Back to Journals » International Journal of Women's Health » Volume 13
Trends and Determinants of Female Genital Mutilation in Ethiopia: Multilevel Analysis of 2000, 2005 and 2016 Ethiopian Demographic and Health Surveys
Authors Alemu AA
Received 21 October 2020
Accepted for publication 15 December 2020
Published 6 January 2021 Volume 2021:13 Pages 19—29
DOI https://doi.org/10.2147/IJWH.S287643
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Elie Al-Chaer
Addisu Alehegn Alemu
College of Health Sciences, Debre Markos University, Debre Markos, Ethiopia
Correspondence: Addisu Alehegn Alemu
College of Health Sciences, Debre Markos University, Debre Markos, Ethiopia
Email [email protected]
Background: Female genital mutilation (FGM) is a harmful practice that causes health-related problems in the life of the affected women and girls. Though FGM is declared as a human right violation, studies revealed it is being practiced throughout Ethiopia. Therefore, this study was conducted to assess the prevalence, trends, and predictors of FGM among reproductive-aged (1549 years) women in Ethiopia.
Methods: Trends of FGM among reproductive-age women were estimated using the three Ethiopian Demographic and Health Survey (EDHS): 2000 (n=15,367), 2005 (n=14,070) and 2016 (n=7248) data. Multilevel logistic regression analysis was conducted to identify both individual- and community-level factors of FGM using the latest (2016) EDHS. To adjust potential confounders, the analysis was conducted considering sample weighting, clustering, and stratifications using STATA-14 software.
Results: The prevalence of FGM among women of reproductive age in Ethiopia decreased from 79.91% in 2000 to 70.37% in 2016. Similarly, FGM among daughters of circumcised mothers decreased from 56.16% in 2000 to 16.76% in 2016. Being Muslim (adjusted odds ratio [AOR] 5.48; 95% confidence interval [CI]: 4.23, 7.09), attending higher education (AOR 0.40; 95% CI: 0.29, 0.54), 45– 49 years old (AOR 5.06; 95% CI: 3.38, 7.57), marriage at ≥ 18 years (AOR 0.80; 95% CI: 0.66, 0.96), not working (AOR 1.20; 95% CI: 1.02, 1.41), married (AOR 1.41; 95% CI: 1.12, 1.77) and residing in peripheral region (AOR 3.0.4; 95% CI: 1.96, 4.70) were determinants of FGM.
Conclusion: Though the reduction of FGM among women of reproductive age in Ethiopia was minimal, it was encouraging among daughters of circumcised women over the last 16 years. Education, religion, age, age at marriage, occupation, marital status, and geographical regions were determinants of FGM. Combined and integrated interventions based on the identified factors are recommended to abandon FGM in Ethiopia.
Keywords: FGM, mutilation, harmful practices, DHS, multilevel analysis, Ethiopia
Introduction
Female genital mutilation (FGM), also known as female circumcision, is a partial or total removal of external female genitalia including injury of their genital organs for non-medical reasons.1–3 According to the World Health Organization (WHO), FGM is classified into four types. Type I is a partial or total removal of clitoral glans and prepuce. Type II is the removal of the clitoris and labia minora partially or totally. Type III is known as infibulation involves removing and apposing of labia minora with the clitoris, creates a covering seal, and narrowing the vaginal opening. Type IV is when it incorporates all other forms of harmful procedures on female genitalia such as incising the clitoris or labia, cutting the vagina, and inserting substances or herbs with the assumption of narrowing the vault of the vagina.4
FGM is a human right violation4 and a reason for many short-term and long-term negative health impacts. Severe pain, hemorrhage, and infection are among short-term complications5 that can occur during pregnancy and childbirth,6,7 whereas sexual dysfunction,8 depression6 and gynecologic problems like fistula9,10 are some of the long-term complications due to FGM. Though FGM is usually performed between infancy and 15 years of age,11 victims suffer from complications throughout their lives,4 and the procedure can be even fatal.1 FGM is also associated with a reduced level of antenatal care12 and other health-care service utilization13,14 and increases the risk of Human papillomavirus infection.15
Despite many physical, sexual, and psychological problems are associated with FGM, it is still practiced in greater than 30 countries mainly in the west and east Africa including Ethiopia.2 United Nations Population Fund (UNFPA) and the United Nations Children’s Fund (UNICEF) have a program focusing on empowering women through education, community discussion, and national commitments to abandon FGM practice.16 Likewise, the Ethiopian government planned to end FGM by 2025 through public education campaigns.17 Though several works have been done in Ethiopia, social obligation18 and lack of discussion about the harmful effects of FGM are still barriers to its abonnement.11 Ethiopia stipulated a proclamation no. 414/2004 called the criminal code of the federal democratic republic of Ethiopia 2004 which makes FGM a criminal offense.19 This was a part of FGM prevention and to address which was not directly addressed by the 1995 constitution.20
Several studies were conducted to estimate the prevalence of FGM in Ethiopia.18,21–23 However, most of them were not nationwide studies in which different geographical areas were not considered. This study, therefore, aimed to assess the trend and determinants of female genital mutilation among women of reproductive age in Ethiopia using 2000, 2005, and 2016 EDHS. The findings of this study will be an input to clarify the actual situation at the national level and to identify factors associated with FGM at the individual and community level. Moreover, it will help to design interventional policies and strategies to reduce the problem and related complications.
