Back to Journals » Neuropsychiatric Disease and Treatment » Volume 16
Treatment-Seeking Behavior Towards Epilepsy Among Rural Residents in Ethiopia: A Cross-Sectional Study
Authors Molla A , Mekuriaw B , Habtamu E, Mareg M
Received 29 November 2019
Accepted for publication 25 January 2020
Published 13 February 2020 Volume 2020:16 Pages 433—439
DOI https://doi.org/10.2147/NDT.S240542
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Roger Pinder
Alemayehu Molla,1 Birhanie Mekuriaw,1 Endashaw Habtamu,1 Moges Mareg2
1Department of Psychiatry, College of Medicine and Health Science, Dilla University, Dilla, Ethiopia; 2Departments of Reproductive Health, College of Medicine and Medical Sciences, Dilla University, Dilla, Ethiopia
Correspondence: Alemayehu Molla
Department of Psychiatry, College of Medicine and Health Science, Dilla University, Dilla, Ethiopia
Tel +25192073609
Email [email protected]
Background: Even though a large number of patients live with epilepsy, few of them receive effective treatment. Most people with epilepsy, particularly those from rural communities, do not seek medical care as they are convinced that solutions lie only with traditional healers (traditional leaders, prophets and community elders). Therefore, studying treatment-seeking behavior regarding this major neurological problem would provide additional knowledge and help to identify a gap which needs to be addressed when tackling related problems.
Participants and Methods: This rural community-based cross-sectional study was conducted in Gedeo zone, Ethiopia, among 755 participants. Data were collected using face-to-face interview-based questionnaires. Collected data were entered into EpiData version 3.01 and analyzed using SPSS version 20. Bivariate and multivariate logistic regression analysis was conducted to identify associated factors. The strengths of associations were presented as adjusted odds ratios with 95% confidence intervals.
Results: The prevalence of poor treatment-seeking behavior was 54.6% (95% CI 51.4, 58.2). Poor knowledge (adjusted odds ratio [AOR]=3.21, 95% CI 2.14, 4.81), poor social support (AOR=2.48, 95% CI 1.12, 5.53), unfavorable attitude (AOR=1.84, 95% CI 1.34, 2.54) and having no history of experiencing others’ seizures (AOR=2.17, 95% CI 1.47, 3.2) were variables strongly associated with poor help-seeking behavior towards epilepsy.
Conclusion: The study showed that more than half of the participants had poor treatment-seeking behavior towards epilepsy. This indicates the need to implement measures to raise community awareness regarding treatment options for epilepsy.
Keywords: epilepsy, Ethiopia, rural residents, treatment-seeking behavior
Introduction
Epilepsy is a common chronic non-communicable disease of the brain that affects people of all age groups. It carries neurological, cognitive, psychological and social consequences, and globally more than 65 million peoples are affected by epilepsy.1–3 Developing countries carry 90% of the financial burden of epilepsy and 85% of the world’s people with epilepsy live in developing countries with little or no access to medical treatment.3
Despite the availability of effective and low-cost anti-seizure medicines, more than 80% of people with epilepsy in low-income countries do not have access to treatment.2,4 Evidence also shows that up to 70% of people with epilepsy could become seizure free with the appropriate use of anti-seizure medicines.4,5
In Ethiopia about 81% of people with epilepsy and their relatives suffer from perceived epilepsy stigma, which has a direct influence on treatment options.6,7 For centuries, religious and cultural taboos have influenced the type of care and treatment available for people with epilepsy.8 In many African communities the myths regarding epilepsy continue to be a cause of wide treatment gaps. Sociocultural attitudes continue to have a negative impact on the management of epilepsy in many African nations.9 Wrong attitudes and beliefs about epilepsy create serious negative social and psychological consequences for people with epilepsy, such as fear, humiliation and limitations in social interactions.10 As a result, people with epilepsy are burdened by social, psychological and economic consequences, which lead to poor quality of life.11,12
Considering this, it is important to know more about treatment perceptions towards epilepsy which can help to improve people's treatment-seeking behavior, to reduce the psychosocial and economic impacts related to disease among community residents.10,13 Therefore, this study was conducted to assess treatment-seeking behavior towards epilepsy among rural residents in southern Ethiopia.
