Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
TVT versus TOT in the treatment of female stress urinary incontinence: a systematic review and meta-analysis
Authors Huang ZM, Xiao H, Ji ZG, Yan WG, Zhang YS
Received 22 March 2018
Accepted for publication 8 May 2018
Published 20 November 2018 Volume 2018:14 Pages 2293—2303
DOI https://doi.org/10.2147/TCRM.S169014
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Zhong-Ming Huang, He Xiao, Zhi-Gang Ji, Wei-Gang Yan, Yan-Sheng Zhang
Department of Urology, Peking Union Medical College Hospital, Chinese Academy of Medical Science and Peking Union Medical College, Beijing 100730, China
Background: To evaluate the evidence available on the effects and safety of tension-free vaginal tape (TVT) versus transobturator tape (TOT) for female stress urinary incontinence therapy based on randomized controlled trials (RCTs).
Methods: PubMed, Cochrane, Embase, Wanfang, China National Knowledge Infrastructure, and Weipu database were searched up to July 2017 to identify relevant studies, including qualified RCT and quite-RCT and literature sources. Relative risks (RRs), mean difference (MD), and 95% CI were calculated in our review.
Result: Twenty-eight RCTs were involved in the meta-analysis with 2,505 patients in the TVT group and 2,477 patients in the TOT group. The aggregated results indicated that TOT significantly decreased the operative time (MD, −1.27; 95% CI: −1.77 to −0.76) and hospital stay (MD, −0.62; 95% CI: −1.08 to −0.17) when compared with TVT. Besides, the complications (RR, 0.86; 95% CI: 0.64–1.16) and blood loss (MD, −0.29; 95% CI: −0.71 to 0.14) were decreased in TOT but with no statistical significance; the change of VAS score (MD, 0.07; 95% CI: −0.05 to 0.19), IIQ-7 score (MD, 0.06; 95% CI: −0.03 to 0.15), and UDI-6 score (MD, 0.15; 95% CI: −0.19 to 0.48) were larger in TOT group than in TVT group, but still, with no statistical significance. However, there was no significant difference of cure rate (RR, 1.00; 95% CI: 0.96–1.04) and satisfied rate (RR, 1.00; 95% CI: 0.96–1.04) between the 2 groups.
Conclusion: TOT may have more valid effects than TVT in operative time and hospital stay. Besides, TOT method showed fewer complications and blood loss than TVT, but there was no significant difference between them. The scores of VAS, incontinence impact questionnaire short form-7 (IIQ-7), and urogenital distress inventory short form-6 (UDI-6) were higher in TOT than TVT, but still no significant difference was observed. However, more studies with higher quality and larger sample size that are multicentric and have longer follow-up in the form of RCTs are warranted to confirm the current findings.
Keywords: TVT, TOT, SUI, meta-analysis, randomized controlled trial
Introduction
Stress urinary incontinence (SUI) is a common disease among middle and aged females, associated with obesity. It is estimated that about 10%–55% of females aged 15–64 have SUI,1 and the prevalence increases with age.2 The International Continence Society defines SUI as the complaint of involuntary urine leakage with effort, exertion, sneezing, or coughing;3 it results from hypermobility of the urethra and functional insufficiency of the urethral sphincter. Ten percent of middle-aged women reported daily or severe incontinence and at least one-third reported leakage at least weekly.4 The main pathogenic factors of SUI include age, menopause, hormone level, body mass index (BMI) and so on, and it is closely related to the number of pregnancies/childbirth, pelvic organ prolapse, chronic pelvic pain, history of pelvic surgery, diet, and lifestyle.5
Nonsurgical therapy and surgical therapy have been used for the treatment of SUI. The surgical therapy is mainly used in patients with ineffective nonsurgical therapy, moderate or severe SUI, bad living quality, and basin function lesion with pelvic organ prolapse.6 The surgeries are of various types such as traditional open operation, minimally invasive surgery, tension-free vaginal tape (TVT), transobturator tape (TOT), and so on. The current gold standard for treating SUI is sling surgery. Many studies were conducted to identify the efficacy of these surgeries; however, no effective conclusions were drawn about the efficacy of TVT vs TOT in the treatment of SUI. We, therefore, conducted this meta-analysis of eligible randomized controlled trials (RCTs) to assess the effects and safety of TVT compared with TOT in the treatment of SUI.