Methods
Study Setting
The study was conducted in Ethiopia, the second-most populous nation in Africa next to Nigeria, with about 109 million people (2018) and with a 2.5% annual fertility rate.24,25 Ethiopia has nine regional states and two city administrations.26 Its economy depends mainly on agriculture.27
Data Source and Sample Size
The study was conducted among 15–49 years old women using data extracted from the 2000 (n=15,367), 2005 (n=14,070),28 and 2016 (n=7248).29 Ethiopian Demographic and Health Surveys (EDHS) datasets with their respective sample size. However, the EDHS 2011 dataset was excluded due to the absence of data on FGM.30 All the included surveys were conducted considering the nine regions and two administrative cities of the country. This study utilized the most recent 2016 EDHS to assess the individual- and community-level determinants of FGM among 15–49 years old women in Ethiopia. The data utilized in this study were obtained from the MEASURE DHS. http://www.dhs.program.com.
Sampling and Data Collection Methods
The sampling of all EDHS surveys considered all regions and administrative cites of the country. A two-stage sampling method was implemented to select the study participants. In the first stage, enumeration areas (EAs) were selected after stratifications of the region into urban and rural areas. In the second stage, households from each EAs were selected. The sample size in each stage was estimated through probability proportion to size. Based on this, a total of 539 EAs (138 Urban & 401 Rural) from EDHS 2000,31 540 EAs (145 Urban & 395 Rural) from EDHS 200528 and 645 EAs (202 urban and 443 rural) from EDHS 201629 were included. All women of reproductive age who were permanent inhabitants or stayed at least one night in the selected households were eligible for EDHS. Data were collected through face-to-face interviews.28,29,32
Data Collection Instrument and Period
All EDHS had three questionnaires, namely, the household’s questionnaire, women’s questionnaire, and men’s questionnaire. However, this study utilized EDHS 2000, EDHS 2005, and EDHS 2016 data collected through women’s questionnaire. The data collection tool was first prepared in English and then translated into the three main local languages – Amharic, Oromiffa, and Tigrigna languages. After intensive training for data collectors and supervisors, a pretest was conducted before the actual data collection.26,28,29 The 2000 EDHS, 2005 EDHS, and EDHS 2016 were conducted from February to May 2000,31 April to August 2005,28 and January to June 2016,29 respectively.
Variables of the Study
Outcome Variable
FGM was the outcome variable of this study. It was categorized and coded as 0 if a woman has not been circumcised and 1 if a woman has been circumcised. It was known from the response of the participants to the question “Have you been circumcised”.28,29,32
Independent Variables
The independent variables were grouped into individual- and community-level independent variables. Religion, educational level, age, occupation, age at first marriage, marital status, and wealth index were the individual-level factors, whereas place of residence, community media access, community poverty, community women educational level, and region were community-level variables (Figure 1). The variables were selected based on previous studies which revealed factors affecting the outcome variable.31,33–36 EDHS had a total of two community-level variables (residence and region). In this study, regions were recoded as large central (Tigray, Amhara, Oromia, and SNNPR), small peripheral regions (Gambela, Somalia, Benishangual, and Afar), and Metropolitans (Addis Ababa, Dire Dawa, and Harari), similar to previous studies.37,38 Additionally, individual-level variables were aggregated concerning their clusters (EAs) to create community-level variables. The aggregated variables were categorized into low or high based on the national median value of the proportions of participants in each characteristic. Community media exposure, community poverty level, and community educational level were community-level variables derived by aggregating individual-level variables.
 |
Figure 1 Conceptual framework showing factors associated with female genital mutilation. |
Data Processing and Analysis
The EDHS data utilized in this study were weighted to ensure its representativeness at the national and regional levels. Data analysis was conducted using STATA-14 software (STATA Corporation, College Station, TX, USA). Descriptive statistics (ie, frequency and percentage) were used to show the trends of FGM in Ethiopia. Similarly, both individual- and community-level factors affecting FGM were identified through multilevel logistic regression analysis.39 The association of each predictor and the outcome variable was checked with a 5% significance level and 95% CI. The presence of multicollinearity was checked among independent variables using the Variance Inflation Factor (VIF) at a cut-off point of 10. Variables with a VIF value of less than 10 indicate the absence of multicollinearity.