Participants and Methods
This rural community-based cross-sectional study was conducted in Gedeo zone in southern Ethiopia from 1 to 30 March 2019. Gedeo zone is located 365 km from Addis Ababa, the capital city of Ethiopia. All adults aged ≥18 years and who were available during the data-gathering period were invited as study participants. Individuals who were ill and unable to communicate during the data-collection time were excluded.
Sample size was calculated using a single population proportion formula, considering the following assumptions: proportion of residents having poor practice of seeking modern treatment 66.5%,9 margin of error 0.05, 95% confidence interval (CI) and design effect 2. After adding a 10% non-response rate, the final calculated sample size was 755. To select samples, a multistage sampling technique was used. First, out of six rural districts in Gedeo zone, three districts were selected at random. In the second step, nine subdistricts (three in each district) were taken, again at random. The list of households in each of the area was obtained from the district offices and health extension workers. The calculated sample size was allocated proportionally in the selected subdistricts based on the number of households belonging to the subdistricts. Finally, participants were interviewed in the household; in the case of more than one participant in the household being eligible, we selected one individual by a lottery method.
Data were collected using a structured and interview-administered questionnaire. The content of the questionnaire included sociodemographic variables, Stigma Scale of Epilepsy, knowledge- and attitude-related variables, help-seeking behavior questionnaires, Oslo Social Support Scale and Substance-Related Questionnaire. Knowledge and attitude were assessed using the Kilifi Epilepsy Beliefs and Attitude Scale.14 Epilepsy stigma was assessed using the 24-item Stigma Scale of Epilepsy, which is validated for use in resource-limited countries.15 Help-seeking behavior was assessed by WHO General Health-Seeking behavior questionnaires and participants who scored greater than or equal to the mean score were considered as having good help-seeking behavior.16 The Alcohol, Smoking and Substance Involvement Screening Test (WHO ASSIST version 3.0), which is a commonly used and culturally validated tool, was used to assess lifetime and current substance use.17 Social support was collected by the 3-item Oslo Social Support Scale; this culturally validated tool has a sum score ranging from 3 to 14 in three categories: poor support 3–8, moderate support 9–11 and strong support 12–14.18
We used nine trained diploma nurses as data collectors and three Bachelor of Science (BSc) psychiatric nurses as supervisors. The questionnaire was translated from the English version to the local language and back to the English language to check its consistency. The data collectors were supervised daily and the completed questionnaires were checked daily by the supervisors and investigators for completeness. Data were entered into the computer using EpiData version 3.1 and exported to SPSS version 20 for analysis. Descriptive data were summarized using tables. Binary logistic regression was used to identify factors associated with the outcome variable. Variables with a P-value of <0.2 in bivariate regression were included in multivariable logistic regression. Finally, a P-value ≤0.05 in multivariate logistic regression was considered statistically significant and the strength of associations was determined using the adjusted odds ratio (AOR) and 95% CI.
Results
Sociodemographic Distribution of Respondents
A total of 732 participants were included in this study, with a response rate of 97%. The mean±SD age of the respondents was 33±11.3 years. Among the participants, the majority [316 (43.2%)] were in the age range 18–28 years and 467 (63.8%) were male. Of the total participants, a large proportion [513 (70.1%)] were Protestant in their religion and 632 (86.3%) were from a Gedeo ethnic background. The majority of participants [513 (70.1%)] were married. The educational status of participants showed that 276 (37.7%) had been educated at primary level. Regarding occupation, 232 (31.7%) of participants reported that they were farmers. Almost all respondents [718 (98.1%)] could access health centers at a distance of <10 km. The majority of respondents had monthly income of less than $1.9 [538 (73.5%)] (Table 1).
 |
Table 1 Frequency Distribution of Participants by Sociodemographic Factors in Rural Gedeo Zone, Ethiopia, 2019 (n=732) |
Psychosocial and Substance-Related Factors of Respondents
Regarding the psychosocial characteristics of the respondents, 347 participants (47.4%) reported stigma with respect to epilepsy and 451 (61.6%) reported poor social support. Of the participants, 173 (23.6%) reported current alcohol use, 40 (5.5%) that they chew khat and 39 (5.3%) that they currently smoke cigarettes (within 3 months of the study) (Table 2).
