Back to Journals » Open Access Emergency Medicine » Volume 14
Trends and Outcomes of Acute Poisoning in Felege Hiwot Comprehensive Specialized Hospital Medical Intensive Care Units: Retrospective Study
Authors Shumet A, Shiferaw N, Mekonnen D , Asemahagn MA
Received 23 August 2022
Accepted for publication 20 December 2022
Published 30 December 2022 Volume 2022:14 Pages 649—656
DOI https://doi.org/10.2147/OAEM.S385420
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Abebe Shumet,1 Niguse Shiferaw,2 Daniel Mekonnen,3 Mulusew Andualem Asemahagn4
1Department of Internal Medicine, School of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia; 2Critical Care Nursing Unit, Felege Hiwot Specialized Hospital, Bahir Dar, Ethiopia; 3Department of Medical Laboratory Sciences, College of Medicine and Health Sciences, Dar University, Bahir Dar, Ethiopia; 4School of Public Health, College of Medicine and Health Sciences, Dar University, Bahir Dar, Ethiopia
Correspondence: Abebe Shumet Mitiku, Bahir Dar University, Bahir Dar, Ethiopia, Tel +251912064411, Email [email protected]; [email protected]
Background: Acute poisoning with agrochemicals, medicines and different environmental exposures continues to be a global health problems. However, with our search for reports about acute poisoning, there was no data regarding a change in trends and outcomes of acute poisoning in Ethiopia and its districts.
Objective: This study was to determine the burden of poison-related health hazards, identify poisoning substances, and clinical outcomes of poisoning cases admitted to Felege Hiwot Comprehensive Specialized Hospital- Medical intensive care unit (FHCSH-MICU), Bahir Dar, Ethiopia.
Methods: A retrospective hospital-based study was conducted using patient data archived from March 2019 to February 2020 at FHCSH-MICU. Collected data were analyzed using Statistical Package for Social Sciences (SPSS) software version 26 and descriptive statistics such as measures of central tendency and proportions were computed. The results were reported as text narrations, figures and tables.
Results: A total 121 poisoned patients were identified from the patient registration log books. Among the total FHCSH-MICU cases registered, acute poisoning accounted for 17.0%. Of 121 poison cases, 118 (98.3%) were due to suicide attempts with the female to male ratio being 1.5:1. The majority, 65 (54.0%), of cases were in the range of 21– 30 years age. Nearly two-thirds, 75 (62.0%), of the poisoning cases died, accounting for 21.6% of all deaths in the FHCSH-MICU. The most common poisoning substance was aluminum phosphide, 92 (76%).
Conclusion and Recommendations: Aluminum phosphide became the leading poisoning substance in the study area. Nearly two-thirds of the poisoning cases died. Hence, aluminum phosphide must be placed in secured and inaccessible places and it should be replaced by less poisonous rodenticides. Health education and awareness creation about this lethal toxin are strongly advisable.
Keywords: trends, poisoning, Felege Hiwot Hospital, medical intensive care unit, Ethiopia
Corrigendum for this paper has been published.
Background
Poison is “any substance that, when relatively small amounts are ingested, inhaled, absorbed, applied to, injected into, or developed within the body, has chemical action that causes damage to structure or disturbance of function, producing symptoms, illness, or death”.1
The diagnostic information was obtained through interview with the patients and families, and studying the remaining agent or its container. A common type of poisoning substance was aluminum phosphide. Aluminum phosphide is used to kill rodents and pests to protect stored grains by fumigation. This fumigant was commonly named Phostoxin, and its formulation was dark gray tablets. Each tablet was 3 gm in weight with a composition of aluminum phosphide (56%) and aluminum carbamate (44%).1,4 Its commercial formulation with 55% to 75% active ingredients were solid tablets. Pellets of solid ALP react with water and form highly toxic phosphine gas. The rate of phosphine gas formation depends on humidity and ambient temperature.3,4
The other types of poisoning agents were organophosphates used as pesticides and insecticides. They are easily available in marketplaces without appropriate controlling and monitoring systems. Organophosphate poisoning is a health-related concern in underdeveloped areas, with high morbidity and mortality.3,4
Poison affects most organ systems. Its effect on the nervous system is a loss of consciousness; on the respiratory system, it decreases reflexes that protect airways and aspirating from the gastro-intestinal tract into the airways and an absence ofrespiration derives from inadequate ventilation, resulting in respiratory failure. Massive aspiration of gastric contents into the lungs with chemical pneumonitis and pulmonary damage is a major cause of death. The effect of poison on the heart is abnormal cardiovascular function with hypotension resulting from decreased contractility of the heart and a loss of bodily fluid; hypervolemia from fluid overload during resuscitation or abnormal cardiac rhythms (arrhythmias). 4
Poison can kill cells of the body by cellular hypoxia (low cellular level oxygen) from inadequate oxygen for normal cellular metabolism called respiration. Cellular hypoxia further affects organs, for example, it can damage the brain resulting in seizure (abnormal body movement) from hyperactivity of muscles or loss of entire body control. Renal failure results from damage of muscles by poison and accumulation of toxin products like myoglobin in the renal system.
