Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 14
Tumor of the Nose – A Rare Manifestation of a Metastatic Lung Cancer
Authors Bolewska A , Słowińska M, Błońska A, Ceryn J, Grala B, Narbutt J, Ciążyńska M, Małecki W, Skibińska M, Lesiak A, Paluchowska E, Owczarek W
Received 27 May 2021
Accepted for publication 5 August 2021
Published 21 September 2021 Volume 2021:14 Pages 1311—1318
DOI https://doi.org/10.2147/CCID.S318748
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Aleksandra Bolewska,1 Monika Słowińska,1 Agata Błońska,1 Justyna Ceryn,2 Bartłomiej Grala,3 Joanna Narbutt,2 Magdalena Ciążyńska,4 Wojciech Małecki,5 Małgorzata Skibińska,2 Aleksandra Lesiak,2 Elwira Paluchowska,1 Witold Owczarek1
1Department of Dermatology, Military Institute of Medicine, Warsaw, Poland; 2Department of Dermatology, Pediatric Dermatology and Oncology, Medical University of Lodz, Łódź, Poland; 3Department of Pathology, Military Institute of Medicine, Warsaw, Poland; 4Department of Proliferative Diseases, Nicolaus Copernicus Multidisciplinary Centre for Oncology and Traumatology, Łódź, Poland; 5Department of Clinical Oncology and Chemotherapy, Poddębice Health Centre, Poddębice, Poland
Correspondence: Aleksandra Bolewska Tel +48 261 816 241
; +48 604 783 340
Email [email protected]
Abstract: Lung cancer most often metastasizes to the central nervous system, bone and liver. Although metastases to the skin are quite rare, it is estimated that they may be the first clinical manifestation of this disease in 0.7%– 12% of cases. Metastases to the skin are caused by adenocarcinoma (about 30%), squamous cell carcinoma (30%) and undifferentiated carcinoma (40%). Nasal tip metastases are extremely rare. They can be confused with more common skin problems, including non-melanoma skin cancers, rhinophyma, inflammatory tumors or infectious diseases. We report two patients with a tumor on the nose, which proved to be the first sign of the metastatic lung cancer.
Keywords: lung cancer, skin metastasis, ulceration, tumor
Introduction
Skin metastases from internal organ cancers are usually an incidental finding. They often present as the first symptom of a systemic disease. Metastases to the skin of the nose from lung cancer are extremely rare.1,2 Frequently they appear as fixed or mobile painless nodules. Cutaneous metastasis on the nasal tip is known as “clown nose”.12,13 It is important to distinguish suspected lesions from common non-melanoma skin cancers and less frequent tumors such as amelanotic melanoma, primary cutaneous lymphomas, and inflammatory lesions.1 We report two patients with a tumor on the nose, which proved to be the first sign of the metastatic lung cancer.
Case Reports
The first patient was a 79-year-old man admitted to the Dermatology Department with a nodular lesion located on the tip of the nose which appeared 2 months before. Initially, the lesion presented as an erythematous papule which increased rapidly in size and transformed into a nodule with an ulceration on the surface. The patient was treated with systemic antibiotics without any improvement. He had numerous comorbidities such as severe chronic obstructive pulmonary disease, chronic kidney disease, type 2 diabetes, previous myocardial infarction and was a smoker (80 pack-years).
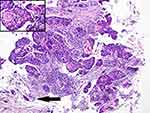
On examination there was a palpable, exophytic, erythematous lesion with a large telangiectasia and central ulceration located on the tip of the nose (Figure 1). The diameter of the lesion was 5cm. Differential diagnoses included pyoderma gangrenosum, keratoacanthoma, skin cancer and granulomatosis with vasculitis. There were no abnormalities in the nasal and nasopharyngeal fiberoscopy, the ulcer swab was sterile, antinuclear antibodies (ANA) and antineutrophil cytoplasmic antibodies against proteinase 3 (PR3) and myeloperoxidase (MPO) were negative. The biopsy of the lesion was performed, and the histopathological findings revealed features of partially keratinizing squamous cell carcinoma (SCC) (Figure 2A and B). Thoracic HRCT (High-Resolution Computed Tomography) revealed an infiltrative lesion of the upper part of the left lung cavity with dimensions 54 × 38mm adjacent to the pulmonary artery trunk, entangling the aorto-pulmonary window with bronchial infiltration into segments 1–3 and the upper left pulmonary vein as well as enlarged lymph nodes (Figure 3). The bronchoscopy revealed an infiltration spreading along the apicoposterior segment of the left upper lobe (LB1 + 2) bronchial wall. The histopathological examination of the biopsy taken from this lesion revealed partially keratinizing squamous cell carcinoma, CK5/6 (+), p63 (+) (Figure 4), which in combination with the result of histopathological examination from the skin lesion confirmed the diagnosis of disseminated squamous cell lung cancer. To exclude other metastases, diagnostic imaging was performed, and no other abnormalities were found. Due to the size of the lesion, general condition and numerous comorbidities, the patient was disqualified from surgery and chemotherapy with only palliative treatment implemented.