Methods
Search strategy
The electronic databases of The Cochrane Library, PubMed, Embase, China National Knowledge Infrastructure, WangFang, and Weipu were systematically searched to identify relevant studies including all RCTs about the efficacy of TVT versus TOT in the treatment of bladder cancer up to July 2017. The databases were searched independently by 2 investigators, and a third investigator was involved to reach an agreement.
Study selection
The studies that met the following criteria were included in our review: 1) RCT or quite-RCT (quite-RCT means the groupings are dependent on birth date, admission number, or the time of admission. It is a “randomized design” but does not state the randomization method); 2) the research subjects are females with SUI and with no other serious diseases; 3) TVT group and TOT group were involved with relevant interventions for the studies; and 4) the publications were available in English or Chinese.
The studies that met the following criteria were extracted: 1) repeated publications, or shared content and results; 2) faulty data; 3) case report, theoretical research, conference report, systematic review, meta-analysis, expert comment, or economic analysis; and 4) the outcomes were not relevant.
Data extraction and quality assessment
Two reviewers independently extracted data based on predefined criteria. Differences were settled by discussion with a third reviewer. The analyses data were extracted from all the included studies and consisted of 2 parts: general information and main outcomes. The authors’ names, the detailed interventions of the 2 groups, the sample size, the percentage of male, the mean age, and the relative information from the Jadad were extracted as general information. Clinical outcomes, such as total operative time, blood loss, transfusion rate, hospital stay, and complications, were utilized to analyze the studies. The Jadad scoring checklist was used to assess the quality of involved studies. We evaluated all the RCTs through following 5 domains: allocation concealment; random sequence generation; blinding of participants and personnel; double-blind assessment; and incomplete outcome data. Domains were classified as “low quality and high bias risks” and “high quality,” with a score of <3 and >3, respectively. The assessments were performed by 2 reviewers independently. Any arising differences were resolved by discussion.
Statistical analysis
All statistical analyses were performed using the STATA 10.0 software (StataCorp LLC, College Station, TX, USA). χ2 and I2 tests were used to assess the statistical heterogeneity of clinical trial results and determine the analysis model (fixed-effect model or random-effect model). The heterogeneity was acceptable when the χ2 test P-value was <0.05 and the value of I2 was >50% assessed by random-effects model. It was defined as homogeneous data when the χ2 test P-value was more than 0.05 and the value of I2 was <50% assessed by fixed-effects model. The continuous variables were expressed as the mean ± SD and analyzed by mean difference (MD). The categorical data were calculated as percentages and analyzed by relative risk (RR) or odds ratio (OR). Complications, cure rate, and satisfaction rate were analyzed by RR and 95% CI. MD and 95% CI were calculated to analyze total operative time, blood loss, hospital stay, VAS score, IIQ-7 score, and UDI-6 score.
Results
Literature search
A total of 2,643 records were identified by the searches. During the preliminary screening of the titles and abstracts, 2,551 records were eliminated, leaving 92 records for further selection. After full-text screening, 64 records were excluded due to the following criteria: not RCTs (26), noncontrolled study (19), reviews (5), had no outcomes (11), and repeat publication (3). Finally, 28 records7–30 were included in our meta-analysis with 2,505 patients in the TVT group and 2,477 patients in the TOT group. The detailed search process is presented in Figure 1.
  | Figure 1 Flow diagram of the literature search and selection process. |
Study characteristics
The main characteristics of all included studies are summarized in Table 1. The general information included treatment, number of patients, age and BMI, and the treatment of TOT from inside to outside and from outside to inside. The age and BMI in the 2 groups were similar. The mean Jadad score of the included studies was 2.24, and a main score lower than 3 indicated low the quality of the included studies.