Poisoning substances can be ingested into the human body accidentally and/or intentionally. A suicide means an intentional intake of poisoning substances and it is a major preventable cause of death throughout the world, both in developed and developing nations.2,3,5
The victims expose themselves to poisonous agents to self-harm or to seek attention of other persons.3,4 Depending on the actual intention of the victims, these kings of toxic exposures result in suicide or para-suicide.3
According to the World Health Organization (WHO) reports, poisoning contributed to nearly 0.3 million deaths annually.5 The deadliest poison worldwide was reported from acute pesticide poisoning.1–6
Promotion and the wide use of pesticides to improve agricultural products results in the easy accessibility of these highly toxic chemicals in the homes of farmers.4 Intentional self-poisoning (suicidal) behavior was the concern of the WHO under the department of Mental Health and Substance Abuse.5,6,8
Despite the WHO organized joint Departments of Violence and Injury Prevention and International Program on Chemical Safety with Mental Health, and the launched initiative in 2004 to reduce global poison deaths, the burden of poisoning has increased and become a public health issue.5,6
Poisoning is always a concern to the communities and law officials that ready availability and accessibility of these chemicals for homicide or tamper intent should be under control.1 Thus, the sale of potentially poisonous agents must be recorded and maintained. There must be laws for pharmacies to maintain a “poison register” recording the sales of toxic substances. These records should include the date of purchase, name and address of the buyers, the information regarding poison agents sold, their dose and intended use.1,2
The trends of acute poisoning varied from nation to nation, depending on geographic factors, poison availability and ready accessibility, religious and cultural practices of the communities.2
Common reasons for victims to be poisoned were losing their businesses, break-up of relationship, failing in examinations, labial emotions, having health-related issues and poison substances accessibility at marketplaces even on straight roads are the commonly given reasons for increasing intentional poisoning in previous studies.2,3
The majority of the Ethiopian population is agrarian and acute poisoning from pesticide agents and chemical fertilizers is considered to be high.7 In our community, the issue of poison becomes a serious agenda. Different studies from other hospitals in Ethiopia showed pesticides and household cleansing agents were the commonest causes of poisonings.9–11 Everywhere accessibility, awareness of our community, and socio-economically related affairs are identified factors for the increasing burden of poison cases. In addition, there is a lack of data on changes in trends of poisoning and outcomes in Ethiopia and its districts. Therefore, the study was to determine the trends and outcomes of poison in Felege Hiwot Comprehensive Specialized Hospital- Medical intensive care unit (FHCSH-MICU), Bahir Dar, Ethiopia.
Methods
Study Area, Design and Period
A retrospective hospital-based study was conducted at FHSH-MICU using patients’ log books and charts registered from March 1, 2019 to February 30, 2020. Felege-Hiwot Compressive Specialized Hospital is a government referral hospital, in the city of Bahir Dar, the capital city of Amara regional state. The city is 536 km northwest from Addis Ababa, the capital city of the country. The hospital serves about 5 million people and has a 12-bed adult MICU.
Study Population
All admitted adult patients to the FHCSH-MICU from March 2019 to February 2020 were considered as the study population.
Eligible Participants
All poisoned cases admitted to the FHCSH-MICU with complete data on -socio-demographic, poisoned chemical, and outcomes were included.
Sample Size
All poisoned cases admitted to the FHSH-MICU from March 2019 to February 2020 were considered as the sample size. Based on that, a total of 121 poisoned patients were studied.
Study Variables
The extracted variables included age, sex, residence and poison substances used, reason, route of poison entry, season, length of stay in the MICU, and outcomes.
Data Collection Tools and Procedures
Trained nurses collected data using a data extraction checklist from July 1 to September 30, 2021. Data collectors extracted the required data from patients’ registration log books and patients’ charts after getting permission from the hospital manager and the medical card unit head. They first did the separation of patients’ charts as poison and non-poison. Then, they extracted data from charts of poisoned cases. They cross-checked data from patients’ registration log books. The research teams supervised data collection procedures.