 |
Figure 1 Exophytic erythematous lesion on the tip of the nose with telangiectasia and central ulceration. |
The second patient was an 82-year-old woman admitted to the Dermatology Department with an ulceration located on the tip of the nose and spreading to the upper lip, covered with serous crust. The patient was treated for 12 months with topical and systemic antibiotics, antifungal, and antiviral medications with no improvement. She had a history of hypertension, rheumatoid arthritis (treated with 10 mg of methotrexate weekly and 5 mg of prednisone daily for many years), pertrochanteric fracture of the right femur in 2013, and herpes zoster of the neck in 2011. On admission her general condition was good. On examination, there was an ulceration covered with serous crust involving the tip of the nose with a visible destruction of the right ala of the nose spreading to the upper lip (Figure 5). Moreover, she had an enlarged, palpable right supraclavicular lymph node. The examination of other organs and systems was unremarkable. Routine laboratory tests showed only mild microcytic anemia, an elevated level of ESR (erythrocyte sedimentation rate) - 68mm/h, and an elevated level of beta-2-microglobulin (4.37 g/dl with normal range from 0.18 to 0.50 g/dl). Cancer markers (CEA, AFP, Ca 125, Ca 19-9, Ca 15-3), ANA, PR3, MPO antibodies, and direct immunofluorescence (DIF) test and indirect immunofluorescence (IIF) test were negative. The biopsy of the lesion was performed, and histopathological examination revealed a subepidermal concentration of atypical cells with hyperchromatic nuclei suggesting SCC surrounded by subepidermal necrotic cells (Figure 6). Extensive diagnostic imaging was performed to exclude the diagnosis of metastasis. HRCT revealed eight neoplastic infiltrations in both lungs with the biggest one present in the middle field of the left lung with dimensions 17.7 × 26.0 mm (Figure 7) and enlarged lymph node in the hilum of the left lung. Other abnormalities involved two hyperdense lesions in the right lobe of the liver with dimensions 13 × 21mm, multiple enlarged lymph nodes along the abdominal aorta forming packages, and numerous enlarged cervical lymph nodes, the biggest in the right supraclavicular fossa. Due to the result of the histopathological examination of the skin lesion and imaging studies a diagnosis of disseminated squamous cell carcinoma of the lung with metastases to the skin and the liver was made. The patient was referred to the Oncology Department and as her general condition was good (WHO-1 scale), she qualified for chemotherapy with cisplatin and vinorelbine. She started her first treatment (out of three in 21-day cycles) with 60mg/m2 intravenous cisplatin (day 1) and 20mg/m2 vinorelbine (day 1 and 8). The doses of the cytostatic medications were reduced due to the iatrogenic thrombocytopenia of 3 10^3 µL [250 — 550 10^3 µL] platelets caused most likely by the previous treatment of rheumatoid arthritis with methotrexate. After 3 weeks, she was admitted for the second cycle of treatment, but her general condition deteriorated (WHO-3 scale). Physical examination revealed asymmetric muscle weakness in the upper and lower extremities while the central nervous system (CNS) imaging revealing ischemic lesions. She was transferred to the internal medicine ward with recommendations to continue chemotherapy with oral vinorelbine if her general condition improved. No further information of the effects of her treatment was available.
