Back to Journals » Clinical Ophthalmology » Volume 16
Tribology and the Ocular Surface
Authors Lievens CW , Rayborn E
Received 28 January 2022
Accepted for publication 24 March 2022
Published 30 March 2022 Volume 2022:16 Pages 973—980
DOI https://doi.org/10.2147/OPTH.S360293
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Chris W Lievens,1,2 Elyse Rayborn1
1Southern College of Optometry, Memphis, TN, USA; 2Anglia Ruskin University, Cambridge, UK
Correspondence: Chris W Lievens, Southern College of Optometry, 1245 Madison Ave, Memphis, TN, 38104, USA, Tel +1 901 722 3330, Fax +1 901 722 3280, Email [email protected]
Introduction: Tribology is known as the science of friction, lubrication and the determination of what occurs when two surfaces slide against one another. The required partners in this science are a minimum of two surfaces and relative motion. Tribology could be a key factor in dissecting the issues that surround and confound dry eye in patients as well as contact lens discomfort and intolerance. Specifically, it is this issue that is a potential causative underlying factor that could lead to conditions like lid wiper epitheliopathy (LWE).
Methods: Peer-reviewed literature was reviewed as It pertains to ocular tribology and the application to the ocular anatomy. A PubMed review was performed using the keywords: tribology, friction, lid wiper epitheliopathy, contact lens, and dry eye. All manuscripts were reviewed for mentions of tribology and friction. The exact same process was performed with The Association for Research in Vision and Ophthalmology (ARVO) abstracts.
Results: In relation to the ocular surface, tribology describes the mechanical interactions between the upper and lower lid wipers and the globe. The Stribeck curve can be applied, as the sliding partners are separated by a complex, lubricating tear film. The surface brush anatomy at the eye to eyelid juncture reduces friction and alters the Stribeck curve in favor of the hydrodynamic regime, allowing for high velocity movement with minimal wear. Changes to the tear film or the introduction of a contact lens can displace the Stribeck curve, increase friction, and induce wear thus leading to patient symptomology.
Conclusion: Further studies may provide new insight into contact lens discomfort and ocular surface disease, including LWE; however, adaptation of tribology work performed in vitro to in vivo patient care is challenging.
Keywords: tribology, friction, lid wiper epitheliopathy, contact lens, dry eye
Introduction
The term, coefficient of friction is used to describe lubricity of the interactions among two partners in motion, and in contact. Coefficient of friction is defined as the ratio between friction and force.1 A low coefficient of friction implies a high lubricity among the sliding partners. Lubricity of a surface is the characteristic that allows it to glide freely against its counterpart surface without pathology, wear, or ill-effect.2 At a microscopic or macroscopic level, when this friction causes any removal of either surface material or any deformation of either surface because of the mechanical action, the result is termed wear.
Adapting the science of tribology to human tissue, like the eyelids and cornea, and artificially created very smooth surfaces, like contact lenses, is challenging. In the last 10–15 years, microtribometers have been used in an attempt to quantify the coefficients of friction among these highly lubricious materials.1,3–5 These instruments can reciprocate at very high speeds, operate with very low forces levels, and analyze microscopic samples.
Science and Background of Tribology
The foundations of understanding coefficients of friction, load, wear, speed, velocities of sliding partners, etc. are based on what is referred to as the Stribeck curve or Stribeck models (Figure 1).6 The Stribeck model identifies three unique regions of focus for sliding partners: boundary lubrication, a mixed regime, and the hydrodynamic regime. These are important foci for interpreting what is occurring in the human eye with and without a contact lens in place. First, the boundary lubrication region has immediate and very close contact of two solid surfaces, and are directly relevant when interpreting the rationale for LWE. The characteristics of each solid surface are critically important because each one’s material surface quality would be directly related to friction, given their close contact points in opposition to one another. In the eye, this region would be defined to occur at the very start, end, and subsequent return point of each blink. As the lid stops and restarts, there would exist the lowest lid velocity as the lid changes direction. When the velocity is at its lowest point, there exist the closest contact points to the globe and the alternate eye lid. When this occurs, boundary lubrication would likely be present. In addition to the low velocity is the load of ‘lid-squeezing’ as the eye lids move nasally to squeeze the tear film towards the drainage system of the puncta. According to the Stribeck curve, an increase in the coefficient of friction would be present. Surprisingly, in a normal eye (with potentially a well fit contact lens), there is not an increase in the coefficient of friction. The intricate and complex microscopic design of the human eye, eye lid, and other biologic systems (known to be lubricious under a variety of conditions) have a natural preventative measure in place to offset this portion of the Stribeck curve.