Data Quality Assurance
Nurses and doctors assigned for data collection were trained for one day about the data extraction checklist, how to collect data, data quality, and data confidentiality issues. Cross-checking of patients’ chart data with registration log books was made. Data collection was fully supervised with feedback on the observed gaps and clarity questions raised from data collectors. Data were entered into excel carefully. Data coding, checking for completeness and data clearances were done after data entry using SPSS software version 26.
Data Management and Analysis
Data entered into excel were transferred into SPSS software version 26 for additional data clearance and analyzed. Data completeness check, clearance, and coding were done. Descriptive statistics such as measures of central tendencies, proportions, and cross-tabulations were computed. The results were summarized and presented using text narrations, tables, and figures.
Ethical Issues
This study was conducted based on Helsinki declaration and national research ethics guidelines. We obtained ethical clearance from Ethical Review Committee of school of medicine and health sciences, Bahir Dar University, with protocol number: 518/2022. Felege Hiwot specialized hospital office gave us permission to conduct the study. We waived patients’ informed consents in this retrospective medical chart reviews and any information taken from the patient’s chart was kept confidential through anonymity using codes.
Results
Characteristics of Poisoned Cases
Of the total 716 critically sick patients admitted to FHCSH-MICU from March 2019 to February 2020, 121 (16.9%) cases were acutely poisoned patients. Of those poisoned patients, 73 (60.33%) were female and 65 (54%) were between 21–30 years of age. Most of the poisoned cases admitted to MICU arrived at our emergency with shock and respiratory failure. Thirty-six (29.8%) of the poisoned cases were residents of Bahir Dar City (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Poisoned Cases at FHCSH-MICU from March 2019 to February 2020 |
Poisoning Substances, Reasons for Poisoning, and Outcomes of Poisoning
Among all poisoned cases, 92 (76.0%) were due to aluminum phosphide-ALP. Thirty-five (28.9%) of poison incident cases occurred in the winter season. One hundred eighteen (97.5%) of the poisoned cases were due to intentional suicidal attempts and only three (2.50%) were accidentally exposed due to carbon monoxide inhalation (Table 2).
 |
Table 2 Types of Poisoning Substances, the Reason for Poisoning, and Outcomes of Poisoning Among Poison Cases Admitted at FHSH-MICU from March 2019 to February 2020 |
Trend of Admission Cases at FHCSH-MICU
During the study period, an average of 60 and 11 critical and poisoned patients respectively were admitted to FHCSH-MICU each month. The trend of critical patients’ admission showed a decreasing order, whereas, the trend of admission for poisoned patients was more or less stable or similar trend. The highest admission for critical patients was 83 in April and the lowest was 42 in December 2019. Similarly, poisoned cases (14) were registered in April and the lowest (7) cases were registered in September 2019 (Figure 1).
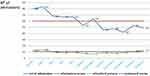 |
Figure 1 Trends of FHCSH-MICU admission per month comparing all cases versus poisoned patients from March 2019 to February 2020. |
Despite a decline in total admissions to the ICU, the total poison admission was stable during the study period.
Trends of Deaths from Poisoned Cases in the FHCSH-MICU
The annual mean mortality rates of critical patients and poisoned patients in the MICU were 46.7% and 62.5%, respectively. The death rate from poisoned patients showed an unstable trend that ranges from 22.2% in June to 87.5% in November 2019. The trends of both cases showed an increasing order from June to November (Figure 2).
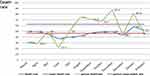 |
Figure 2 Crude versus poisoned death rates per month in FHCSH-MICU from March 2019 to February 2020. |
Discussion
Poisoning is an acute medical condition that requires prompt medical intervention. However, this study revealed that the majority of the cases, 101 (83.5%), arrived at the hospital after 3 hours. It is in line with reports from other Ethiopia hospitals.9,11 The explanation could be cultural practices, such as ingestion of milk at home, visiting holy water, before healthcare is sought and the inaccessibility of health services.
The poisoning rate has increased around the world, it has been a serious health and socio-economical problem.5 This situation is also happening in Ethiopia. Based on our study, 121 poisoned cases were admitted to FHCSH-MICU care and contributed to 17% of all FHCSH-MICU admissions. This figure is higher than reports from other Ethiopian hospital's ICU-poisoned admissions as our study focused on poisoned cases admitted to MICU care, unlike other reports.9–11 The increment of acute poisoning implies that people are accessing and using poisoning substances without knowing their effects on their health. This will be a more serious health problem in the future if it continues without interventions since most farmers are using these substances for their agricultural activities. Therefore, it is time for the government and other concerned offices to take action among the population on how to properly use, and store such poisoning substances and seek treatment if once exposed to such substances. Unless the government acts on preventing deaths from poisoning, more people will die and people will never use these and other important healthy substances for agricultural activities. This will directly or indirectly affect agricultural practices and productivity of the country.