 |
Figure 5 The ulceration covered with serous crust including the tip of the nose with the destruction of the right ala of the nose spreading to the upper lip. |
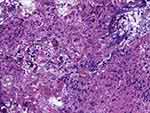 |
Figure 6 Subepidermal accumulation of atypical cells with hyperchromatic nuclei suggesting squamous cell carcinoma (SCC) (arrows) surrounded by subepidermal necrotic cells. |
 |
Figure 7 HRCT revealed eight neoplastic infiltrations in both lungs with the biggest one present in the middle field of the left lung with dimensions 17.7×26.0 mm. |
Discussion
The lung cancer most often metastasizes to the central nervous system, bone and liver. Although metastases to the skin are quite rare, it is estimated that they may be the first clinical manifestation of this disease in 0.7% −12% of cases.1–5 There are two types of lung cancer: small cell and non-small cell, which includes adenocarcinoma, SCC and large cell carcinoma. Brownstein et al described 117 cases of lung cancers with skin metastases, of which almost 30% were adenocarcinomas, 30% SCC and 40% undifferentiated carcinomas.5 According to Hidaka et al, metastasis to the skin was most often caused by adenocarcinoma and least often by large cell carcinoma.6 Terashima and Kanazawa showed that in a group of 34 patients with lung cancer, the risk of cutaneous metastases was higher in non-small cell carcinoma, of which the lowest in SCC.2 Song et al presented an analysis of 60 cases of advanced non-small cell lung cancer metastases to the skin, of which 58% were adenocarcinoma and 18% SCC.3 Cutaneous metastases of lung cancer usually arise relatively near the primary lesion - within the chest, abdomen, back, head and neck, while less often they are located on the limbs.6–8 The head area is considered the most frequent location for lung cancer metastases - about 54% of all skin metastases.6 However, in the Song et al study, the most common skin metastasis site was chest (32%) followed by head (25%) and abdomen (15%).3 Cutaneous metastases of the lung cancer are characterized by a single or multiple flesh-coloured, pink-red or purple-violet papules or nodules, most often rounded at the edges and varying in size. Over time, erosions, ulcers and numerous telangiectasias develop within the lesion. The lesions are usually painless but at an advanced stage they may cause severe pain most likely because of infiltration of the dermis and subcutaneous tissue.9,10 Nasal tip metastases are extremely rare. They can be confused with more common diseases, including non-melanoma skin cancers, rhinophyma, inflammatory tumors or infectious diseases.11 Nodular red or brown lesion located on the tip of the nose is known as a “clown nose” because of its resemblance to a red, fake nose. In addition to lung cancer, it has also been reported in hepatocellular carcinoma, esophageal cancer, seminoma, chordoma, leukemia, breast cancer, and cervical cancer.12,13 The mechanism of development of lung cancer metastases to the nasal skin is not fully understood. It is suggested that lung cancer cells can be transported through the pulmonary vessels and the lymphatic system to distant locations. Lung cancer metastases also tend to occur in acral parts of the body including the fingers and toes.11,14 Pathomorphological diagnosis of SCC of the lung metastases to the skin is difficult, mainly due to the rare occurrence of metastasis compared to cases of primary SCC of the skin, and the lack of expression of organ-specific immunohistochemical markers by tumor cells. Regardless of location of the primary lesion, it will express the same squamous cell differentiation antigens, eg p63 or CK5/6.11,15 Squamous cell carcinoma can present different degree of maturity and numerous morphological variants. A thorough analysis of clinical data and histopathological features of the tumor, sometimes combined with molecular genetics, often allows to determine whether it is SCC metastasis to the skin or a primary tumor. In the presented cases, simultaneous occurrences of SCC of the lung and skin were found. In the first patient, histopathological examination of biopsies taken from both tumors revealed identical features of medium-differentiated, partially keratinizing (G2), squamous cell carcinoma. The tumor in both locations showed stromal infiltration with irregular nests of atypical cells and features of angioinvasion (Figures 2 and 4). In the section from the skin tumor, the infiltrate of the cancer spread subcutaneously. The epidermis lying above the neoplastic tissue did not show dysplasia features. Those morphological features indicated the metastatic nature of the nasal tumor.
Due to the advancement of the neoplastic process, the prognosis for patients with lung cancer metastases to the skin is very unfavorable.1 The predicted survival varies between 3 and 6 months from the diagnosis. According to the analysis of Hidaka et al, the median survival time for patients with lung cancer from the detection of the skin metastases was only 4 months,6 with similar data of 4.9 months reported by Terashima i Kanazawa.2 Song et al observed a significant difference in overall survival time between patients with cutaneous and non-cutaneous metastases, with respectively 3.9 months vs 10 months. Interestingly, the prognosis of the disease in patients with skin metastases only compared to patients with metastases to the skin and other organs was similar, with 4 months vs 3 months, respectively.3
Conclusion
Metastases to the skin of the lung cancer are quite rare, with first clinical manifestation of the disease in 0.7−12% of patients. However, they may be the first symptom that prompts the patient to visit the doctor. Histopathological examination of the skin biopsy, which is a widely available diagnostic tool in dermatology, is necessary to obtain the diagnosis of refractory skin lesions. In case of the presence of neoplastic cells it is essential to perform imaging tests to find the primary location and the stage of the cancer. Those patients need to be promptly referred to oncology. To sum up, rare as it is, diagnosis of metastasis should be considered in each case of refractory skin lesions, especially those of morphology of tumor or ulceration.