A total of four modelings were conducted to identify determinants of FGM. The first model was an empty model, which was conducted to estimate the random variability in the intercept. The second model was conducted to estimate the effect of individual-level factors on FGM. The third model assessed the effect of community-level factors on FGM. Finally, model four estimated the effect of both individual- and community-level factors on FGM. The Intra-Cluster Correlation (ICC) between clusters within each model was determined using the following formula.40,41
where ICC is the magnitude of variations explained by the clusters (community), VA is community variance and  is individual-level variance in standard logistic distribution = 3.29.40 Similarly,
is individual-level variance in standard logistic distribution = 3.29.40 Similarly,
Proportional Change in Variance (PCV) was calculated to determine the power of variables predicting FGM in each model. However, Akaike Information Criterion (AIC) was chosen to select the final model that explains the data best. The AIC value for each subsequent model was compared and the model with the lowest value was considered to be the best fit model.41–43
Moreover, variables with a p-value of less than 0.05 were considered as significant factors.
Ethics Approval and Consent to Participate
Ethical clearance was obtained from Ethiopia Health and Nutrition Research Institute Review.
Board for all EDHS, the Ministry of Science and Technology, the Institutional Review Board of ICF International, and the CDC. Data were collected after taking informed consent from all study participants and were kept confidential.28,29,31 This study was conducted after getting permission DHS Program. The datasets were used confidentially during processing and analysis.
Results
Characteristics of Participants
The mean age (± standard deviation (SD)) of participants in 2016 EDHS was 28.14 ± 9.16 years. More than three fourth (77.03%) of them were from rural areas. The majority (43.56%) of participants were Orthodox followed by Muslims (31.56%). There was a significant reduction of uneducated women from 75.17% in 2000 EDHS to 47% in 2016 EDHS. However, the percentage of participants married before the age of 18 years increased from 55.87% in 2000 EDHS to 62.05% in 2016 EDHS (Table 1).
 |
Table 1 Female Genital Mutilation by Background Characteristics in Ethiopia, Findings from 2000 to 2016 EDHS |
Prevalence of Female Genital Mutilation
The percentage of FGM was increased with age in all three surveys. It was increased from 70.72% among 15–19 years old to 86.79% among 45–49 years old in 2000 EDHS and from 64.22% among 15–19 years old to 83.68% among 45–49 years’ old in 2005 EDHS. Similarly, it was increased from 51.64% among 15–19 years old to 81.53% among 45–49 years old in 2016 EDHS. FGM among those who were working decreased from 79.57% in 2000 EDHS to 76.13% in 2005 EDHS then to 72.94% in 2016 EDHS. Similarly, FGM was decreased from 85.46% in 2000 EDHS to 58.11 in 2005 EDHS then to 50.74% in 2016 EDHS among participants who attended higher education. Moreover, it was decreased among participants in urban areas from 79.79% in 2000 EDHS to 72.53% in EDHS 2005 then to 55.49% in 2016 EDHS (Table 1).
Trends of Female Genital Mutilation in Ethiopia
The prevalence of FGM among women of reproductive age was 79.91% (95% CI: 79.27, 80.54), 74.26% (95% CI: 73.53, 74.98) and 70.37% (95% CI: 69.31, 71.43) in 2000 EDHS, 2005 EDHS and 2016 EDHS, respectively. Likewise, the prevalence of FGM among daughters of circumcised women was 56.16% (95% CI: 54.98, 57.33), 45.42% (95% CI: 44.18, 46.66) and 16.75% (95% CI: 15.73, 17.80) in 2000 EDHS, 2005 EDHS and 2016 EDHS, respectively. It was decreased by 39.41% from 2000 to 2016 among daughters of circumcised women (Figure 2).