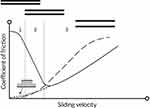 |
Figure 1 Schematic of a Stribeck curve. Linear scale: (1) boundary lubrication, (2) mixed lubrication, (3) hydrodynamic/full fluid film lubrication. The solid line is the normal Stribeck curve with significant boundary lubrication at low velocity. The dashed lines demonstrate the brush to brush effect of reducing the coefficient of friction event at low sliding velocity. Notes: Adapted from Ocul Surf, 13 (3), Pult H, Tosatti SGP, Spencer ND, Asfour JM, Ebenhoch M, Murphy PJ. Spontaneous Blinking from a Tribological Viewpoint. 236–249, Copyright 2015, with permission from Elsevier.6 |
The eye and eye lid juncture are not smooth surfaces or disjointed surfaces that act in opposition. Instead, there exists a multitude of hydrophilic, surface-tethered, sugar containing biomolecules commonly referred to as surface brushes.6 This design alters the path of the Stribeck curve. Instead of having two surfaces sliding against one another in close contact with a greater load, the surfaces are separated by the surface brushes to prevent the coefficient of friction from steeply rising (with every blink). This results in a fluid-containing soft layer on the ocular surfaces that sustain the external pressures of apposing surfaces and lowers frictional forces.7
In an ideal scenario, the presence of this thin polymer brush drastically reduces the coefficient of friction in the boundary region in a way that the theoretical transition between the boundary lubrication regime and the hydrodynamic regime disappears.6 The revised Stribeck curve would then demonstrate ‘dominance’ by the hydrodynamic regime in which there is a full fluid and lubricant film between the two sliding structures (ie no contact). This regime allows for very high velocity of movement with virtually no load or wear. The surface brush dual interface allows for the potential of full fluid, hydrodynamic regime. The eye lids are the driving engine of movement for the external ocular anatomy. The optimally designed tear film affords the ocular surfaces with a shock absorber for the most fragile tissues and transmits the kinetic energy of the spontaneous blinks to the least viscous portion of the tear film, in the mucoaqueous region.8
In a non-ideal scenario, biologic systems can be stressed and affected. Situations and factors to do so might be the environment, humidity, ambient temperature, anatomic changes, poor lubrication, fluid pH, and osmolarity.6 In these cases, external factors can cause the surface brushes to be damaged, crushed, more or less densely packed, and thinner. Any of the aforementioned conditions could then enable the typical Stribeck curve to apply, reducing the coefficient of friction and thereby initiate damage and wear. Dry eye patients and those with an intolerance to contact lenses may have ‘altered’ Stribeck curves.
The region that comes into the most contact with the globe or contact lens is the lid wiper and thereby is the most susceptible to microtrauma and vital dye staining. Damage and wear of the lid wiper (LWE) theoretically, could lead to patient symptoms. Variations of LWE imply that differing surface areas come into contact with the ocular surface patient to patient. A greater extent of staining implies greater wear. Theoretically, a greater extent and depth of damage to the lid wiper would relate to greater damage to the glycocalyx and surface brushes. Changes to the glycocalyx, would directly impact the sliding surface partners of the eye lid and ocular surface. When one sliding partner is worn, it is more likely to incur wear to the other sliding partner. Collapsed surface brushes increase friction at low blink speeds (beginning and end of the blink) by preventing the transition of boundary regime to full fluid hydrodynamic regime.
