Back to Journals » Risk Management and Healthcare Policy » Volume 16
Trends in the Burden of COPD Attributable to Ambient PM2.5 Exposure in China 1990−2019: An Age-Period-Cohort Analysis
Authors Su X, Li H, Li F, Liang H, Wei L, Shi D, Zhang J, Wang Z
Received 1 December 2022
Accepted for publication 21 January 2023
Published 26 January 2023 Volume 2023:16 Pages 69—77
DOI https://doi.org/10.2147/RMHP.S395278
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Xin Su,1,* Haifeng Li,2,* Fajun Li,3 Hongsen Liang,4 Li Wei,4 Donglei Shi,4 Junhang Zhang,4 Zhaojun Wang4
1Department of Respiratory, Hainan Hospital of PLA General Hospital, Sanya, People’s Republic of China; 2Department of Anesthesiology, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Guangzhou, People’s Republic of China; 3Department of Critical Care Medicine, The First People’s Hospital of Kunshan, Kunshan, People’s Republic of China; 4Department of Thoracic Surgery, The Seventh Affiliated Hospital, Sun Yat-sen University, Shenzhen, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Junhang Zhang; Zhaojun Wang, Department of Thoracic Surgery, The Seventh Affiliated Hospital, Sun Yat-sen University, No. 628, Zhenyuan Road, Guangming (New) Dist, Shenzhen, 518107, People’s Republic of China, Email [email protected]; [email protected]
Objective: Exposure to ambient particulate matter (PM2.5) is the leading risk factor for developing chronic obstructive pulmonary disease (COPD) in China. The present study aimed to investigate the trends in COPD mortality attributable to ambient PM2.5 exposure in China from 1990 to 2019.
Methods: Data on COPD burden attributable to ambient PM2.5 exposure in China were extracted from the Global Burden of Disease (GBD) study 2019. The estimated annual percentage change (EAPC) was used to assess COPD mortality from 1990 to 2019. The APC model was used to analyze the temporal trends in the rate of COPD mortality attributable to ambient PM2.5 exposure according to age, period, and cohort.
Results: Exposure to ambient PM2.5 contributed to 192.4 thousand deaths in 1990 and 263.6 thousand deaths in 2019. The age-standardized mortality rate (ASMR) and the age-standardized disability-adjusted life year rate (ASDR) due to ambient PM2.5 exposure showed a gradual downward trend, the ASMR and ASDR in 2019 decreased to 16.6 per 100,000 with an EAPC of − 2.82 (95% CI: − 8.61 to 3.34) and 278.6 per 100,000 with an EAPC of − 2.02 (95% CI: − 7.85 to 4.19), compared to those in 1990, respectively. The relative risk (RR) of COPD increased with age in females, while in males, mortality significantly increased from the levels among those in the 60– 64 age group to that among those in the 90– 94 age group. In the period group, the RR of COPD in males remained above 1.0 from the 2000 to 2004 period, but it gradually decreased in females. The cohort effect showed an overall downward trend.
Conclusion: Although the ASMR and ASDR are decreasing in Chinese patients with COPD, the number of deaths due to COPD is increasing. Ambient PM2.5 exposure is more harmful in males and older people above 60 years of age.
Keywords: chronic obstructive pulmonary disease, PM2.5, age-period-cohort model
Introduction
Chronic respiratory diseases are among the leading causes of incidence and mortality worldwide, and their incidence in 2017 was reported to be 544.9 million cases; chronic obstructive pulmonary disease (COPD) remained the most general disease-specific chronic respiratory disease in the world in 2017.1,2 COPD is accompanied by persistent respiratory symptoms and airflow limitation, often with airway and alveolar abnormalities associated with high exposure to toxic particles or gases.3 There is some evidence that dusty work environments play a role in COPD development.4
Air pollution from exposure to ambient particulate matter [with a diameter <2.5 µm (PM2.5)] can have severe negative health effects, including respiratory infections, COPD, and lung cancer, leading to premature death. Particles with particle size ≤2.5 μm have the characteristics of small particle size, large surface area, and strong ability to adsorb toxic substances.5 Exposure to PM2.5 has been reported to be associated not only with an increased risk of developing COPD but also with worsening of lung function and symptoms in patients with COPD.6 Ambient air pollution mainly originates from factories, traffic, and household fuel.7,8 Chen et al reported that smoking, male sex, low education level, family history of respiratory diseases, childhood respiratory infections, history of allergies, poor residential ventilation, exposure to occupational dust and biomass burning emissions, and living in and around polluted areas may be risk factors for developing COPD in Chinese population.9
Air pollution has become a serious environmental concern and has attracted increasing attention of many researchers in China.8 Several studies have investigated the relationship between PM2.5 exposure in China and disease burdens.8,10 However, few studies have been conducted on the burden of COPD attributable to ambient PM2.5 exposure in China.11–13 In the present study, we provided an assessment of current trends in COPD mortality attributable to ambient PM2.5 exposure in China from 1990 to 2019 by using an age-period-cohort (APC) analysis. We hope that our findings could provide a reference for developing effective public health policy to prevent COPD in China.