Complications
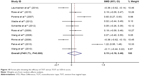
Eleven studies with 2,515 patients (TVT group =1,279, TOT group =1,236) reported on complications. Based on the χ2 test P-value (P=0.000) and I2 test value (I2=70.1%), random-effect model was chosen to analyze the complications. The pooled results showed that TOT decreased the incidence of complication compared with the TVT, but without statistical significance (RR, 0.86; 95% CI: 0.64–1.16, Figure 2).
Cure rate
Ten studies with 1,991 patients (TVT group =982, TOT group =1,009) reported on cure rate. Based on the χ2 test P-value (P=0.943) and I2 test value (I2=0.0%), fixed-effect model was chosen to analyze the cure rate. There was no significant difference of cure rate between the 2 groups (RR, 1.00; 95% CI: 0.96–1.04, Figure 3).
  | Figure 3 Forest plot showing the efficacy of TVT versus TOT on cure rate. |
Satisfaction rate
Six studies with 1,128 patients (TVT group =569, TOT group =559) reported on satisfaction rate. Based on the χ2 test P-value (P=0.790) and I2 test value (I2=0.0%), fixed-effect model was chosen to analyze the satisfaction rate. There was no significant difference of satisfaction rate between the two groups (RR, 1.00; 95% CI: 0.96–1.04, Figure 4).
  | Figure 4 Forest plot showing the efficacy of TVT versus TOT on satisfaction rate. |
Operative time
Eleven studies with 2,861 patients (TVT group =1,440, TOT group =1,421) reported on operative time. Based on the χ2 test P-value (P=0.000) and I2 test value (I2=97.3%), random-effect model was chosen to analyze the operative time. TOT significantly decreased the operative time compared with TVT (MD, −1.27; 95% CI: −1.77 to −0.76, Figure 5).
Blood loss
Ten studies with 1,784 patients (TVT group =893, TOT group =891) reported on blood loss. Based on the χ2 test P-value (P=0.000) and I2 test value (I2=94.7%), random-effect model was chosen to analyze the blood loss. TOT reduced the blood loss, but with no statistical significance compared with TVT (MD, −0.29; 95% CI: −0.71 to 0.14, Figure 6).
Hospital stay
Thirteen studies with 1,892 patients (TVT group =958, TOT group =934) reported on hospital stay. Based on the χ2 test P-value (P=0.000) and I2 test value (I2=95.5%), random-effect model was chosen to analyze the hospital stay. The hospital stay was significantly decreased in the TOT group compared with TVT group (MD, −0.62; 95% CI: −1.08 to −0.17, Figure 7).
VAS score
Five studies with 1,151 patients (TVT group =581, TOT group =570) reported on scores obtained on the VAS. Based on the χ2 test P-value (P=0.000) and I2 test value (I2=92.1%), random-effect model was chosen to analyze the VAS score. The change in VAS score after the treatment was larger in TOT group than in TVT group, but without statistical significance (MD, 0.07; 95% CI: −0.05 to 0.19, Figure 8).
  | Figure 8 Forest plot showing the efficacy of TVT versus TOT on VAS score. |
IIQ-7 score
Eleven studies with 1,943 patients (TVT group =988, TOT group =955) reported on IIQ-7 score. Based on the χ2 test P-value (P=0.100) and I2 test value (I2=37.5%), fixed-effect model was chosen to analyze the IIQ-7 score. The decrease in IIQ-7 score was more in TOT group than in TVT group, but without statistical significance (MD, 0.06; 95% CI: −0.03 to 0.15, Figure 9).
  | Figure 9 Forest plot showing the efficacy of TVT versus TOT on IIQ-7 score. |
UDI-6 score
Eleven studies with 1,779 patients (TVT group =907, TOT group =872) reported on UDI-6 score. Based on the χ2 test P-value (P=0.000) and I2 test value (I2=91.7%), random-effect model was chosen to analyze the UDI-6 score. The change in UDI-6 score after the treatment was larger in TOT group than in TVT group, but without statistical significance (MD, 0.15; 95% CI: −0.19 to 0.48, Figure 10).