Most of the poisoned patients, 118 (98.3%), were due to suicide attempts and only 3 (1.7%) were accidental poisonings. This finding was similar to findings at Tikur Anbesa Specialized Hospital (Ethiopia) which reported 96.5% intentional poisoning.9 However, it became higher compared to other study findings from other Ethiopian hospitals: 60% from the University of Gondar teaching referral hospital,10 and 54% intentional poisoning from Jima University hospital.11 The discrepancy might be related to variations in the study period that has a potential connection to access and use of such poisoning substances for agricultural practices. Our study was conducted in 2021, where the Ethiopian government has worked more to scale up agricultural practices and productivity using all the possible agricultural inputs compared to the situation in the former study periods. This might create opportunities for people to access and use these substances for suicidal practices.
This study finding was also found to be higher compared to reports from Turkey hospital’s intensive care units that reported suicide attempts varied from 10.2% to 68%.8,9 This variation might be attributed to differences in awareness creation, storage conditions, access to substances, and the type and safety of substances used for agricultural practices.12,13 These figures revealed that intentional poisoning is a major problem in Ethiopia and beyond. A suicide attempt by self-poisoning is high among the young age group of the population during which age major life changes occur, such as the age of university completion, employment, and the time of marriage and departure from the family. For instance, in this study, among all poisoned patients, 65 (54.0%) were found to be between 21−30 years of age. A similar study in Turkey showed that 56.9% of poisoned patients were between 15–35 years of age.8 The main reasons for a high rate of poisoning in this age group were social problems such as separation of family, unsettled life conditions, unemployment and quarreling. Similarly, the rate of poisoning was higher in females than in males in different studies including this study.8,9 It is known that adolescent aged females show a high rate of stress due to gender-related issues like love failure and mental conflicts. Additionally, family arguments, job problems, poverty, and being unable to have open discussions with families can be incited as possible causes.
According to this report the most likely, 92 (76.1%), poisoning substance was aluminum phosphide-ALP. This is different from findings in Turkey MICU, where drug related poisonings (58.4%) were major problems.9 This might be related to the accessibility of the ALP over the counter to use for rat poison. The trends and outcomes of poisoning changed.14–17 Moreover, this report is in apparent contradiction with other reports in Ethiopia where house cleaning agents and organophosphates (OP) were the most common poison agents mentioned by other previous studies.10,11 For instance, in Tikur Anbesa Specialized Hospital, household cleansing agents accounted for 43.1% followed by organophosphate (21.6%).9 Reports from Gondar teaching referral hospital showed that organophosphates accounted for 35% whereas bleaching agents accounted for 25% of poisoned cases.10 Similarly, in Jima, the leading poisoning chemicals were household cleaning agents (43, 41.7%) and organophosphate products (28, 27.2%). There was no antidote for ALP and therapy was supportive care with fluid resuscitation, MgSO4 infusion, calcium gluconate, glucocorticoid, and mechanical ventilation. Gastric lavage is not recommended care as it hastens generation of its toxic phosphine gas.
Poisoning has contributed to 21.6% of the total MICU deaths and the death rate for poison was 62%. The majority of deaths, 72 (96%), were from aluminum phosphate (ALP). This study implies that there was a higher mortality rate when compared to prior local studies.9–11 and studies done in Turkey.8 The higher mortality rate in this report might be linked with the types of poisoning substance used, ALP. ALP has no specific antidote management.18 Additionally, the difference in delays to reach health facilities, more than 3 hours, might contribute to the discrepancy in terms of the death rate among studies.
Conclusion and Recommendations
Based on this study, a significant number of patients from the emergency units were due to acute poisoning. The pattern of acute poisoning changed to more fatal poison agents, ALP, which had a higher MICU mortality rate. Poisoning particularly affects young females, and most of them were suicide attempts that result in more deaths. Hence, regulatory agencies should restrict the open sales of such poisonous substances. Sellers should maintain a “poison register”, recording the sale of any toxic chemicals. Increasing the community’s awareness of handling and management of poisoning substances also has high importance. It is also advisable to establish poison management centers with diagnostic capacity and treatment protocols. Finally, poison survivors should be linked to the district police station and psychiatrist before being discharged from the hospital. A further, community-based, large-scale mixed study is recommended to determine the magnitude of poisoning, identify contributing factors, and design mitigating mechanisms.
Abbreviations
ALP, aluminum phosphate poisoning; ARDS, acute respiratory distress syndrome; CO, carbon monoxide; FHSH, Felege Hiwot Specialized Hospital; HF, heath facility; HCW, health care workers; MICU, medical intensive care unit; OP, organophosphate poisoning; WHO, World Health Organization.