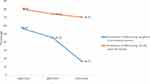 |
Figure 2 Trend of female genital mutilation in Ethiopia using 2000, 2005, and 2016 EDHS data. |
Factors Associated with Female Genital Mutilation
The most recent survey (2016 EDHS) data were utilized to identify individual- and community-level determinants of FGM. Based on the crude multilevel modeling, religion, educational level, age, occupation, age at first marriage, marital status, wealth index, residence, region, and mass media access were variable associated with FGM. However, religion, educational level, age, occupation, age at first marriage, marital status, residence, and region were variables significantly associated with FGM in the final multilevel logistic regression in which individual- and community-level variables were fitted simultaneously.
The odds of FGM were 5.48 times higher 5.48 (95% CI: 4.23, 7.09) among Muslims compared to Orthodox followers. Women who attended secondary and higher education were 43% less likely 0.57 (95% CI: 0.44, 0.74) and 60% less likely 0.40 (95% CI: 0.29,0.54) to be found circumcised, respectively. Participants aged 45–49 and 40–44 years were 5.06 times 5.06 (95% CI: 3.38, 7.57) and 4.11 times 4.11 (95% CI: 2.90, 5.85) more likely to be found circumcised, respectively, compared to women aged 15–19 years. Similarly, participants who were not working were 1.20 times 1.20 (95% CI: 1.02,1.41) more likely to be found circumcised (Table 2).
 |
Table 2 Findings of the Multilevel Logistic Regression to Identify the Factors Associated with Female Genital Mutilation in Ethiopia Using Data from 2016 EDHS |
Random Effect Results
The ICC value in the null model was (ICC = 0.598, P < 0.001). Based on ICC value, 60% of the variation on FGM is attributable to community-level factors. This higher ICC indicates multilevel modeling was better than single/individual-level analysis. However, ICC was reduced to 51% in the combined final model of regression. The highest value of PCV (30.5%) was also shown in the final model which indicates 30.5% of the variations on FGM is explained by individual- and community-level variables (Table 3).
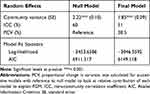 |
Table 3 Community-Level Variance Two Level Mixed Effects Logit Models Predicting Female Genital Mutilation, Ethiopia, 2016 |
Discussion
FGM is one of the major causes of reproductive health problems,44 particularly in low-income countries where medical care access is poor.45,46 This study aimed to assessed trends and determinants of FGM among 15–49 years old women using data from 2000, 2005, and 2016 EDHS.
According to this study, the prevalence of FGM was slightly decreased over time from 79.91% in 2000 to 70.37% in 2016. This was in line with a study in Burkina Faso which declined from 83.6% to 76.1% over 11 years.47 Moreover, the current study indicated a reduction of FGM by 39.1% among daughters of circumcised participants over the last 16 years. Though the risk of getting circumcised daughters is higher among daughters whose mothers are circumcised,44 the recent activities on increasing educational coverage48 might be the possible reason for its reduction. Similarly, the legal frameworks for the prevention of FGM might have a role in the reduction of FGM in Ethiopia.
This multilevel analysis identified different individual- and community-level determinants of FGM using EDHS 2016 data. Age, religion, educational level, occupation, age at first marriage, and marital status of participants were significant determinants of FGM at the individual level.
Likewise, region and residence were determinants of FGM at the community level.
In this study, the chance of women to be found mutilated was higher among Muslims compared to Orthodox Christians. The result was in line with previous studies conducted in Ethiopia,32 Burkina Faso,47,49 Somalia,50 Egypt,5 Cote d’Ivoire,51 and Senegal.35 Though FGM is not recommended by Islam,47 a study in Somali where 99% of the population is Sunni Muslim revealed that FGM was supported by 98% of Somali females.6 Similarly, a higher magnitude of FGM was shown in parts of Ethiopia where most of the populations were Muslims (ie, Somalia and afar regions).29 This might be due to Muslims might accept it is supported by the religion. According to previous studies, FGM was supported to attenuate women’s sexual desire which helps women to agree with the moral view of Islam52 and keep their virginity before marriage.22
In this study, education had a strong negative association with FGM. There was a reduction in the percentage of FGM with increasing women’s educational level. This finding was consistent with previous studies conducted in Somaliland,55 Nigeria,56,57 Egypt,58 Sudan,59 and Ghana.60 This could be due to the positive effect of education in changing the attitude of women towards FGM.48 Additionally, FGM was not a common practice among educated women,61 they usually oppose the practice.48 However, women who experienced FGM had lower school attendance and a higher dropout rate.62 Due to the above reasons, educating women is a known strategy to reduce FGM practice.63
Similar to studies conducted in Nigeria56 and Iraq,64 the current study identified that women who had not occupation were more likely to be found circumcised than those who had an occupation. This could be due to most women have an occupation when they are more educated. Their occupation helps them to decide independently on the practice.65 Similarly, their occupation might help them not to be poor. Another study revealed the magnitude of FGM was higher among the more poor women.59