Methods
Data Sources
The number of deaths and mortality rate of COPD attributable to ambient PM2.5 exposure was extracted from the Global Burden of Disease (GBD) study 2019 (http://ghdx.healthdata.org/gbd-results-tool), which is an estimate of the world’s epidemiological data to offer a comparative assessment of disease burdens for 359 diseases and injuries and 84 risk factors from 1990 to 2019.14 The APC analysis requires 5-year intervals for each age group,15 and we excluded the group of 95-years-old and older. All methods were performed using relevant guidelines and regulations.
Descriptive Study
To assess the magnitude and direction of trends in the mortality rate and disability-adjusted life years (DALYs) of COPD over time, we used R software (version 4.1.2) to calculate the estimated annual percentage change (EAPC) and the corresponding 95% confidence interval (CI). The number of deaths, DALYs number, age-standardized mortality rate (ASMR), and the age-standardized disability-adjusted life year rate (ASDR) due to ambient PM2.5 exposure were calculated. Because EAPC is a popular tool for calculating ASR trends from 1990 to 2019,16 we also calculated EAPC of DALYs.
APC Model Analysis
The APC model is a common epidemiological, demographic, and sociological model that is applied to assess the age, period, and cohort effects on the disease mortality rate.17 Age effects represent age-related developmental changes and accumulation of exposures and are related to variations linked with different age groups. Period effects are changes over time that affect all age groups simultaneously and represent changes in disease classifications, cultures, medical and diagnostic techniques, and economies specific to a given period. Cohort effects refer to changes between populations born in a region and represent early exposure to behavioral, environmental, and socioeconomic factors. Intrinsic estimator is one of the APC models that is used to analyze the three trends simultaneously and provides relatively efficient estimation results.18
In the APC model, the rates of COPD mortality were recoded into successive 5-year age groups (25−29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79, 80–84, 85–89, 90–94), consecutive 5-year periods (1990−1994, 1995–1999, 2000–2004, 2005–2009, 2010–2014, 2015−2019), and corresponding consecutive 5-year birth cohort groups (1900−1904, 1905–1909, 1910–1914, 1915–1919, 1920–1924, 1925–1929, 1930–1934, 1935–1939, 1940–1944, 1945–1949, 1950–1954, 1955–1959, 1960–1964, 1965–1969, 1970–1974, 1975–1979, 1980–1984, 1985–1989, 1990−1994). Population aged under 25 years is rare and not included in this study; moreover, because the APC model requires 5-year intervals for each age group, we excluded the group of 95-years-old and older. The APC model estimated coefficients for the age, period, and cohort effects, and these coefficients were used to calculate the relative risk (RR) [RR= exp (coef.)]. In the present study, Stata version 17.0 (StataCorp, College Station, TX, USA) was used. The Bayesian information criterion (BIC) and Akaike information criterion (AIC) were used to estimate the degree of model fitting. p < 0.05 was considered to be statistically significant.