Tribology as It Applies to the Eye and Blinking
Tribology describes the mechanical interaction between two (or more) sliding surfaces. In ocular anatomy, the obvious sliding surfaces are the eyelids (specifically the upper lid wiper and the lower lid wiper that come into contact with the globe) and the cornea. The lubricating film is the tear film. In a contact lens wearer, the anatomic partners are the same and the interacting partners are the front contact lens surface and the rear contact lens surface. The most likely anatomic partners of mechanical concern with a blink would be the lid wiper and the cornea.6
The construction of the surface brushes that act to negate the left most portion of the Stribeck curve are created through secreted and membrane bound mucins that coat almost all moist surfaces in the human body, including the ocular anatomy. Specifically, the palpebral conjunctiva to include the lid wipers, the bulbar conjunctiva and the corneal surface (the ocular tribological system) are coated with mucins in the form of a glycocalyx.9 It enables cells to adhere to one another and smoothly glide against one another.
In a healthy tear film with normal mucin production, the glycocalyx and the continuous viscoelastic gels that are created on the cornea, bulbar conjunctiva and lid wipers contribute to the brush formations. So, whereas a high coefficient of friction would be expected in a nearly zero, low velocity movement of the sliding surfaces, this does not occur. The Stribeck curve, instead, is greatly displaced. In a non-healthy tear film, the opposite can occur. Other factors can also play a role to confound this system. Degrading factors could be a combination of poor mucin production, aberrant eye lid pressure, reduced blinking, surface and texture roughness, stiff contact lens modulus, excessive contact lens edge eye lid interaction, and tear film viscosity.6 These factors, when present, could alter surface brushes which would directly alter the Stribeck curve in both the low speed boundary regime and the high-speed hydrodynamic regime. As a result, patient signs and symptoms could be the result.
Blinking maintains ocular health and a smooth optical surface by ridding the tear film of degrading or older materials while smoothing out a thin refracting tear film.10 In order for the ocular surface to retain moisture and protect the surface epithelial cells and lid wiper, the tear film must be maintained and repeatedly regenerated. The precorneal tear film is very thin (approximately 4 −10 μm) and there is continual evaporation, and potential for discontinuity of the lipids, mucins, and aqueous with blinking.11 In addition to preventing evaporation, the lipid and mucin layers are thought to contribute to the maintenance of tear film spreading and prevent collapse. The maintenance of the tear film, to prevent friction and wear, is accomplished by two likely processes. First, the tears must adhere to the ocular surfaces. Membrane bound mucins accomplish this by increasing the adhesion tension (ie being more ‘sticky’ to the ocular surface).11 Secondly, the tear film surface tension must be reduced and the contact angle of a tear droplet must be close to zero. This reduction in surface tension encourages the very thin spread of tears.
In a normal patient, the tear film has to regenerate and reconstitute with spontaneous blinking that is timed before dry patches occur (the blink interval must be shorter than the tear break up time).12 Additionally, it spreads out newly generated tear materials like mucins and physically stimulates the release of lipids from the meibomian glands.13,14 Blink speed has been measured in certain patient populations. It is currently unknown how blink speed varies in one’s lifetime and varies among patent demographics. The Stribeck curve depends on the speed of the sliding partners a great deal. Higher velocities encourage separation of the sliding partners as the model transitions to a full fluid regime.
Tear Film Viscosity
Fluids that separate two sliding partners are key to how the partners interact. As the velocity of the sliding partners increase to a high level, the partners separate from one another. This leaves the fluid, itself, to be the key factor as to whether or not the sliding partners are traumatized. Specifically, at high speeds and velocities, the coefficient of friction increases due to the viscosity of the fluid that separates the partners.