Quality assessment and potential bias
Based on the mentioned criteria, 28 articles were included in the meta-analysis. The quality assessment and potential bias were assessed by funnel plot, Begg and Mazumdar’s rank test, and Egger’s test. The funnel plot for MD with regard to operative time in the included studies was notably unsymmetrical, suggesting significant publication bias (Figure 11). Moreover, significant asymmetry was detected using Begg and Mazumdar’s rank test (Z=2.24, P=0.025). The Egger’s test result showed that there was significant publication bias (P=0.033).
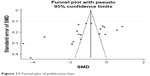  | Figure 11 Funnel plot of publication bias. |
Discussion
Petros and Ulmsten31 were the first to come up with the treatment TVT in 1995. TOT was proposed by some scholars in 2001, and another TVT inside-out (TVT-obturator system) was proposed by de Leval4 In previous studies, Maggiore et al32 reported that objective and subjective cumulative cure rates of TVT and TOT (both out–in and in–out) were 61.6% (95% CI: 58.5%–64.8%) and 76.5% (95% CI: 73.8%–79.2%), and 64.4% (95% CI: 61.4%–67.4%) and 81.3% (95% CI: 78.9%–83.7%), respectively. Both TVT and TOT were associated with similar long-term objectives (OR, 0.87 [95% CI: 0.49–1.53]) and subjective (OR, 0.84 [95% CI: 0.46–1.55]) cure rates. In addition, it was shown that there was no significant difference in the complication rates when TVT was compared with TOT: TVT versus TOT (OR, 0.83 [95% CI: 0.54–1.28]), TOT-O versus TVT-O (OR, 0.77 [95% CI: 0.17–3.46]). Huang et al33 found that TVT-Secur showed significant reduction in operative time, visual analog score for pain, and postoperative complications compared with TVT-O. TVT-Secur had a significantly lower subjective cure rate (P<0.00001), lower objective cure rate (P<0.00001), and higher intraoperative complication rate compared with TVT-O at 1–3 years; however, there was no significant difference between TVT-Secur and TVT-O in the subjective cure rate, objective cure rate, or complications at 3–5 years. Moreover, TVT-Secur had significantly lower subjective and objective cure rates compared with TVT.
The operative time in our systematic review and meta-analysis was significantly decreased in TOT group when compared with TVT group; TOT had shorter operative time with no routine cystoscopy. TOT would reduce the incidence of bladder perforation, which helps patients return to normal life as soon as possible, so the hospital stay was significantly shorter in TOT group.
The complications can be either intraoperative or postoperative. The intraoperative complications include necessity of blood transfusion, bladder injury, vaginal wall perforation, urethral injury, ureteral injury, bowel injury, cardiac arrhythmia, and so on. The postoperative complications are infections requiring antibiotics, urinary tract infections, cardiac or myocardial infarction, pulmonary, ileus, pelvic abscess, necessity for blood transfusion, leg or obturator complication, hospital readmissions, emergency room evaluations, and so on. The incidence of bladder perforation or vaginal perforation was reported to be as high as 24%;34 thus, TOT (in–out and out–in) appeared successively. In this review, we found that the complications were lower in TOT group than in TVT group, and the blood loss was also decreased in TOT group, but this showed no statistical significance. More studies are required to support the evidence.
The UDI-6 questionnaire is used to evaluate the urethral stimulant symptom, pressure symptoms, and obstructive symptoms in SUI patients. The IIQ-7 questionnaires evaluate four aspects including daily activities, physical activities, social activities, and psychological health of patients. The VAS is used to assess the pain in patients. The change in VAS score (MD, 0.07; 95% CI: −0.05 to 0.19), IIQ-7 score (MD, 0.06; 95% CI: −0.03 to 0.15), and UDI-6 score (MD, 0.15; 95% CI: −0.19 to 0.48) before and after the operation were larger in TOT group than in TVT group, but without statistical significance.