According to this study, age was one of the determinants of FGM. An increase in women’s age was associated with higher odds of FGM. Similar findings were also identified in different studies conducted in Egypt,66 Ghana,60 and Nigeria.63,67 This could be due to the recent improved activities against FGM such as creating awareness on women’s sexual and reproductive health rights68 and strict laws against FGM practice.69 Moreover, the awareness of the effects of FGM could also be the reason for its lower odds among younger women than older.44
Marital status was also found to be determinants of FGM, in this study. Married women were higher likely to be found circumcised than divorced/widowed/ separated women. Studies done in Ghana60 and Finland10 showed a similar result. Surprisingly, in line with studies from Burkina Faso47 and Iraq,70 women who were married before their eighteenth birthday were more likely to be found circumcised than women married at age of 18 years or later. This might be due to the preference of their partners to get a circumcised wife50,71 There is a community belief that FGM is a means of keeping women from promiscuity72 and became a prerequisite for marriage in several sub-Saharan African countries including Ethiopia.73,74 For this reason, several women were forced to be found circumcised.75
In the current multilevel logistic regression, the geographical region was one of the determinants of FGM. Women from the metropolitans and peripheral regions were more likely to be found circumcised as compared to women from central regions. Similarly, women residing in rural areas were more likely to be found circumcised than urban residents. Similar results were revealed in different studies conducted in Burkina Faso,47,76 Somaliland,55 and Nigeria.77 This could be because of the better education coverage and better awareness creation activities towards the effects of FGM in urban areas. Likewise, it could be also due to better access to sexual and reproductive health services in urban areas.
Strength and Limitations of the Study
This study has limitations and strengths. First, the study used nationally representative DHS data collected from 2000 to 2016. This helps to provide better representative data as all regions and administrative cities in the country were included in all the surveys. Second, all three surveys used uniform and standardized survey instruments which allowed a better comparison of FGM across individual- and community-level variables across the consecutive surveys. However, it has limitations of cross-sectional studies. It does not show the fortitude cause and effect relationship between the variables.
Conclusions
Seven in ten reproductive-age women were found to be circumcised in Ethiopia. Similarly, around two of ten daughters of circumcised women were circumcised. Though FGM reduction from 2000 to 2016 among reproductive-aged women was unsatisfactory, it was significant among daughters of circumcised women. Age, religion, residence, region, age at first marriage, marital status, occupation, and educational level were determinants of FGM. Therefore, future interventions on FGM should target the metropolitan and peripheral regions. The interventions should also consider the roles of religious leaders, empowering, and educating women. Future experimental studies on the effectiveness of the intervention programs the country is considering to prevent FGM are recommended.
Abbreviations
AIC, Akaike Information Criterion; AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio; SD, standard deviation; FGM, female genital mutilation; SNNPR, Southern Nations Nationalities and Peoples region; DHS, Demographic and Health Survey; EDHS, Ethiopian Demographic and Health Survey; EAs, enumeration areas; ICC, intra-cluster variance; PCA, principal components analysis; PCV, proportional change in variance; SD, standard deviation; UNFPA, United Nations Population Fund; UNICEF, United Nations Children’s Fund; VIF, variance inflation factor; WHO, World Health Organization.
Data Sharing Statement
The data for this study are found on the DHS website http://www.dhsmeasures.
Acknowledgment
I acknowledge the DHS program for providing the data.
Author Contributions
The author made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Funding
There was no funding for this study.
Disclosure
The author declares that he has no competing interests.
References
1. WHO. An update on WHO’s work on Female Genital Mutilation (FGM). Progress Report. 2011
2. Mutilation FG Cutting: a global concern UNICEF. New York. 2016
3. UNICEF. New Statistical Report on Female Genital Mutilation Shows the Harmful Practice is a Global Concern. New York: UNICEF; 2016.
4. Organization WH. WHO Guidelines on the Management of Health Complications from Female Genital Mutilation. World Health Organization; 2016.
5. Alkhalaileh D, Hayford SR, Norris AH, Gallo MF. Prevalence and attitudes on female genital mutilation/cutting in Egypt since criminalisation in 2008. Cult Health Sex. 2018;20(2):173–182.
6. Fox KA, Johnson-Agbakwu C. Crime victimization, health, and female genital mutilation or cutting among Somali women and adolescent girls in the United States, 2017. Am J Public Health. 2020;110(1):112–118.