Results
Overall Trends in COPD Mortality Attributable to Ambient PM2.5 Exposure in China
Figure 1 shows the trend in the ASMR of COPD attributable to PM2.5 exposure from 1990 to 2019. The ASMR remained stable before 2000 and decreased markedly; the ASDR showed a similar downward trend in both male with an EAPC of −3.06 (95% CI: −8.85 to 3.09), and female with an EAPC of −3 (95% CI: −8.79 to 3.15) (Table 1). In Figure 2, the ASDR shows the same curve as that in Figure 1, but the decline was significantly faster in males than in females (Table 1), the ASDR in 2019 decreased to 356 per 100,000 with an EAPC of −2.49 (95% CI: −8.3 to 3.69) in males, and 224.7 per 100,000 with an EAPC of −2.23 (95% CI: −8.05 to 3.97) in females, compared to those in 1990, respectively.
 |
Table 1 The DALYs and Deaths of COPD in China Attributable to Ambient PM2.5 Exposure in 1990 and 2019, and Its Estimated Annual Percentage Change from 1990 to 2019 |
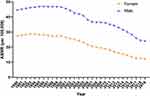 |
Figure 1 The trends in the age-standardized mortality rate (ASMR) of chronic obstructive pulmonary disease attributable to ambient PM2.5 exposure from 1990 to 2019 in China. |
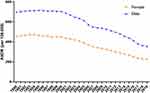 |
Figure 2 The trends in the age-standardized DALYs rate (ASDR) of chronic obstructive pulmonary disease attributable to ambient PM2.5 exposure from 1990 to 2019 in China. |
Table 1 shows the DALYs and the number of deaths due to COPD attributable to ambient PM2.5 exposure in 1990 and 2019, and its temporal trends of EAPC from 1990 to 2019. Over the past 30 years, the number of deaths increased from 192.4 thousand in 1990 to 263.6 thousand in 2019, the DALYs increased from 3969.5 thousand in 1990 to 5055.9 thousand in 2019, but the ASMR showed a downward trend with an EAPC of −2.82 (95% CI: −8.61 to 3.34) from 1990 to 2019, the ASDR also showed a decreasing trend with an EAPC of −2.02 (95% CI: −7.85 to 4.19), respectively. However, the age standardized rate (ASR) decreased from 554.8 in 1990 to 278.6 in 2019 per 100,000 in DALYs and from 33.8 in 1990 to 16.6 in 2019 per 100,000 in deaths.
APC Analysis
Age Effect
The age RR of COPD mortality attributable to ambient PM2.5 exposure in China is shown in Figure 3A. The RR of COPD increased with age in both sexes. Females and males in the 60- to 64-year-older age group were risk groups with an RR > 1. The RR in males was higher than that in females in the 85−89 and 90−94 age groups (Tables 2 and 3).
 |
Table 2 Age–Period–Cohort (APC) Model Analysis Results of COPD Mortality Attributable to Ambient PM2.5 Exposure in China Female, P < 0.05 |
 |
Table 3 Age–Period–Cohort (APC) Model Analysis Results of COPD Mortality Attributable to Ambient PM2.5 Exposure in China Male, P < 0.05 |
 |
Figure 3 Chronic obstructive pulmonary disease mortality in China attributable to ambient PM2.5 exposure relative risks due to (A) Age; (B) Period; and (C) Cohort. |
Period Effect
Figure 3B shows the period RR of COPD mortality attributable to ambient PM2.5 exposure in China. The period RR attributable to PM2.5 exposure showed a slow upward trend in males. The trends among females and males were increased in three periods (1990−1994, 1995−1999, and 2000−2004); moreover, although the trends in females began to decrease, the trend among males did not show a significant decrease. The period groups 1990−1994, 1995−1999, 2000−2004, and 2005−2009 were the four risk groups with an RR > 1 in females (Table 2), while the period groups 2000−2004, 2005−2009, 2010−2014, and 2015−2019 are the four risk groups with an RR > 1 in males (Table 3).
Cohort Effect
Figure 3C shows the cohort RR of COPD mortality in both sexes. Overall, both curves show a downward trend in mortality. The 1900−1934 birth cohort showed that the cohort RR of males is slightly higher than that of females, and it tends to be stable in both sexes. The 1900−1954 birth cohort in females and the 1900−1949 birth cohort in males are the risk groups with an RR > 1 in mortality (Tables 2 and 3).
