, the number of days to readmission, the number of heavy drinking days, self-assessed health maintenance, employment status, social participation (voluntary participation and contribution to the community through attendance at school, self-help group, and vocational aid center; volunteer activity), and recovery that is defined in detail in the following sections. There is a custom of checking about heavy drinking as an indicator of the severity of redrinking in Japan. Outcomes were evaluated by psychiatrist by asking face-to-face. Participants were interviewed by telephone 2 years after discharge even if they had stopped attending checkup sessions.
We trusted the patients’ self-reports for the number of days to redrinking corroborated, if possible and with patients’ permission, with information about drinking from families and medical attendants. The degree of abstinence was divided into two categories: “perfect abstinence”, which was defined as no drinking of alcohol, and “partial abstinence”, which was defined as drinking several times but not drinking continuously during the 2 years since discharge. We utilized the definition of the Ministry of Health, Labour, and Welfare in Japan25 of “heavy drinking” as drinking >60 g of alcohol per day.
Recovery was evaluated by the Japanese version of the Self-Identified Stage of Recovery, Part A (SISR-A).26 A patient was defined as having achieved “SISR-A recovery” if he/she had reached the rebuilding or growth stages of recovery. A second measure of recovery (Criteria of Recovery from Alcohol and Drug Dependence in Japan, CRADJ) utilized the criteria from a previous study27 and from the Betty Ford Institute Consensus Panel,28 which defined recovery as “a voluntarily maintained lifestyle characterized by sobriety, personal health, and citizenship”. We used the Betty Ford Institute’s criteria of sobriety and personal health, but we expanded their definition of citizenship from voluntary contributions to the community through working and school attendance to include also the participation in self-help groups or vocational aid center and other volunteer activities. In brief, we judged a patient to have achieved CRADJ recovery if he/she exhibited sobriety (perfect abstinence or partial abstinence), personal health, and citizenship.
Participation in self-help groups was also divided into two categories: “frequent participation”, in which the participant attended most meetings, and “partial participation”, in which the participant attended at least half of the meetings. Only patients in the “frequent participation” category could be said to meet the criteria of 3CGS. Participants were defined as attending regular medical checkups only if they had been attending continuously for 2 years. Finally, we analyzed the relationship between prognosis and each guideline of 3CGS.
The ethics committee of the Mental Care Center, Prefecture of Mie, approved this study, and all subjects provided written consent.
Statistical analysis
Statistical procedures used depended on the conditions of the different 3CGS guidelines. We performed t-tests for continuous variables with an approximately normal distribution (mean number of rehospitalization, mean number of days until rehospitalization, mean heavy drinking days, and mean number of days until first drink) and χ2 tests for categorical variables (perfect and partial abstinence, health maintenance, employed social participation, CRADJ with perfect and partial abstinence, SISR-A recovery, partial and participation in self-help groups, health maintenance, regular medical checkups, employed, and social participation).
In addition, logistic regression analysis was used to evaluate the association between perfect abstinence rate and each chief guideline. Age, sex, and each chief guideline were then mutually adjusted (adjusted odds ratio, AOR) using a forced entry method.
All statistical tests were two tailed, and the significance level was set at 0.05. All statistical analyses were carried out with SPSS® Statistics 17.0 software (SPSS Inc., Chicago, IL, USA).
Results
The perfect abstinence rate 2 years after discharge was 36.7% (36 of 98 participants). The perfect and partial abstinence rates for the patients who followed all the principles of 3CGS were significantly higher than those for patients who did not follow any of the three guidelines (P<0.05 and P<0.01, respectively). However, only six patients followed the 3CGS perfectly.
In the logistic regression analyses between perfect abstinence rate and each guideline, perfect abstinence rate was statistically associated with regular medical checkups (AOR =5.33, 95% confidence interval =1.35–21.0) and participation to self-help group (AOR =3.79, 95% confidence interval =1.17–12.3).
Table 4 shows the attendance of medical checkups and prognosis. The perfect and partial abstinence rates, and some indicators, for patients who had attended checkup sessions were significantly higher than those for patients who had discontinued attendance. In addition, patients who had been regularly attending medical checkups were rehospitalized significantly more number of times.
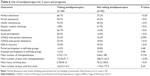
Table 5 shows the participation in self-help groups and prognosis. The partial abstinence rates for patients who participated in self-help groups were significantly higher than those for patients who did not participate.