7. Mahmoud MIH. Effect of female genital mutilation on female sexual function, Alexandria, Egypt. Alexandria J Med. 2016;52(1):55–59.
8. Biglu M-H, Farnam A, Abotalebi P, Biglu S, Ghavami M. Effect of female genital mutilation/cutting on sexual functions. Sex Reprod Healthc. 2016;10:3–8.
9. Matanda DJ, Sripad P, Ndwiga C. Is there a relationship between female genital mutilation/cutting and fistula? A statistical analysis using cross-sectional data from demographic and health surveys in 10 Sub-Saharan Africa countries. BMJ Open. 2019;9(7):e025355.
10. Koukkula M, Keskimäki I, Koponen P, Mölsä M, Klemetti R. Female genital mutilation/cutting among women of Somali and Kurdish origin in Finland. Birth. 2016;43(3):240–246.
11. Varol N, Turkmani S, Black K, Hall J, Dawson A. The role of men in abandonment of female genital mutilation: a systematic review. BMC Public Health. 2015;15(1).
12. Antabe R, Sano Y, Anfaara FW, Kansanga M, Chai X, Luginaah I. Antenatal care utilization and female genital mutilation in Kenya. Sex Cult. 2019;23(3):705–717.
13. Mbanya VN, Gele AA, Diaz E, Kumar B. Health care-seeking patterns for female genital mutilation/cutting among young Somalis in Norway. BMC Public Health. 2018;18(1):517.
14. Kimani S, Kabiru CW, Muteshi J, Guyo J. Exploring barriers to seeking health care among Kenyan Somali women with female genital mutilation: a qualitative study. BMC Int Health Hum Rights. 2020;20(1):3.
15. Ogah J, Kolawole O, Awelimobor D. High risk human papillomavirus (HPV) common among a cohort of women with female genital mutilation. Afr Health Sci. 2019;19(4):2985–2992.
16. Malmström MF. UNFPA-UNICEF Joint Programme on Female Genital MutilationCutting: Accelerating Change: Annual Report 2010: Nurturing Change from Within. UNFPA-UNICEF; 2011.
17. Kidane G, Morrow RH. Teaching mothers to provide home treatment of malaria in Tigray, Ethiopia: a randomised trial. Lancet. 2000;356(9229):550–555.
18. Andarge MY The difficulties of ending Female Genital Mutilation (FGM): case of Afar Pastoralist Communities in Ethiopia; 2014. Available from: www.ohchrorg/Documents/Issues/Women/WRGS/FGM/NGOs/ActionFor.
19. Federal Democratic Republic of Ethiopia. The criminal code of the Federal Democratic Republic of Ethiopia, Proclamation No. 414/2004; 2005. Addis Ababa. Available from: http://www.ilo.org/dyn/natlex/docs/ELECTRONIC/70993/75092/F1429731028/ETH70993.pdf. Accessed May 9.
20. Constitution F. The Constitution of the Federal Democratic Republic of Ethiopia. Addis Ababa. 1995.
21. Degefa H, Samuel K, Taye L, Desalegn T. Prevalence of female genital mutilation and its association with birth complications among women attending delivery service in Nigist Eleni Mohammed General Hospital, Hossana, Southern Nations, Nationalities and Peoples’ Region, Ethiopia. Reprod Syst Sex. 2017;18–23.
22. Gajaa M, Wakgari N, Kebede Y, Derseh L. Prevalence and associated factors of circumcision among daughters of reproductive aged women in the Hababo Guduru District, Western Ethiopia: a cross-sectional study. BMC Womens Health. 2016;16(1):42.
23. Oljira T, Assefa N, Dessie Y. Female genital mutilation among mothers and daughters in Harar, eastern Ethiopia. Int J Gynecol Obstet. 2016;135(3):304–309.
24. Hailemariam A. The second biggest African country undergoing rapid change: Ethiopia. In: Groth H, May J, editors. Africa’s Population: In Search of a Demographic Dividend. Cham: Springer; 2017:53– 69. doi:10.1007/978-3-319-46889-1_4.
25. The World Bank In Ethiopia. The World Bank in Ethiopia [Internet]; 2019. Available from: https://www.worldbank.org/en/country/ethiopia/overview#1.
26. Kaewkiattikun K. Effects of immediate postpartum contraceptive counseling on long-acting reversible contraceptive use in adolescents. Adolesc Health Med Ther. 2017;8:115–123.
27. Dulitha F, Nalika G, Upul S, Chrishantha WM, De Alwis SR, Hemantha S. Risk factors for teenage pregnancies in Sri Lanka: perspective of a community based study. HealTH Sci J. 2013;7(3):269.