Informed Consent Statement
The patients or their representatives had given written informed consent for the publication of the case details and all accompanying images.
Funding
This research was funded by statutory activities of Medical University of Lodz no. 503/5-064-04/503-01.
Disclosure
The authors declare no conflicts of interest.
References
1. Dhambri S, Zendah I, Ayadi-Kaddour A, Adouni O, El Mezni F. Cutaneous metastasis of lung carcinoma: a retrospective study of 12 cases. J Eur Acad Dermatol Venereol. 2011;25(6):722–726. doi:10.1111/j.1468-3083.2010.03818.x
2. Terashima T, Kanazawa M. Lung cancer with skin metastasis. Chest. 1994Nov;106(5):1448–50. doi:10.1378/chest.106.5.1448.
3. Song Z, Lin B, Shao L, Zhang Y. Cutaneous metastasis as a initial presentation in advanced non-small cell lung cancer and its poor survival prognosis. J Cancer Res Clin Oncol. 2012;138(10):1613–1617. doi:10.1007/s00432-012-1239-6
4. Brownstein MH, Helwig EB. Patterns of cutaneous metastasis. Arch Dermatol. 1972;105(6):862–868. doi:10.1001/archderm.1972.01620090034008
5. Brownstein MH, Helwig EB. Metastatic tumors of the skin. Cancer. 1972;29(5):1298–1307. doi:10.1002/1097-0142(197205)29:5<298::aid-cncr2820290526>3.0.co;2-6
6. Hidaka T, Ishii Y, Kitamura S. Clinical features of skin metastasis from lung cancer. Intern Med. 1996;35(6):459–462. doi:10.2169/internalmedicine.35.459
7. Dreizen S, Dhingra HM, Chiuten DF, Umsawasdi T, Valdivieso M. Cutaneous and subcutaneous metastases of lung cancer. Clinical characteristics. Postgrad Med. 1986;80(8):111–116. doi:10.1080/00325481.1986.11699635
8. Coslett LM, Katlic MR. Lung cancer with skin metastasis. Chest. 1990;97(3):757–759. doi:10.1378/chest.97.3.757
9. Choate EA, Nobori A, Worswick S. Cutaneous metastasis of internal tumors. Dermatol Clin. 2019;37(4):545–554. doi:10.1016/j.det.2019.05.012
10. Wang F, Tong ZH. Cutaneous metastasis as the first symptom: an uncommon presentation of squamous cell lung cancer. Chin Med J (Engl). 2017;130(1):115–116. doi:10.4103/0366-6999.196584
11. Chun SM, Kim YC, Lee JB, et al. Nasal tip cutaneous metastases secondary to lung carcinoma: three case reports and a review of the literature. Acta Derm Venereol. 2013;93(5):569–572. doi:10.2340/00015555-1529
12. Marcoval J, Martínez-Molina L, Bonfill-Ortí M, Valentí-Medina F. “Clown nose” as first manifestation of squamous cell carcinoma of the lung. J Dermatol Case Rep. 2017;11(1):9–11. doi:10.3315/jdcr.2017.1241
13. Colletti G, Allevi F, Moneghini L, Palvarini M. Clown nose: a case of disfiguring nodular squamous cell carcinoma of the face. BMJ Case Rep. 2014;2014:bcr2013200471. doi:10.1136/bcr-2013-200471
14. Batson OV. The function of the vertebral veins and their role in the spread of metastases. Ann Surg. 1940;112(1):138–149. doi:10.1097/00000658-194007000-00016
15. Ruiz SJ, Al Salihi S, Prieto VG, et al. Unusual cutaneous metastatic carcinoma. Ann Diagn Pathol. 2019;43:151399. doi:10.1016/j.anndiagpath.2019.08.003
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.