To prevent trauma during normal blinking, normal tears are non-Newtonian, where the rate of shear and shear stress are not proportional. At the lowest shear rate, the viscosity of normal tears is the highest. The lowest shear rate occurs when the eyes are opened for the longest periods (interblink interval).6 This allows the spread of tears to be evenly dispersed and stable over the open ocular surface. As the lids move over the ocular surface during a spontaneous blink, the tear film’s viscosity decreases so that no surface mechanical trauma is induced.15 The viscosity of tears in a patient with dry eye has been reported to be three times as high when compared to a normal patient’s tear film.16 Additionally, it has been proposed by Bron et al14 that there exists a greater variation of tear film temperature in patients with dry eye where there is an ever increasing viscosity of the tears at the cooler ocular surface. This is a potentially critical finding as the extremely viscous tear film is likely higher than the ocular surfaces can withstand and is not well tolerated. It has been hypothesized that microtrauma results on the weakest surface and in this case would initiate LWE.6 The lid wiper is more susceptible to damage than the cornea and it is the most sensitive conjunctival tissue.17 Damage can lead to symptoms in this scenario. This mechanical potential for damage and insult is more likely to occur in contact lens wearers with dysfunctional tear film than in non-contact lens wearers. This would be due to the fact that the coefficient of friction of the eye lid against a contact lens surface would be higher than that of the eye lid against the cornea and ocular surface.5,18,19
The gel forming mucins form the surface brushes are complex linear polymers that are responsible for the non-Newtonian property of the tear film. It is believed that the mucins are the main responsible party to establish the viscosity of the tears.15 The mucin gel completely disintegrates with each blink and then then is completely restored at the end of the blink cycle.20 The tear film should quickly move to full fluid regime in low blink velocities and maintain low friction. Unlike the normal eye condition where the highest viscosity during the interblink interval shifts to a low viscosity condition during the fast-spontaneous blink phase, this is not the case for dry eye patients. Instead, the high viscosity may allow for full fluid regime at the beginning of the blink but the viscosity is not phase altered and the maintained high viscosity creates high shear forces, increased shear stress, and friction during the blink (much like a Newtonian fluid).14 This can illicit microtrauma during the high velocity blink. The shear stress can be accompanied by physical pressure to deform the sliding surfaces in a way that exceeds tolerances in corneal and lid margin sensitivity leading to patient symptomatology.6,21
Eye Lids and the Lid Wiper
Initially, it was theorized that the line of Marx was the structure that contacted the ocular surface with every blink. The line of Marx is a very small area and insult to that region could be easily determined. Once it was found that a much larger area, the lid wiper region, was in contact with the globe, pressure measurements and shear stress models could be proposed. One issue that has yet to be explored is the amount of the lid wiper (area) that can come into contact with the ocular surface. Differing areas of contact would result in differing resultant forces between the two partners and could impact symptomatology (see Figure 2). Most tribological systems in biologic anatomies involve soft surfaces.7 One characteristic of soft surfaces is that they are mobile, flexible and can be deformed by external loads. This deformation increases surface area and results in a low contact pressure and force.7 If the positioning of the lid wiper was inappropriate and anomalous, it could negatively impact the surface brush interaction and prevent full fluid regime, and thereby increase friction and microtrauma.6 It can then be theorized that staining of the lid wiper might suggest a non-ideal lid wiper area of contact with the ocular surface.