Discussion
There is growing evidence that PM2.5 is the most harmful air pollutant to human health.19,20 With the acceleration of industrialization and urbanization, the role of PM2.5 in the development of COPD is becoming increasingly important.21 Long-term exposure to PM2.5 can result in reduced lung function and changes in airway inflammation.22 A meta-analysis showed that exposure to PM2.5 is a risk factor for developing COPD in Chinese population.9 In the present study, we investigated the long-term trends in COPD mortality attributable to ambient PM2.5 exposure in China and studied the age, period, and cohort effects on COPD mortality attributable to ambient PM2.5 exposure by using the APC model in both sexes. The findings of the present study could help to clarify the impact of PM2.5 on COPD in Chinese population.
Our study showed that the ASMR and ASDR values were decreased in both sexes, but the number of deaths and DALYs numbers were increased. The aging of the Chinese population could be the cause of this. If a population grows more quickly than exposures do, the overall burden of disease may rise despite decreasing exposures to air pollution. Besides, older people are more likely to be affected by air pollution-related diseases, aging populations are likely to face a higher burden of disease.23 Chinese populations are aging rapidly. According to the findings of the seventh Chinese population census, 264 million people aged 60 and over lived in China in 2020, making up 18.7% of the country’s overall population.24 Moreover, although the EAPC of DALYs and deaths was <0 from 1990 to 2019, which represented a downward trend, it will still bring a heavy burden on society. Because the burden of COPD death is likely to become more severe in the future, we need to place greater emphasis on the prevention of COPD.
Age, period, and cohort effects affect the risks of disease mortality in specific ways. The accumulation of exposure to risk factors has been proven to be related to the development of COPD in the elderly population.25 Age effects on COPD mortality attributable to ambient PM2.5 exposure showed that the 60- to 64-year-older age group is the risk group with an RR > 1, and this group is growing exponentially, which may be related to the decline in immunity in the elderly population; hence, we should focus on the effects of PM2.5 on the elderly population.
Period effects are often influenced by a complicated set of environmental factors and historical events. China needs to pay high attention to reducing outdoor and indoor air pollution.8 Various measures have been implemented for reducing PM2.5, including electrostatic precipitators and the use of fabric filters in large factories and more rigorous PM emission standards for power plants.26 Air pollution has decreased in the last two decades, which has effectively reduced COPD mortality in China.27 Additionally, more accessible health services and improvements in medical technology have contributed to decreased period RR of COPD mortality in China.28 In contrast, because of the industrialization process and China’s rapid economic development, PM2.5 has shown a significant upward trend due to the increase in the number of motor vehicles.29 Our study found that the trend among females was increased in the 1990−2004 periods and began to decrease, but no significant decrease in trends was observed in males. There may be the following reasons: One, male sex is a potential risk factor for COPD, which was also confirmed by a previous study.9 Two, smoking is another risk factor for COPD.30 As a result of signing the WHO the Framework Convention on Tobacco Control in 2003, China has issued a number of national and local tobacco control laws and regulations.31 There is a 52.9% prevalence of smoking among male in China, whereas only 2.4% of adult female smoke.32,33
In the present study, the 1900−1954 birth cohort in females and the 1900−1949 birth cohort in males were the risk groups with an RR > 1 in mortality; the high risk was mainly caused by the Liberation War accompanied with an underdeveloped economy and poor nutrition. Better awareness of COPD-related knowledge and nutrition may play an important role in reducing COPD mortality.34
The present study had some limitations. First, GBD 2019 could adjusting collection and evaluation methods and its data sources, improve its data quality and collect missing data, but eliminate bias could always affect the accuracy of the results. Second, the APC model considered the effects of age, period, and cohort, without further analysis of other risk factors.
Conclusion
The number of deaths and DALYs of COPD attributable to ambient PM2.5 exposure are heavy health burden in China, and the effect is particularly severe for those over 60 years of age. In the future, it is necessary to implement public policies and interventions to reduce the impact of PM2.5 in order to achieve the goal of reducing the burden of COPD in China.
Data Sharing Statement
The datasets generated and/or analysed during the current study are available in the Global Health Data Exchange (GHDx) repository [http://ghdx.healthdata.org/gbd-results-tool].
Ethics Statement
This study was approved by the Ethics Committee of the Seventh Affiliated Hospital, Sun Yat-sen University in line with the Declaration of Helsinki (KY-2022-089-01), as a result of the secondary data analysis in this study, the review board waived informed consent. Additionally, this article does not contain any personal information about patients. All authors are in agreement with the manuscript.