Table 6 shows the use of antidipsotropics (28 had taken disulfiram and two had taken cyanamide) after discharge and prognosis. The perfect and partial abstinence and regular attendance of checkup sessions for patients who had been taking antidipsotropics were significantly higher than those for patients who had not been taking antidipsotropics. We did not receive any reports of severe side effects from the use of antidipsotropics for 2 years.
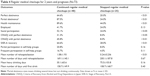
For patients who were administered antidipsotropics before discharge, the rates of perfect and partial abstinence, regular attendance of checkup sessions, partial participation in self-help groups were significantly higher than those for patients who were not administered antidipsotropics before discharge (Table 2).
The perfect abstinence rates for patients who had continued regular medical checkups (P<0.001) and who were taking antidipsotropics (P<0.05) were significantly higher than those for patients who did not follow these components of 3CGS (Tables 4 and 6).
The partial abstinence rates for patients who had continued attending checkup sessions (P<0.001), who had participated in self-help groups (P<0.05), and who were taking antidipsotropics (P<0.001) were significantly higher than those for patients who did not follow any of the components of 3CGS (Tables 4–6).
Discussion
The results of this study indicate that 3CGS can enhance abstinence and recovery rates for at least 2 years after discharge from residential treatment. The logistic regression analyses also supported the effectiveness of regular medical checkups and participation in self-help groups. However, only six patients followed the 3CGS perfectly. Therefore, 3CGS is not only effective but also very difficult to follow. Therefore, we discuss the results of the each chief guideline in the following sections.
Antidipsotropics
The prognosis 2 years after discharge was significantly better for patients who were taking antidipsotropics before discharge. We believe that readiness is an important factor in the treatment of alcohol dependence, and the decision to take antidipsotropics depends on the patient’s level of motivation. Similarly, the use of antidipsotropics is likely to have important effects in combination with psychotherapy on motivational enhancement. This study showed that participants who were taking antidipsotropics at the time of discharge had a significantly better prognosis 2 years after discharge. Therefore, an important factor for sobriety might be the decision to take antidipsotropics. We believe that antidipsotropics are psychologically needed to maintain abstinence without reduction of craving by the action of the medication. During the research period (2007–2008), we could not use acamprosate in Japan, and we had been able to use it from 2013. From now on, we should reconsider about the combination with acamprosate.
That period may vary depending on the individual, and in our hospital, we often prescribe antidipsotropics for 2–3 years. Findings from our study, including the absence of severe side effects even after 2 years of antidipsotropic administration, indicate that usage for a longer term than the period recommended in the questionnaire study12 is reasonable. Therefore, we feel that a larger study about the usefulness of antidipsotropics is needed.
On the other hand, the COMBINE study29 demonstrated that placebo was also effective in the treatment of alcohol dependence, and the importance of pill taking was pointed out. Therefore, we might be able to say the same thing for antidipsotropics in this research, because we have no control group.
Self-help groups
Regular meetings of Dansyukai are held in 16 places in Mie, Japan, whereas AA meetings are held in only two places. Because none of the participants in this study attended AA meetings, we were not able to compare the two types of self-help programs. However, no previous evidence indicates a difference in efficacy between Dansyukai and AA, and it seems that attendance in either program would fulfill the self-help group requirement of 3CGS. From the results of this study, participants who made the decision to participate in self-help groups before discharge from residential treatment had a significantly better prognosis 2 years after discharge than those who did not make this decision, especially if they were also taking antidipsotropics. In addition, an earlier study3 reported that enrollment in Dansyukai had a meaningful influence on convalescence. Therefore, we believe that the prognosis improved more by continuous participation in regular meetings of self-help groups. However in the handbook of alcoholism treatment approaches,30 participation in self-help groups and taking antidipsotropics are a statistically negative evaluation. Further study is needed on this subject.
Regular medical checkups
Attending regular medical checkups has been shown to be the most important factor in convalescence from alcohol dependence.4,8 The results of our study support the importance of regular medical checkups. Furthermore, we would like to focus on the fact that the frequency of medical checkups attended was higher in this study, as compared to previous studies.7,9,14 It is a well-known fact that alcoholics may recover even if they drink during treatment or are rehospitalized, as long as they are connected to a medical support system. Finally, the patients who had been regularly attending medical checkups were rehospitalized significantly more number of times. We did not get any finding about readmission. However, we believe that regular medical checkups enhance the motivation to decide their voluntary admissions.