 |
Table 2 Distribution of Psychosocial and Substance-Related Factors Among Rural Residents in Gedeo Zone, 2019 (n=732) |
Clinical and Related Factors
Although 54 respondents (7.4%) reported a previous history of epilepsy, only 12 (1.6%) of them had obtained help for their problem. Among participants who received help for their epilepsy, seven (58.33%) obtained help from religious centers and three (25%) from traditional healers. Only two respondents (16.66%) accessed help from health centers. Among the respondents who did not seek help for epilepsy, most [31 (73.8%)] reported that epilepsy has no modern treatment. Furthermore, 27% and 51.6% of participants had poor knowledge and an unfavorable attitude, respectively. About 21% of study participants had a history of witnessing seizures. Regarding family history, 61 respondents (8.3%) and 76 (10.4%) reported a family history of epilepsy and mental illness, respectively. Furthermore, 58 participants (7.9%) reported a history of head injury (Table 3).
 |
Table 3 Descriptions of Clinical-Related Factors Among Rural Residents in Gedeo Zone, 2019 (n=732) |
Factors Related to Treatment-Seeking Behavior Towards Epilepsy
More than half of the particpants [400 (54.6%)] scored below the mean score, which is an indicator of poor help-seeking behavior towards epilepsy according to the WHO general help-seeking questionnaire. Regarding the place in which they sought treatment, most respondents [416 (56.8%)] preferred religious centers for epilepsy treatment, and 305 participants (41.7%) reported that they did not prefer health centers as a treatment option for epilepsy. Among community participants, 147 (20.1%) reported they would not seek any treatment options for epilepsy (Table 4).
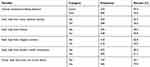 |
Table 4 Treatment Seeking-Related Factors Towards Epilepsy Among Rural Residents in Gedeo Zone, 2019 (n=732) |
Factors Associated with Treatment-Seeking Behavior Towards Epilepsy
In multivariable binary logistic regression, the variables unfavorable attitude, poor knowledge, poor social support and having no history of experiencing others' seizures were statistically significantly correlated with poor help-seeking behavior towards epilepsy (p<0.05).
Participants with poor knowledge were 3.21 times more likely to have poor help-seeking behavior than those with higher knowledge levels (AOR=3.21, 95% CI 2.14, 4.81).
The factor of having no history of experiencing others' seizures was strongly associated with lack of help-seeking behavior in this study. The odds of having poor help-seeking behavior among participants who had no history of experiencing others' seizures were 2.17 times higher than in those with such a history (AOR=2.17, 95% CI 1.47, 3.2).
The odds of having poor help-seeking behavior among respondents with a history of an unfavorable attitude were 1.84 times higher than in those without this attitude (AOR=1.84, 95% CI 1.34, 2.54).
The other factor that was strongly associated with poor help-seeking behavior was poor social support. The odds of having poor help-seeking behavior among participants with poor social support were 2.48 times higher than among participants with good social support (AOR=2.48, 95% CI 1.12, 5.53) (Table 5).
 |
Table 5 Bivariate and Multivariate Logistic Regression Analysis of Factors Associated with Poor Help-Seeking Behavior Among Rural Residents in Gedeo Zone, Ethiopia, 2019 (n=732) |
Discussion
Epilepsy is a major health problem in Ethiopia.19 This study aimed to assess treatment-seeking behavior towards epilepsy and associated factors among residents of rural communities in southern Ethiopia.
The study showed that 54.6% of respondents had poor treatment-seeking behavior. This proportion is similar to that found in a study conducted in Jimma University, Ethiopia (53.3%),20 but lower than in another study conducted in Ethiopia in which 66.5% had poor practice of seeking treatment for epilepsy.9 It is also lower than in a study conducted in low-income countries in which about 80% of respondents did not seek any treatment.21 In the current study, 41.7% of participants did not seek help from modern health institutions; this result is supported by a study conducted from Nigeria in which 55.8% of participants did not take epileptic patients to a hospital during a seizure.22 This may be a result of cultural influences regarding the causes of and treatment options for seizure, as people in many developing countries believe that epilepsy cannot be cured by modern treatment, but rather by traditional treatments. Another possible reason may be due to stigma, as many people consider that having an epileptic patient is stigmatizing to the community, so they are afraid to take the patient to a public place such as a hospital.23 Another possible explanation is the difference in the tools used; the study conducted in Nigeria used an author-developed tool, whereas in this study we tried to use tools that have been approved by the WHO to assess help-seeking behavior.