The cure rate in this review was same as the objective cure rate, and satisfaction rate was same as the subjective cure rates. We found that there was no significant difference in cure rate and satisfaction rate between the 2 groups, and the results were consistent with that of Leval et al.
However, there were several limitations in this analysis, such as the following: 1) only RCTs and quite-RCT were included; 2) there were differences in the inclusion and exclusion criteria for patients; 3) different patients with previous disease and treatments were unavailable; 4) some trials with low quality and low Jadad score were included in our study; 5) all the included studies were in English and/or Chinese only; 6) the technique of surgery between different studies was different; and 7) pooled data were used for analysis, and individual patient data was unavailable. Considering all the limitations mentioned above, more high-quality studies are needed to confirm our current findings.
Conclusion
Our systematic review and meta-analysis suggested that TOT is better at decreasing operative time, the length of hospital stay, the incidence of complications, the blood loss, and leading to score reductions in VAS, IIQ-7, and UDI-6 compared with TVT, indicating TOT to be a more effective and safer method in the treatment of SUI. More detailed research with well-performed assays and larger sample size are warranted to verify these results.
Disclosure
The authors report no conflicts of interest in this work.
References
Liedl B. Urinary stress incontinence in women. Aktuelle Urol. 2004;35(6):485–490. | ||
Luber KM. The definition, prevalence, and risk factors for stress urinary incontinence. Rev Urol. 2004;6(Suppl 3):S3–S9. | ||
Abrams P, Blaivas JG, Stanton S, Andersen JT. The standardisation of terminology of lower urinary tract function. The International Continence Society Committee on Standardisation of Terminology. Scand J Urol Nephrol Suppl. 1998;114. | ||
de Leval J. Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol. 2003;44(6):724–730. | ||
Hunskaar S, Burgio K, Clark A, et al. Epidemiology of urinary (UI) and faecal (FI) incontinence and pelvic organ prolapse (POP). WHO-ICS International Consultation on Incontinence. 3rd ed. Paris: Health Publications Ltd; 2005. | ||
Na Yanqun SG. China Urology Disease Diagnosis and Treatment Guidelines. Beijing: People’s Medical Publishing House. 2009;151. | ||
Teo R, Moran P, Mayne C, Tincello D. Randomized trial of tension-free vaginal tapeand tension-free vaginal tape-obturator for urodynamic stress incontinence in women. J Urol. 2011;185(4):1350–1355. | ||
Wang W, Zhu L, Lang J. Transobturator tape procedure versus tension-free vaginal tape for treatment of stress urinary incontinence. Int J Gynaecol Obstet. 2009;104(2):113–116. | ||
Rinne K, Laurikainen E, Kivelä A, et al. A randomized trial comparing TVT with TVT-O: 12-month results. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(8):1049–1054. | ||
Zyczkowski M, Nowakowski K, Kuczmik W, et al. Tension-free vaginal tape, transobturator tape, and own modification of transobturator tape in the treatment of female stress urinary incontinence: comparative analysis. Biomed Res Int. 2014;2014:1–6. | ||
Zullo MA, Plotti F, Calcagno M, et al. One-year follow-up of tension-free vaginal tape (TVT) and trans-obturator suburethral tape from inside to outside (TVT-O) for surgical treatment of female stress urinary incontinence: a prospective randomised trial. Eur Urol. 2007;51(5):1376–1384. | ||