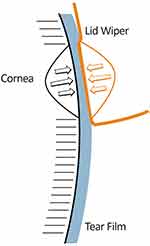 |
Figure 2 Diagram of the corneal interaction with the lid wiper. During the downward blink of the upper eyelid, the tear film thins due to the pressure exerted inwards from the cornea and lid wiper. Notes: Adapted from Ocul Surf, 13 (3), Pult H, Tosatti SGP, Spencer ND, Asfour JM, Ebenhoch M, Murphy PJ. Spontaneous Blinking from a Tribological Viewpoint. 236–249, Copyright 2015, with permission from Elsevier.6 |
Tribology and Contact Lenses
Contact lenses are optical correcting and protecting (as in the case of a bandage contact lens) devices that are designed to be biocompatible. They rest on ocular surface and dissect the tear film. In a non-contact lens wearer, the anatomy is more simplistic as there are only the ocular surface, tears, and eyelids. The contact lens adds additional complexity as there are the ocular surface, the post-lens tear film, the contact lens, the pre-lens tear film, and finally the eyelids. Soft contact lenses, in particular, have limited movement on the eye which afford visual stability. Since some lenses correct for astigmatism, lens stability, and rotational stability can be critical for good vision. Lens stability is not easy obtained as there is lens/lid interaction with spontaneous blinks. Contact lenses have physical and chemical properties that, ideally, contribute to minimal interaction between the eyelids (primarily the upper eyelid) and the ocular surface.6 Otherwise stated, there should be a low coefficient of friction between the upper eyelid and the contact lens surface. Excessive friction can lead to contact lens intolerance, discomfort, and patient symptoms and measured coefficients of friction on various contact lenses have an inverse relationship with patient comfort. In a retrospective analysis of clinical studies, there was a 0.025 reduction in the coefficient of friction that was associated with a 1 unit improvement in comfort (when using a 10 point scale).22 Contact lenses are routinely designed with materials and coatings to reduce friction between the contact lens and the lid wiper. In vitro studies have attempted to quantify the coefficient of friction on varied contact lenses but there is great challenge and complexity having a consistent and repetitive methodology to accomplish this due to the high velocity of the lid closure and the low degree of force between the lids, the lens, and the ocular surface.
Because of the complexities that contact lenses introduce to the human blinking system, contact lens manufacturers have made improvements in their surface design to afford as minimal as an opportunity to invite friction as can be produced. A contact lens that has a similar coefficient of friction as the human cornea could prevent enactment of the Stribeck curve in the same way as non-contact lens wearers. Well-designed contact lenses can offer the same brush to brush interaction as do the lid wiper and the cornea and thus prevent problems even at the lowest velocity, at the beginning and end of each blink.6 In a contact lens wearer with dry eye, the pre-lens tear film is expected to be thinner. In order to counteract the likely resulting friction, lenses require a densely packed polymeric brush that can resist high amounts of pressure.23 As such, lubricating wetting agents and surfactants have been added to lenses in an attempt to remedy and re-lubricate the ocular surface and reduce friction. Amazingly, the surfaces of most contact lenses emulate a hydrophilic surface brush that can interact with the eye lid and pre-lens tear film (and cornea via the post-lens tear film) much in the same way that the eye lids and ocular surface interact in non-contact lens wearers.6
As described in non-contact lens wearers, the viscosity of the tear film can also alter the relationship of the sliding partners. The TFOS working groups found that tear film proteins and the lipid components in the tear film of contact lens wearers can be very different than those in non-contact lens wearers.15 Both of these findings, in addition to any alterations of the mucin components would directly impact the viscosity of the pre-lens and post-lens tear films. The altered tear film composition that can increase the tear viscosity can then lead to higher shear stresses when the eye lids move at high velocities.
An estimate of the contact pressure and force exhibited by the eye lids in a contact lens wearer during a spontaneous blink is 3.5 to 4.0 kPa.3–5 With the average blink speed of 12 cm/s there exists a potential challenge of contact pressure with low speed. In tribology research, reciprocating microtribometers are used to determine the coefficient of friction measurement of contact lenses in vitro. Soft contact lenses are sensitive to water content and humidity. Contact pressure on the lens is known to cause a temporary redistribution or reduction of water content of the lens itself. Fortunately, the contact pressure is low in a blink and may not routinely do this upon blinking. In conditions where the force of a blink were to dramatically increase (such as that of a voluntary blink or anatomic abnormalities) a problem could result since it was reported that friction rises with increased levels of external force.24 Data has shown that contact lens surface friction increases as the sliding speed of microtribometers increases.4 This friction is exacerbated with time and is likely due to the contact lens drying out. Reading and computer work has been shown to reduce the frequency and completeness of blinking.12 Incomplete blinking throughout a normal day has been estimated to occur 75% of the time.12 If the contact lens becomes dry and dehydrated, the lens it at risk for surface deposits, focused areas of dewetting, corneal punctate staining and discomfort.25 It has been proposed that friction is the root cause of contact lens symptomatology.22,26 In high concentrated tasks, high speed blinks can increase friction levels and prevent the eye lid and lens interaction from being in full fluid hydrodynamic lubrication regime. Worse yet, in dry environments or in conditions whereby the lens wearer has reduced blinking, the lens surface can dry and increase friction levels further.