Acknowledgments
We thank International Science Editing (http://www.internationalscienceediting.com) for editing this manuscript.
Funding
No funding was obtained for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lancet T. GBD 2017: a fragile world. Lancet. 2018;392:1683.
2. Soriano JB, Kendrick PJ, Paulson KR. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet Respir Med. 2020;8(6):585–596. doi:10.1016/S2213-2600(20)30105-3
3. Barnes PJ, Burney PG, Silverman EK, et al. Chronic obstructive pulmonary disease. Nat Rev Dis Primers. 2015;1:15076. doi:10.1038/nrdp.2015.76
4. Hooper R, Burney P, Vollmer WM, et al. Risk factors for COPD spirometrically defined from the lower limit of normal in the BOLD project. Eur Respir J. 2012;39(6):1343–1353. doi:10.1183/09031936.00002711
5. Kim Y, Seo J, Kim JY, Lee JY, Kim H, Kim BM. Characterization of PM2.5 and identification of transported secondary and biomass burning contribution in Seoul, Korea. Environ Sci Pollut Res Int. 2018;25(5):4330–4343. doi:10.1007/s11356-017-0772-x
6. Zhao B, Zheng H, Wang S, et al. Change in household fuels dominates the decrease in PM2.5 exposure and premature mortality in China in 2005–2015. Proc Natl Acad Sci U S A. 2018;115(49):12401–12406. doi:10.1073/pnas.1812955115
7. Apte JS, Brauer M, Cohen AJ, Ezzati M, Pope CA. Ambient PM2.5 reduces global and regional life expectancy. Environ Sci Technol Lett. 2018;5(9):546–551. doi:10.1021/acs.estlett.8b00360
8. Wu X, Zhu B, Zhou J, Bi Y, Xu S, Zhou B. The epidemiological trends in the burden of lung cancer attributable to PM2.5. Exposure in China BMC Public Health. 2021;21:737. doi:10.1186/s12889-021-10765-1
9. Chen H, Liu X, Gao X, et al. Epidemiological evidence relating risk factors to chronic obstructive pulmonary disease in China: a systematic review and meta-analysis. PLoS One. 2021;16(12):e0261692. doi:10.1371/journal.pone.0261692
10. Xia S-Y, Huang D-S, Jia H, et al. Relationship between atmospheric pollutants and risk of death caused by cardiovascular and respiratory diseases and malignant tumors in Shenyang, China, from 2013 to 2016: an ecological research. Chin Med J. 2019;132(19):2269–2277. doi:10.1097/CM9.0000000000000453
11. Zhao C, Wang W, Wen H, et al. Effects of green spaces on alleviating mortality attributable to PM2.5 in China. Environ Sci Pollut Res Int. 2022;2022:1–11.
12. Su J, Ye Q, Zhang D, et al. Joint association of cigarette smoking and PM2.5 with COPD among urban and rural adults in regional China. BMC Pulm Med. 2021;21(1):87. doi:10.1186/s12890-021-01465-y
13. Maji KJ, Arora M, Dikshit AK. Burden of disease attributed to ambient PM2.5 and PM10 exposure in 190 cities in China. Environ Sci Pollut Res Int. 2017;24(12):11559–11572.
14. Wang Z, Hu L, Li J, Wei L, Zhang J, Zhou J. Magnitude, temporal trends and inequality in global burden of tracheal, bronchus and lung cancer: findings from the global burden of disease study 2017. BMJ Glob Health. 2020;5(10):e002788. doi:10.1136/bmjgh-2020-002788
15. Wang L, Wang W. Temporal trends in notification and mortality of tuberculosis in China, 2004–2019: a joinpoint and age-period-cohort analysis. Int J Environ Res Public Health. 2021;18:5607.