Zhang Y, Jiang M, Tong XW, Fan BZ, Li HF, Chen XL. The comparison of an inexpensive-modified transobturator vaginal tape versus TVT-O procedure for the surgical treatment of female stress urinary incontinence. Taiwan J Obstet Gynecol. 2011;50(3):318–321. | ||
Wang YJ, Li FP, Wang Q, Yang S, Cai XG, Chen YH. Comparison of three mid-urethral tension-free tapes (TVT, TVT-O, and TVT-Secur) in the treatment of female stress urinary incontinence: 1-year follow-up. Int Urogynecol J. 2011;22(11):1369–1374. | ||
Wang F, Song Y, Huang H. Prospective randomized trial of TVT and TOT as primary treatment for female stress urinary incontinence with or without pelvic organ prolapse in Southeast China. Arch Gynecol Obstet. 2009;281(2):279–286. | ||
Wadie BS, El-Hefnawy AS. TVT versus TOT, 2-year prospective randomized study. World J Urol. 2013;31(3):645–649. | ||
Schierlitz L, Dwyer PL, Rosamilia A, et al. Three-year follow-up of tension-free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency. Obstet Gynecol. 2012;119(2 Pt 1):321–327. | ||
Ross S, Tang S, Eliasziw M, et al. Transobturator tape versus retropubic tension-free vaginal tape for stress urinary incontinence: 5-year safety and effectiveness outcomes following a randomised trial. Int Urogynecol J. 2015;27(6):879–886. | ||
Ross S, Robert M, Swaby C, et al. Transobturator tape compared with tension-free vaginal tape for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2009;114(6):1287–1294. | ||
Porena M, Costantini E, Frea B, et al. Tension-free vaginal tape versus transobturator tape as surgery for stress urinary incontinence: results of a multicentre randomised trial. Eur Urol. 2007;52(5):1481–1491. | ||
Palva K, Rinne K, Aukee P, et al. A randomized trial comparing tension-free vaginal tape with tension-free vaginal tape-obturator: 36-month results. Int Urogynecol J. 2010;21(9):1049–1055. | ||
Laurikainen E, Valpas A, Aukee P, et al. Five-year results of a randomized trial comparing retropubic and transobturator midurethral slings for stress incontinence. Eur Urol. 2014;65(6):1109–1114. | ||
Krofta L, Feyereisl J, Otčenášek M, Velebil P, Kašíková E, Krčmář M. TVT and TVT-O for surgical treatment of primary stress urinary incontinence: prospective randomized trial. Int Urogynecol J. 2009;21(2):141–148. | ||
Kenton K, Stoddard AM, Zyczynski H, et al. 5-year longitudinal followup after retropubic and transobturator mid urethral slings. J Urol. 2015;193(1):203–210. | ||
Karateke A, Haliloglu B, Cam C, Sakalli M. Comparison of TVT and TVT-O in patients with stress urinary incontinence: short-term cure rates and factors influencing the outcome. A prospective randomised study. Aust N Z J Obstet Gynaecol. 2009;49(1):99–105. | ||
Freeman R, Holmes D, Hillard T, et al. What patients think: patient-reported outcomes of retropubic versus trans-obturator mid-urethral slings for urodynamic stress incontinence – a multi-centre randomised controlled trial. Int Urogynecol J. 2011;22(3):279–286. | ||
Deffieux X, Daher N, Mansoor A, Debodinance P, Muhlstein J, Fernandez H. Transobturator TVT-O versus retropubic TVT: results of a multicenter randomized controlled trial at 24 months follow-up. Int Urogynecol J. 2010;21(11):1337–1345. | ||
de Tayrac R, Deffieux X, Droupy S, Chauveaud-Lambling A, Calvanèse-Benamour L, Fernandez H. Retracted: a prospective randomized trial comparing tension-free vaginal tape and transobturator suburethral tape for surgical treatment of stress urinary incontinence. Am J Obstet Gynecol. 2004;190(3):602–608. | ||
Araco F, Gravante G, Sorge R, et al. TVT-O vs TVT: a randomized trial in patients with different degrees of urinary stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(7):917–926. | ||