Research has identified reproducible differences in the contact lens surfaces with regards to friction. The posterior surface of the lens interacts with the ocular surface and corneal epithelium. The cornea is rich in sensory nerves and can detect friction - induced wear. In a similar fashion, the anterior surface of the lens slides against the lid wiper which is also a highly sensitive tissue. The measured coefficient of friction was always higher on the anterior contact lens surface when compared to the posterior surface.27 There was also more slip-stick activity on the anterior lens. The slip-stick phenomenon refers to the spontaneous jerking motion that can occur while two objects are poorly interacting with each other in boundary lubrication regime. This is an important factor when considering contact lens symptomatology and the resulting wear of LWE. An review study evaluated end of day comfort scores from over 700 contact lens clinical trials and found that the principle contact lens property associated to comfort was, in fact, coefficient of friction.26
Conclusion
In relation to the ocular surface, tribology describes the mechanical interactions between the upper and lower lid wipers and the globe. The Stribeck curve can be applied, as the sliding partners are separated by a complex, lubricating tear film. The surface brush anatomy at the eye to eyelid juncture reduces friction and alters the Stribeck curve in favor of the hydrodynamic regime, allowing for high velocity movement with minimal wear. Changes to the tear film or the introduction of a contact lens can displace the Stribeck curve, increase friction, and induce wear thus leading to patient symptomology. Further studies may provide new insight into contact lens discomfort and ocular surface disease, including LWE, however, adaptation of tribology work performed in vitro to in vivo patient care is challenging.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wilson T, Aeschlimann R, Tosatti S, Toubouti Y, Kakkassery J, Osborn Lorenz K. Coefficient of friction of human corneal tissue. Cornea. 2015;34(9):1179–1185. doi:10.1097/ICO.0000000000000524
2. Cher I. Blink-related microtrauma: when the ocular surface harms itself. Clin Exp Ophthalmol. 2003;31(3):183–190. doi:10.1046/j.1442-9071.2003.00633.x
3. Dunn A, Cobb J, Kantzios A, et al. Friction coefficient measurement of hydrogel materials on living epithelial cells. Tribol Lett. 2008;30(1):13–19. doi:10.1007/s11249-008-9306-5
4. Rennie AC, Dickrell PI, Sawyer W. Friction coefficient of soft contact lenses: measurements and modeling. Tribol Lett. 2005;18(4):499–504. doi:10.1007/s11249-005-3610-0
5. Roba M, Duncan EG, Ga H, Spencer NDTS, Tosatti SGP. Friction measurements on contact lenses in their operating environment. Tribol Lett. 2011;44(3):387–397. doi:10.1007/s11249-011-9856-9
6. Pult H, Tosatti SGP, Spencer ND, Asfour JM, Ebenhoch M, Murphy PJ. Spontaneous blinking from a tribological viewpoint. Ocul Surf. 2015;13(3):236–249. doi:10.1016/j.jtos.2014.12.004
7. Lee S, Spencer ND. Sweet, hairy, soft, and slippery. Science. 2008;319(5863):575–576. doi:10.1126/science.1153273
8. Cher I. A new look at lubrication of the ocular surface: fluid mechanics behind the blinking eyelids. Ocul Surf. 2008;6(2):79–86. doi:10.1016/s1542-0124(12)70271-9
9. Knop N, Korb DR, Blackie CA, Knop E. The lid wiper contains goblet cells and goblet cell crypts for ocular surface lubrication during the blink. Cornea. 2012;31(6):668–679. doi:10.1097/ICO.0b013e31823f8d8c