28. [Ethiopia] CSA, Macro ORC. Ethiopia Demographic and Health Survey 2005. Addis Ababa, Ethiopia and Calverton: Central Statistical Agency and ORC Macro Maryland, USA; 2006.
29. ICF C. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2016.
30. CSA-Ethiopia ICF. International: Ethiopia Demographic and Health Survey 2011. Addis Ababa, Ethiop Calverton, Maryland, USA: Cent Stat Agency Ethiop ICF Int; 2012.
31. Authority CS. Ethiopia Demographic and Health Survey 2000. Cent Stat Authority, Addis Ababa. 2001
32. Setegn T, Yihunie Lakew KD. Geographic variation and factors associated with female genital mutilation among reproductive age women in Ethiopia: a national population based survey. PLoS One. 2016;11(1).
33. Yirga WS, Kassa NA, Gebremichael MW, Aro AR. Female genital mutilation: prevalence, perceptions and effect on women’s health in Kersa district of Ethiopia. Int J Womens Health. 2012;4:45.
34. Njue C, Karumbi J, Esho T, Varol N, Dawson A. Preventing female genital mutilation in high income countries: a systematic review of the evidence. Reprod Health. 2019;16(1):113.
35. Kandala N-B, Shell-Duncan B. Trends in female genital mutilation/cutting in Senegal: what can we learn from successive household surveys in sub-Saharan African countries? Int J Equity Health. 2019;18(1):25.
36. Van Rossem R, Meekers D, Gage AJ. Women’s position and attitudes towards female genital mutilation in Egypt: a secondary analysis of the Egypt demographic and health surveys, 1995–2014. BMC Public Health. 2015;15(1):874.
37. Abrha S, Shiferaw S, Ahmed KY. Overweight and obesity and its socio-demographic correlates among urban Ethiopian women: evidence from the 2011 EDHS. BMC Public Health. 2016;16(1):636.
38. Ahmed KY, Page A, Arora A, Ogbo FA. Trends and determinants of early initiation of breastfeeding and exclusive breastfeeding in Ethiopia from 2000 to 2016. Int Breastfeed J. 2019;14(1):40.
39. Hox JJ, Moerbeek M, Van de Schoot R. Multilevel Analysis: Techniques and Applications. Routledge: Lawrence Erlbaum Associates Publishers; 2010.
40. Darmawan I, Keeves JP Suppressor variables and multilevel mixture modelling. 2006
41. Goldstein H. Multilevel Statistical Models. Vol. 922. John Wiley & Sons; 2011.
42. Schwarz G. Estimating the dimension of a model. Ann Stat. 1978;6(2):461–464.
43. Akaike H. A new look at the statistical model identification. IEEE Trans Automat Contr. 1974;19(6):716–723.
44. Yasin BA, Al-Tawil NG, Shabila NP, Al-Hadithi TS. Female genital mutilation among Iraqi Kurdish women: a cross-sectional study from Erbil city. BMC Public Health. 2013;13(1):809.
45. Clayton-Hathway K A Pilot Evaluation of Health Services for Communities Affected by FGM in Oxfordshire. 2016
46. Dixon S, Shacklock J, Leach J. Tackling female genital mutilation in the UK: female genital mutilation: barriers to accessing care. BMJ. 2019;364.
47. Chikhungu LC, Madise NJ. Trends and protective factors of female genital mutilation in Burkina Faso: 1999 to 2010. Int J Equity Health. 2015;14(1):42.
48. Van Rossem R, Meekers D, Gage AJ. Trends in attitudes towards female genital mutilation among ever-married Egyptian women, evidence from the Demographic and Health Surveys, 1995–2014: paths of change. Int J Equity Health. 2016;15(1):31.
49. Inungu J, Tou Y. Factors associated with female genital mutilation in Burkina Faso. J Publ Health Epidemiol. 2013;5(11):20–28.
50. Gele AA, Bø BP, Sundby J. Have we made progress in Somalia after 30 years of interventions? Attitudes toward female circumcision among people in the Hargeisa district. BMC Res Notes. 2013;6(1):122.
51. Plo K, Asse K, Seï D, Yenan J. Female genital mutilation in infants and young girls: report of sixty cases observed at the general hospital of abobo (abidjan, cote d’ivoire, west Africa). Int J Pediatr. 2014;2014.
52. Arafa A, Mostafa A, Eshak ES. Prevalence and risk factors of female genital mutilation in Egypt: a systematic review. Clin Epidemiol Glob Health. 2020.