Regarding factors, poor knowledge, having no history of experiencing epileptic seizures, unfavorable attitude and poor social support were strongly associated with poor help-seeking behavior towards epilepsy. This finding is supported by studies conducted in Sudan,24 Ethiopia9 and Asia.25 These factors may be due to social isolation and poor social adaptation resulting from perceived stigma, which can make it difficult for people to seek treatment for their illness; however, good social support is vital for good health in reducing the risk of having epilepsy.26 Participants with poor social support may not receive information regarding the treatment options for epilepsy. Another possible reason is that participants with a history of having experienced others' seizures may have had to see different treatment options owing to the frequent impact of seizures on the physical and emotional health of those patients. Most studies also showed that attitude had a direct relationship with treatment-seeking behavior towards epilepsy, particularly in rural communities, and sociocultural attitudes continue to have a negative impact on the management of epilepsy in Ethiopia.9 Limitations of this study are that some ideal factors that might have been addressed by a qualitative study were not included, and the nature of the study design could not establish a temporal relationship between the outcome and the independent variables.
Conclusion
The current study showed that participants had poor treatment-seeking behavior. Factors such as poor social support, having no history of experiencing others' seizures, unfavorable attitude and poor knowledge were associated with poor treatment-seeking behavior. Community awareness regarding treatments for epilepsy needs be raised.
Compliance with Ethical Standards
All procedures undertaken during data collection were in accordance with the ethical review board of Dilla University and the Helsinki Declaration. The study was approved by the ethical review board of Dilla University. The participants were informed about the aim of the study and any identification or names were not recorded to maintain confidentiality. The right was also given to the study participants to refuse or discontinue participation at any time during the interview. Finally, data were collected after obtaining written informed consent from the participants.
Acknowledgments
We acknowledge Dilla University College of Medicine and Health Sciences for technical support and study participants for their willingness to participate in this study. We also acknowledge Gedeo Zone Health Bureau Administrative Office.
Author Contributions
All authors contributed towards data analysis, drafting and revising the manuscript, gave final approval of the paper to be published, and agreed to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Devinsky O, Spruill T, Thurman D, Friedman D. Recognizing and preventing epilepsy-related mortality: a call for action. Neurology. 2016;86(8):779–786. doi:10.1212/WNL.0000000000002253
2. World Health Organization. Epilepsy: A Public Health Imperative: Summary. World Health Organization; 2019.
3. Ngugi AK, Bottomley C, Kleinschmidt I, Sander JW, Newton CR. Estimation of the burden of active and life‐time epilepsy: a meta‐analytic approach. Epilepsia. 2010;51(5):883–890. doi:10.1111/j.1528-1167.2009.02481.x
4. Meyer A-C, Dua T, Ma J, Saxena S, Birbeck G. Global disparities in the epilepsy treatment gap: a systematic review. Bull World Health Organ. 2010;88:260–266. doi:10.2471/BLT.09.064147
5. Brodie M, Barry S, Bamagous G, Norrie J, Kwan P. Patterns of treatment response in newly diagnosed epilepsy. Neurology. 2012;78(20):1548–1554. doi:10.1212/WNL.0b013e3182563b19
6. Pal SK, Sharma K, Prabhakar S, Pathak A. Psychosocial, demographic, and treatment-seeking strategic behavior, including faith healing practices, among patients with epilepsy in northwest India. Epilepsy Behav. 2008;13(2):323–332. doi:10.1016/j.yebeh.2007.12.023
7. Shibre T, Alem A, Tekle-Haimanot R, Medhin G. Perception of stigma in people with epilepsy and their relatives in Butajira, Ethiopia. Ethiop J Health Dev. 2006;20(3).