16. Li Z, Fang Y, Chen H, et al. Spatiotemporal trends of the global burden of melanoma in 204 countries and territories from 1990 to 2019: results from the 2019 global burden of disease study. Neoplasia. 2022;24(1):12–21. doi:10.1016/j.neo.2021.11.013
17. Wen H, Xie C, Wang L, et al. Difference in long-term trends in COPD mortality between China and the U.S., 1992(-)2017: an age(-)period(-)cohort analysis. Int J Environ Res Public Health. 2019;16(9):1529. doi:10.3390/ijerph16091529
18. Yang Y, Schulhofer‐Wohl S, Fu W, Land K. The intrinsic estimator for age-period-cohort analysis: what it is and how to use it. Am J Sociol. 2008;113(6):1697–1736. doi:10.1086/587154
19. World Health Organization. Health consequences of air pollution on populations. Available from: https://www.who.int/news/item/15-11-2019-what-are-health-consequences-of-air-pollution-on-populations.
20. Bu X, Xie Z, Liu J, et al. Global PM2.5-attributable health burden from 1990 to 2017: estimates from the global burden of disease study 2017. Environ Res. 2021;197:111123. doi:10.1016/j.envres.2021.111123
21. Zou W, Wang X, Sun R, et al. PM2.5 induces airway remodeling in chronic obstructive pulmonary diseases via the Wnt5a/beta-catenin pathway. Int J Chron Obstruct Pulmon Dis. 2021;16:3285–3295. doi:10.2147/COPD.S334439
22. Zielinski M, Gasior M, Jastrzebski D, Desperak A, Ziora D. Influence of particulate matter air pollution on exacerbation of chronic obstructive pulmonary disease depending on aerodynamic diameter and the time of exposure in the selected population with coexistent cardiovascular diseases. Adv Respir Med. 2018;86:227–233. doi:10.5603/ARM.2018.0036
23. State of global air. Health impacts of PM2.5. Available from: https://www.stateofglobalair.org/health/pm#growing-burden.
24. Lam KB, Yin P, Jiang CQ, et al. Past dust and GAS/FUME exposure and COPD in Chinese: the Guangzhou biobank cohort study. Respir Med. 2012;106:1421–1428. doi:10.1016/j.rmed.2012.05.009
25. Xiao L, Fu J, Lin L, Han Y. Temporal trends in incidence of nutritional deficiency among older adults in China: a secondary analysis of the global burden of disease study 1990–2019. Nutrients. 2022;14(23):5008. doi:10.3390/nu14235008
26. Wang S, Hao J. Air quality management in China: issues, challenges, and options. J Environ Sci. 2012;24(1):2–13. doi:10.1016/S1001-0742(11)60724-9
27. Cheng Z, Jiang JK, Fajardo O, Wang SX, Hao JM. Characteristics and health impacts of particulate matter pollution in China (2001–2011). Atmos Environ. 2013;65:186–194. doi:10.1016/j.atmosenv.2012.10.022
28. Yin P, Wang H, Vos T, et al. A subnational analysis of mortality and prevalence of COPD in China from 1990 to 2013: findings from the global burden of disease study 2013. Chest. 2016;150:1269–1280. doi:10.1016/j.chest.2016.08.1474
29. Liu M, Huang Y, Ma Z, et al. Spatial and temporal trends in the mortality burden of air pollution in China: 2004–2012. Environ Int. 2017;98:75–81. doi:10.1016/j.envint.2016.10.003
30. Zhu B, Wang Y, Ming J, Chen W, Zhang L. Disease burden of COPD in China: a systematic review. Int J Chron Obstruct Pulmon Dis. 2018;13:1353–1364. doi:10.2147/COPD.S161555
31. Wang M, Luo X, Xu S, et al. Trends in smoking prevalence and implication for chronic diseases in China: serial national cross-sectional surveys from 2003 to 2013. Lancet Respir Med. 2019;7(1):35–45. doi:10.1016/S2213-2600(18)30432-6
32. Sansone N, Yong HH, Li L, Jiang Y, Fong GT. Perceived acceptability of female smoking in China. Tob Control. 2015;24(Suppl 4):iv48–iv54. doi:10.1136/tobaccocontrol-2015-052380
33. Li Q, Hsia J, Yang G. Prevalence of smoking in China in 2010. N Engl J Med. 2011;364(25):2469–2470. doi:10.1056/NEJMc1102459
34. Cohen AK, Syme SL. Education: a missed opportunity for public health intervention. Am J Public Health. 2013;103:997–1001. doi:10.2105/AJPH.2012.300993
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