Natural recovery
Although for many sufferers, substance dependence is a chronic relapsing disorder similar to hypertension, diabetes, and asthma,1 a study in the US showed that 24.4% of alcoholics recover without hospital consultations or self-help group attendance.31 It is possible that some of the patients who dropped out of this study experienced this so-called “natural recovery”.
Limitations
We had no control group and did not randomly assign the groups. Therefore, our data had a large bias in grouping. Although we assured participants that their privacy would be protected, we cannot be certain that their self-reports about redrinking were reliable. With the permission of the participants, we attempted to confirm their reports with information from their families or medical attendants, but we cannot deny that reporting bias may have occurred. Therefore, the accuracy of redrinking was poor because we decided by self-declaration, interview by telephone, and information from informants. We also feel that participants tend to underreport their failure to attend medical checkups. However, we believe that the bias in this category may be lower than for redrinking because participants who have attended medical checkups cannot be classified as abstinent by using objective findings such as information from family members and biochemical examination by medical staff.
Participants who were taking antidipsotropics had a lower mortality rate compared to participants who were not taking antidipsotropics. In addition, participants who were taking antidipsotropics were required to attend regular medical examinations. Both of these factors may have supported the effectiveness of antidipsotropics. Furthermore, we did not check the compliance to the antidipsotropic regimen, because disulfiram may well have positive effects on drinking if medication compliance procedures are employed.15,32–34
The number of participants in this study was small, and we examined only alcoholics who were voluntarily attending inpatient treatment. Furthermore, because rehabilitation is usually attempted during hospitalization, residential treatment in Japan tends to be for a longer term than in other countries. An additional limitation of this study is the possible bias introduced by patients who refused to participate or who dropped out during the research.
Conclusion
In this study, we reported on the effectiveness of 3CGS for the first time. According to a literature review,17 a treatment period of 12 months has been classified as a long period for alcohol dependence. This study examined the recovery rate of alcoholics 2 years after discharge from residential treatment. However, due to the chronic nature of alcoholism, further studies are required to investigate the efficacy of 3CGS beyond 2 years.
Acknowledgment
This work was supported by Mental Care Center, Prefecture of Mie, and Department of Psychiatry, Nara Medical University School of Medicine.
Disclosure
The authors report no conflicts of interest in this work.
References
McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284(13):1689–1695. | ||
Enoch MA. The influence of gene-environment interactions on the development of alcoholism and drug dependence. Curr Psychiatry Rep. 2012;14(2):150–158. | ||
Suzuki Y. A multiphasic study of the prognoses of 625 alcoholics. Seishin Shinkeigaku Zasshi. 1982;84(4):243–261. (in Japanese). | ||
Suwaki H. A follow-up study of alcoholic patients. Seishin Shinkeigaku Zasshi. 1975;77(2):89–106. (in Japanese). | ||
Matsumoto T, Kobayashi O, Imamura F. Workbook of Recovery Support for Alcohol and Drug Dependence. Tokyo: Kongo Shuppan; 2011:84–89. (in Japanese). | ||
Baekeland F, Lundwall L. Dropping out of treatment: a critical review. Psychol Bull. 1975;82(5):738–783. | ||
Scivoletto S, De Andrade AG, Castel S. The effect of a “recall-system” in the treatment of alcoholic patients. Br J Addict. 1992;87(8): 1185–1188. | ||
Dale V, Coulton S, Godfrey C, et al; UKATT Research Team. Exploring treatment attendance and its relationship to outcome in a randomized controlled trial of treatment for alcohol problems: secondary analysis of the UK alcohol treatment trial (UKATT). Alcohol Alcohol. 2011;46(5):592–599. | ||
Nishikawa K, Hashimoto N, Tatsuki S, Hirano K, Imamichi H. Research on factors for dropout from treatment by outpatients of alcohol abuse or alcohol dependence (II) – based on questionnaire’s outcome. Nihon Arukoru Yakubutsu Igakkai Zasshi. 2002;37(5):496–504. (in Japanese). | ||