8. Stigma Obeid T. An aspect of epilepsy not to be ignored. Saudi Med J. 2008;29(4):489–497.
9. Teferi J, Shewangizaw Z. Assessment of knowledge, attitude, and practice related to epilepsy: a community-based study. Neuropsychiatr Dis Treat. 2015;11:1239.
10. Lua PL, Neni WS. Awareness, knowledge, and attitudes with respect to epilepsy: an investigation in relation to health-related quality of life within a Malaysian setting. Epilepsy Behav. 2011;21(3):248–254. doi:10.1016/j.yebeh.2011.03.039
11. Keezer MR, Sisodiya SM, Sander JW. Comorbidities of epilepsy: current concepts and future perspectives. Lancet Neurol. 2016;15(1):106–115. doi:10.1016/S1474-4422(15)00225-2
12. De Boer HM, Mula M, Sander JW. The global burden and stigma of epilepsy. Epilepsy Behav. 2008;12(4):540–546. doi:10.1016/j.yebeh.2007.12.019
13. Beghi E, Berg A, Carpio A, et al. Comment on epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia. 2005;46(10):1698–1699. doi:10.1111/epi.2005.46.issue-10
14. Mbuba CK, Abubakar A, Hartley S, Odermatt P, Newton CR, Carter JA. Development and validation of the kilifi epilepsy beliefs and attitude scale. Epilepsy Behav. 2012;24(4):480–487. doi:10.1016/j.yebeh.2012.06.001
15. Fernandes PT, Salgado PC, Noronha AL, Sander JW, Li LM. Stigma scale of epilepsy: validation process. Arq Neuropsiquiatr. 2007;65:35–42. doi:10.1590/S0004-282X2007001000006
16. Wilson CJ, Deane FP, Ciarrochi JV, Rickwood D Measuring help seeking intentions: properties of the general help seeking questionnaire; 2005.
17. Henry-Edwards S, Humeniuk R, Ali R, Poznyak V, Monteiro M. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Guidelines for Use in Primary Care (Draft Version 1.1 For Field Testing). Geneva: World Health Organization; 2003.
18. Dalgard OS, Dowrick C, Lehtinen V, et al. Negative life events, social support and gender difference in depression. Soc Psychiatry Psychiatr Epidemiol. 2006;41(6):444–451. doi:10.1007/s00127-006-0051-5
19. Gedefa M, Wolde T, Solomon G. Knowledge, attitudes and practices with respect to epilepsy among preparatory school students in Mekelle city, Ethiopia. Int J Collab Res Intern Med Public Health. 2012;4(3):202.
20. Kassie GM, Kebede TM, Duguma BK. Knowledge, attitude, and practice of epileptic patients towards their illness and treatment in Jimma University specialized hospital, Southwest Ethiopia. N Am J Med Sci. 2014;6(8):383. doi:10.4103/1947-2714.139288
21. Tsigebrhan R, Hanlon C, Medhin G, Fekadu A. Help seeking and suicidality among people with epilepsy in a rural low income country setting: cross-sectional survey. Int J Ment Health Syst. 2017;11(1):44. doi:10.1186/s13033-017-0151-5
22. Jack-Ide IO, Maliki AE, Onasoga O. Community members’ perception of epilepsy and their attitude towards persons living with epilepsy disorders in a rural community of Bayelsa State, Nigeria. Int Neuropsychiatr Dis J. 161–167.
23. Baskind R, Birbeck GL. Epilepsy-associated stigma in sub-Saharan Africa: the social landscape of a disease. Epilepsy Behav. 2005;7(1):68–73. doi:10.1016/j.yebeh.2005.04.009
24. Babikar HE, Abbas IM. Knowledge, practice and attitude toward epilepsy among primary and secondary school teachers in South Gezira locality, Gezira State, Sudan. J Family Community Med. 2011;18(1):17. doi:10.4103/1319-1683.78633
25. Lim KS, Lim CH, Tan CT. Attitudes toward epilepsy, a systematic review. Neurol Asia. 2011;16:4.
26. Hills MD. The psychological and social impact of epilepsy. Neurol Asia. 2007;12(1):10–12.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