10. Jones MB, Fulford GR, Please CP, McElwain DLS, Collins MJ. Elastohydrodynamics of the eyelid wiper. Bull Math Biol. 2008;70(2):323–343. doi:10.1007/s11538-007-9252-7
11. Millar TJ, Schuett BS. The real reason for having a meibomian lipid layer covering the outer surface of the tear film - A review. Exp Eye Res. 2015;137:125–138. doi:10.1016/j.exer.2015.05.002
12. Doane MG. Interaction of eyelids and tears in corneal wetting and the dynamics of the normal human eyeblink. Am J Ophthalmol. 1980;89(4):507–516. doi:10.1016/0002-9394(80)90058-6
13. McMonnies CW. Incomplete blinking: exposure keratopathy, lid wiper epitheliopathy, dry eye, refractive surgery, and dry contact lenses. Cont Lens Anterior Eye. 2007;30(1):37–51. doi:10.1016/j.clae.2006.12.002
14. Bron AJ, Tiffany JM, Gouveia SM, Yokoi N, Voon LW. Functional aspects of the tear film lipid layer. Exp Eye Res. 2004;78(3):347–360. doi:10.1016/j.exer.2003.09.019
15. Efron N, Jones L, Bron AJ, et al. The TFOS international workshop on contact lens discomfort: report of the contact lens interactions with the ocular surface and adnexa subcommittee. Invest Ophth Vis Sci. 2013;54(11):TFOS98. doi:10.1167/iovs.13-13187
16. Tiffany JM. The viscosity of human tears. Int Ophthalmol. 1991;15(6):371–376. doi:10.1007/BF00137947
17. Navascues-Cornago M, Morgan PB, Maldonado-Codina C. Lid margin sensitivity and staining in contact lens wear versus no lens wear. Cornea. 2015;34(7):808–816. doi:10.1097/ICO.0000000000000448
18. Pult H, Purslow C, Berry M, Murphy PJ. Clinical tests for successful contact lens wear: relationship and predictive potential. Optom Vis Sci. 2008;85(10):E924–9. doi:10.1097/OPX.0b013e3181888909
19. Sterner O, Aeschlimann R, Zürcher S, et al. Friction measurements on contact lenses in a physiologically relevant environment: effect of testing conditions on friction. Investig Ophthalmol Vis Sci. 2016;57(13):5383. doi:10.1167/iovs.16-19713
20. Yokoi N, Bron AJ, Georgiev GA. The precorneal tear film as a fluid shell: the effect of blinking and saccades on tear film distribution and dynamics. Ocul Surf. 2014;12(4):252–266. doi:10.1016/j.jtos.2014.01.006
21. Golebiowski B, Chim K, So J, Jalbert I. Lid margins: sensitivity, staining, meibomian gland dysfunction, and symptoms. Optom Vis Sci. 2012;89(10):1443–1449. doi:10.1097/OPX.0b013e3182693cef
22. Kern JR, Rappon J, Bauman E, Baughn B. Assessment of the relationship between contact lens coefficient of friction and subject lens comfort. Invest Ophthalmol Vis Sci. 2013;54(1):494. doi:10.1167/iovs.12-10528
23. Wolffsohn JS, Hunt OA, Chowdhury A. Objective clinical performance of “comfort-enhanced” daily disposable soft contact lenses. Cont Lens Anterior Eye. 2010;33(2):88–92. doi:10.1016/j.clae.2010.01.004
24. Ngai V, MEdley JB, Jones L, Forrest J, Teichroeb J. Friction of contact lenses: silicone hydrogel versus conventional hydrogel. Life Cycle Tribol. 2005;48:371–379.
25. Collins M, Heron H, Larsen R, Lindner R. Blinking patterns in soft contact lens wearers can be altered with training. Am J Optom Physiol Opt. 1987;64(2):100–103. doi:10.1097/00006324-198702000-00004
26. Coles M-LC. Coefficient of friction and soft contact lens comfort. Optom Vis Sci. 2009;86:e–abstract90957.
27. Nairn J, Jiang T. Measurement of the friction and lubricity properties of contact lenses. Boston MA: ANTEC; 1995: 1–5.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