53. Perron L, Senikas V, Burnett M, et al. Female genital cutting. J Obstet Gynaecol Can. 2013;35(11):1028–1045.
54. Sagna ML. Gender differences in support for the discontinuation of female genital cutting in Sierra Leone. Cult Health Sex. 2014;16(6):603–619.
55. Newell-Jones K. Empowering communities to collectively abandon FGM/C in Somaliland. Action Aid. 2016.
56. Ashimi AO, Amole TG, Iliyasu Z. Prevalence and predictors of female genital mutilation among infants in a semi urban community in northern Nigeria. Sex Reprod Healthc. 2015;6(4):243–248.
57. Ossai EN, Aniwada EC, Nwobi EA, Ezeoke UE. Prevalence and predictors of female genital cutting in Nigeria: an analysis of 2013 Nigeria Demographic and Health Survey. J Community Med Health Care. 2018;3(1):1026.
58. Modrek S, Liu JX. Exploration of pathways related to the decline in female circumcision in Egypt. BMC Public Health. 2013;13(1):921.
59. Elduma AH. Female genital mutilation in Sudan. Open Access Maced J Med Sci. 2018;6(2):430.
60. Sakeah E, Debpuur C, Oduro AR, et al. Prevalence and factors associated with female genital mutilation among women of reproductive age in the Bawku municipality and Pusiga District of northern Ghana. BMC Womens Health. 2018;18(1):150.
61. Arafa AE, Elbahrawe RS, Shawky SM, Abbas AM. Epidemiological and gynecological correlates with female genital mutilation among Beni-Suef University students; cross sectional study. Middle East Fertil Soc J. 2018;23(3):184–188.
62. Chai X, Sano Y, Kansanga M, Baada J, Antabe R. Married women’s negotiation for safer sexual intercourse in Kenya: does experience of female genital mutilation matter? Sex Reprod Healthc. 2017;14:79–84.
63. Adewole AJ, Adayonfo EO. Correlates of female genital mutilation (FGM) among patients of a teaching hospital in Nigeria. IFE Psychol Int J. 2017;25(1):223–231.
64. Shabila NP. Mothers’ factors associated with female genital mutilation in daughters in the Iraqi Kurdistan region. Women Health. 2017;57(3):283–294.
65. Afifi M Women’s empowerment and the intention to continue the practice of female genital cutting in Egypt. 2009
66. Mohammed ES, Seedhom AE, Mahfouz EM. Female genital mutilation: current awareness, believes and future intention in rural Egypt. Reprod Health. 2018;15(1):175.
67. Bogale D, Markos D, Kaso M. Prevalence of female genital mutilation and its effect on women’s health in Bale zone, Ethiopia: a cross-sectional study. BMC Public Health. 2014;14(1):1076.
68. Grose RG, Hayford SR, Cheong YF, Garver S, Kandala N-B, Yount KM. Community influences on female genital mutilation/cutting in Kenya: norms, opportunities, and ethnic diversity. J Health Soc Behav. 2019;60(1):84–100.
69. Kandala N-B, Komba PN. Geographic variation of female genital mutilation and legal enforcement in sub-saharan Africa: a case study of Senegal. Am J Trop Med Hyg. 2015;92(4):838–847.
70. Saleem RA, Othman N, Fattah FH, Hazim L, Adnan B. Female Genital Mutilation in Iraqi Kurdistan: description and associated factors. Women Health. 2013;53(6):537–551.
71. Sakeah E, Doctor HV, Beke A, Hodgson AB. Males\’Preference for circumcised women in Northern Ghana. Afr J Reprod Health. 2006;10(2):37–47.
72. Waigwa S, Doos L, Bradbury-Jones C, Taylor J. Effectiveness of health education as an intervention designed to prevent female genital mutilation/cutting (FGM/C): a systematic review. Reprod Health. 2018;15(1):62.
73. Althaus FA. Female circumcision: rite of passage or violation of rights? Int Fam Plan Perspect. 1997;130–133.
74. Martinelli M, Ollé-Goig JE. Female genital mutilation in Djibouti. Afr Health Sci. 2012;12(4):412–415.
75. Pande R, Malhotra A, Grown C Impact of investments in female education on gender equality. In:
76. Karmaker B, Kandala N-B, Chung D, Clarke A. Factors associated with female genital mutilation in Burkina Faso and its policy implications. Int J Equity Health. 2011;10(1):20.
77. Adeyinka A, Adedotun O, Asabi O. Knowledge and practice of female circumcision among women of reproductive ages in South West Nigeria. J Humanit Soc Sci. 2012;2(3):38–45.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.