Kaskutas LA. Alcoholics anonymous effectiveness: faith meets science. J Addict Dis. 2009;28(2):145–157. | ||
Nishikawa K. Prognostic factors for alcoholism. Ecological Social Work for Patients and Families Alcoholism. Tokyo: Aikawasyobou; 2006:79–120. | ||
Kochi Y, Fukushima H, Suwaki H, et al. Physiopathology of alcoholism and present status of the therapy in Japan – result of the questionnaires sent to all psychiatric care facilities. Seishin Shinkeigaku Zasshi. 2007;109(6):541–546. (in Japanese). | ||
Saito T, Ozaki S. General remarks for pharmacotherapy. In: Shirakura K, Higuchi S, Wada K, editors. Guidelines of Diagnosis and Treatment for Alcohol and Drug-Related Disorders. Tokyo: Jihou; 2003:33–39. (in Japanese). | ||
Berglund M. A better widget? Three lessons for improving addiction treatment from a meta-analytical study. Addiction. 2005;100(6):742–750. | ||
Chick J, Gough K, Falkowski W, et al. Disulfiram treatment of alcoholism. Br J Psychiatry. 1992;161:84–89. | ||
Diehl A, Ulmer L, Mutschler J, et al. Why is disulfiram superior to acamprosate in the routine clinical setting? A retrospective long-term study in 353 alcohol-dependent patients. Alcohol Alcohol. 2010;45(3):271–277. | ||
Jørgensen CH, Pedersen B, Tønnesen H. The efficacy of disulfiram for the treatment of alcohol use disorder. Alcohol Clin Exp Res. 2011;35(10):1749–1758. | ||
Krampe H, Spies CD, Ehrenreich H. Supervised disulfiram in the treatment of alcohol use disorder: a commentary. Alcohol Clin Exp Res. 2011;35(10):1732–1736. | ||
Laaksonen E, Koski-Jännes A, Salaspuro M, Ahtinen H, Alho H. A randomized, multicentre, open-label, comparative trial of disulfiram, naltrexone and acamprosate in the treatment of alcohol dependence. Alcohol Alcohol. 2008;43(1):53–61. | ||
Neto D, Lambaz R, Tavares JE. Compliance with aftercare treatment, including disulfiram, and effect on outcome in alcohol-dependent patients. Alcohol Alcohol. 2007;42(6):604–609. | ||
Niederhofer H, Staffen W, Mair A. Comparison of cyanamide and placebo in the treatment of alcohol dependence of adolescents. Alcohol Alcohol. 2003;38(1):50–53. | ||
Allen JP, Litten RZ. Techniques to enhance compliance with disulfiram. Alcohol Clin Exp Res. 1992;16(6):1035–1041. | ||
World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical descriptions and diagnostic guidelines. Geneva: WHO; 1992. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. | ||
Ministry of Health, Labour and Welfare [webpage on the Internet]. Healthy Japan 21. Available from: http://www1.mhlw.go.jp/topics/kenko21_11/b5f.html. Accessed June 10, 2016. | ||
Chiba R, Kawakami N, Miyamoto Y, Andresen R. Reliability and validity of the Japanese version of the self-identified stage of recovery for people with long term mental illness. Int J Ment Health Nurs. 2010;19(3):195–202. | ||
Cho T, Tanoue Y, Ishimoto S. Research on the recovery from alcohol and drug dependence on welfare recipients, Report a comprehensive community life support services for assistance for the social life of an addiction. Ministry of Health, Labour and Welfare; Tokyo. 2009:117–128. (in Japanese). | ||
Betty Ford Institute Consensus Panel. What is recovery? A working definition from the Betty Ford Institute. J Subst Abuse Treat. 2007;33(3):221–228. | ||
Anton RF, O’Malley SS, Ciraulo DA, et al; COMBINE Study Research Group. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295(17):2003–2017. | ||
Miller WR, Wilbourne PL, Hettema JE. What works? A summary of alcohol treatment outcome research. In: Hester RK, Miller WR, editors. Handbook of Alcoholism Treatment Approaches: Effective Alternatives. 3rd ed. Boston, MA: Allyn and Bacon; 2003:13–63. | ||
Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100(3):281–292. | ||
Fuller RK, Branchey L, Brightwell DR, et al. Disulfiram treatment of alcoholism. A Veterans Administration Cooperative Study. JAMA. 1986;256(11):1449–1455. | ||
De Sousa A, De Sousa A. A one-year pragmatic trial of naltrexone vs disulfiram in the treatment of alcohol dependence. Alcohol Alcohol. 2004;39(6):528–531. | ||
De Sousa A, De Sousa A. An open randomized study comparing disulfiram and acamprosate in the treatment of alcohol dependence. Alcohol Alcohol. 2005;40(6):545–548. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.