Angioli R, Plotti F, Muzii L, Montera R, Panici PB, Zullo MA. Tension-free vaginal tape versus transobturator suburethral tape: five-year follow-up results of a prospective, randomised trial. Eur Urol. 2010;58(5):671–677. | ||
Ito H, Yamanaka H, Hagiwara M, Furuuchi T, Matsumoto K, Kanai K, et al. Efficacy of tension-free vaginal tape compared with transobturator tape in the treatment of stress urinary incontinence in women: analysis of learning curve, perioperative changes of voiding function. BMC Urology. 2011;11:13. | ||
Petros PE, Ulmsten UI. An integral theory and its method for the diagnosis and management of female urinary incontinence. Scand J Urol Nephrol Suppl. 1993;153:1–93. | ||
Leone Roberti Maggiore U, Finazzi Agro E, Soligo M, Li Marzi V, Digesu A, Serati M. Long-term outcomes of TOT and TVT procedures for the treatment of female stress urinary incontinence: a systematic review and meta-analysis. Int Urogynecol J. 2017;28(8):1119–1130. | ||
Huang W, Wang T, Zong H, Zhang Y. Efficacy and safety of tension-free vaginal tape-secur mini-sling versus standard midurethral slings for female stress urinary incontinence: a systematic review and meta-analysis. Int Neurourol J. 2015;19(4):246–258. | ||
Liapis A, Bakas P, Creatsas G. Monarc vs TVT-O for the treatment of primary stress incontinence: a randomized study. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(2):185–190. | ||
Wadie BS, El-Hefnawy AS. TVT versus TOT, 2-year prospective randomized study. World J Urol. 2013;31(3):645–649. | ||
Oliveira R, Botelho F, Silva P, et al. Exploratory study assessing efficacy and complications of TVT-O, TVT-Secur, and Mini-Arc: results at 12-month follow-up. Eur Urol. 2011;59(6):940–944. | ||
Araco F, Gravante G, Sorge R, et al. TVT-O vs TVT: a randomized trial in patients with different degrees of urinary stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(7):917–926. | ||
Wang WY, Zhu L, Lang JH, Sun ZJ, Hai N. Línchuáng yánjiū yīndào wú zhānglì niàodào xuán diào zhìliáo yánzhòng yālì xìng niào shījìn de bùtóng tújìng [Clinical study on tension-free vaginal tape and tension-free vaginal tape obturator for surgical treatment of severe stress urinary incontinence]. Chin J Obstet Gynecol. 2008;43(3):180–184. Chinese. | ||
Porena M, Costantini E, Frea B, Giannantoni A, Ranzoni S, Mearini L, et al. Tension-free vaginal tape versus transobturator tape as surgery for stress urinary incontinence: results of a multicentre randomised trial. Eur Urol. 2007;52(5):1481–1490. | ||
Zullo MA, Plotti F, Calcagno M, Marullo E, Palaia I, Bellati F, et al. One-Year Follow-up of Tension-free Vaginal Tape (TVT) and Trans-obturator Suburethral Tape from Inside to Outside (TVT-O) for Surgical Treatment of Female Stress Urinary Incontinence: A Prospective Randomised Trial. Eur Urol. 2007;51(5):1376–1384. | ||
Wang F, Song Y, Huang H. Prospective randomized trial of TVT and TOT as primary treatment for female stress urinary incontinence with or without pelvic organ prolapse in Southeast China. Arch Gynecol Obstet. 2009;281(2):279–286. | ||
Barber MD, Kleeman S, Karram MM, Paraiso MF, Walters MD, Vasavada S, et al. Transobturator tape compared with tension-free vaginal tape for the treatment of stress urinary incontinence: a randomized controlled trial. Obstet Gynecol. 2008;111(3):611–621. | ||
Wang YJ, Li FP, Wang Q, Yang S, Cai XG, Chen YH. Comparison of three mid-urethral tension-free tapes (TVT, TVT-O, and TVT-Secur) in the treatment of female stress urinary incontinence: 1-year follow-up. Int Urogynecol J. 2011;22(11):1369–1374. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.