Data and Materials Availability
Data supporting the conclusions of this study are included in the report. Any required materials can be available upon request.
Ethical Issues
Ethical approval was obtained from the Ethical Review committee of the School of Medicine and Health Sciences at Bahir Dar University. We conducted this study under the Declaration of Helsinki. Data confidentiality and privacy were maintained by coding, deidentifying personal identifiers, and limiting others to access the datasets.
Acknowledgments
We would like to thank the FHSH-MICU staff for their assistance during the data collection.
Disclosure
The authors declared that they have no competing interests.
References
1. Deichman WB, Henschler D, Keil G. What is there that is not poison? A study of the third defense by paracelsus. Arch Toxicol. 1986;58:207–213. doi:10.1007/BF00297107
2. Mohamed F, Perera A, Wijayaweera K, et al. The prevalence of previous self-harm amongst self-poisoning patients in Sri Lanka. Soc Psychiatry Psychiatr Epidemiol. 2011;46(6):517–520. doi:10.1007/s00127-010-0217-z
3. Malanga N. Acute Poisoning in Three African Countries: Botswana, South Africa and Uganda Doctoral dissertation. University of Limpopo; 2011.
4. Razwiedani LL, Rautenbach PGD. Epidemiology of organophosphate poisoning in the Tshwane District of South Africa. Environ Health Insights. 2017;24:1178630217694149.
5. World Health Organization. Clinical management of acute pesticide intoxication: prevention of suicidal behaviors; 2008.
6. Khadka SB, Ale SB. A study of poisoning cases in emergency Kathmandu Medical College Teaching Hospital. Alcohol. 2005;9:13–14.
7. Mustafa Cengiz MD, Baysal Z. characteristics of poisoning cases in adult intensive care unit in Sanliurfa, Turkey. Saudi Med J. 2006;27:497.
8. Satar S, Seydaoglu G, Sebe A. Trends in acute adult poisoning in ten years period in Turkey: factors affecting the hazardous outcome. Bratisl Lek Listy. 2014;110:404–411.
9. Getie A, Belayneh YM. A retrospective study of acute poisoning cases and their management at emergency department of Dessie Referral Hospital, Northeast Ethiopia. Drug Health Patient Saf. 2020;12:41–48. PMID: 32184673; PMCID: PMC7062390. doi:10.2147/DHPS.S241413
10. Desalew M, Aklilu A, Amanuel A, Addisu M, Ethiopia T. Pattern of acute adult poisoning at Tikur Anbessa specialized teaching hospital, a retrospective study, Ethiopia. Hum Exp Toxicol. 2011;30:523–527. doi:10.1177/0960327110377520
11. Adinew GM, Asrie AB, Birru EM. Pattern of acute organophosphorus poisoning at University of Gondar Teaching Hospital, Northwest Ethiopia. BMC Res Notes. 2017;10(1):149. PMID: 28376842; PMCID: PMC5381028. doi:10.1186/s13104-017-2464-5
12. Adinew GM, Woredekal AT, DeVos EL, et al. Poisoning cases and their management in emergency centers of government hospitals in northwest Ethiopia. Afr J Emerg Med. 2017;7:74–78. doi:10.1016/j.afjem.2017.04.005
13. Agrawal K, Bansal A. Aluminum phosphide poisoning: possible role of supportive measures in the absences of specific antidotes in India. Indian J Crit Care Med. 2015;19:109. doi:10.4103/0972-5229.151019
14. Bardin PG, Vaneeden SF, Joubert JR. Intensive care management acute organophosphate poisoning A7-year experience in the western Cape; 2010.
15. Jayashree M, Singhi S. Changing trends and predictors of outcome in patients with acute poisoning admitted to the intensive Care, India. J Trop Pediatr. 2011;57:340. doi:10.1093/tropej/fmq099
16. Fathelrahman AI, Zain ZM. Self-poisoning by drugs and chemicals: variations in demographics, associated factors and final outcomes. Gen Hosp Psychiatry. 2008;30(5):467–470. doi:10.1016/j.genhosppsych.2008.04.004
17. Sungur M, Güven M. Intensive care management of organophosphate insecticide poisoning. Critical Care. 2001;5(4):1–5. doi:10.1186/cc1025
18. Hosseinian A, Pakravan N, Rafiei A, Feyzbakhsh SM. aluminum phosphide poisoning known as rice tablet: a common toxicity in North Iran. Indian J Med Sci. 2011;65:143. doi:10.4103/0019-5359.104777
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
