Back to Journals » Patient Preference and Adherence » Volume 10
Treatment satisfaction of patients undergoing ranibizumab therapy for neovascular age-related macular degeneration in a real-life setting
Authors Gohil R, Crosby-Nwaobi R, Forbes A, Burton B, Hykin P, Sivaprasad S
Received 1 February 2016
Accepted for publication 29 February 2016
Published 26 May 2016 Volume 2016:10 Pages 949—955
DOI https://doi.org/10.2147/PPA.S105536
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Rishma Gohil,1,2 Roxanne Crosby-Nwaobi,1,2 Angus Forbes,2 Ben J Burton,3 Philip Hykin,1 Sobha Sivaprasad1,4
1National Institute for Health Research Moorfields Biomedical Research Centre, London, 2Diabetes Nursing, King’s College London, London, 3Ophthalmology Department, James Paget University Hospital, Great Yarmouth, 4Laser and Retinal Research Unit, King’s College Hospital, London, UK
Context: Treatment satisfaction with a loading phase of monthly injections for 3 months followed by a pro-re-nata regimen of ranibizumab in neovascular age-related macular degeneration (nAMD) remains unclear.
Aims: The aim was to evaluate the treatment satisfaction of persons with nAMD treated with ranibizumab in a real-life setting.
Settings and design: A cross-sectional study was conducted across three eye clinics within the National Health Service in the UK, where treatment is provided free at point of contact.
Materials and methods: A total of 250 patients were selected randomly for the study. Treatment satisfaction was assessed using the Macular Treatment Satisfaction Questionnaire. Data were collected on satisfaction of the service provided (Client Service Questionnaire-8) and the patients’ demographic and quality of life and treatment history. Factors governing treatment questionnaire were determined.
Results: The most important factors that determined the satisfaction were the service provided at the clinic (Client Service Questionnaire-8), health-related quality of life (EQ-5D-3L), and duration of AMD. Visual acuity changes were rated as less important than one would have expected.
Conclusion: The study result suggested that treatment satisfaction for nAMD was governed by the perception of being reviewed and injected regularly over a long period of time than the actual change in visual acuity from the treatment.
Keyword: macular treatment satisfaction questionnaire, patient related outcome measure, treatment history, quality of life
A Letter to the Editor has been received and published for this article.
Introduction
Advanced age-related macular degeneration (AMD) is one of the most common causes of visual impairment in the older population.1 If left untreated, the neovascular form of advanced AMD (nAMD) results in central retinal scaring and atrophy, resulting in severe visual loss. Visual loss in the elderly is associated with functional decline, an increased utilization of social and community support services, increased risk of falls and depression.2–5
In the last decade, there have been significant advances in the treatment of nAMD. Clinical trials on repeated intravitreal injections of inhibitors of vascular endothelial growth factor (VEGF) in nAMD show that ~30% of individuals show improved visual outcomes and 95% show stabilization of vision.6–8 However, the therapy can be demanding, as patients require frequent hospital attendance for their injections. The therapy burden on patients and caregivers may moderate the real-life outcomes observed outside of the clinical trial9,10 and factors such as patient satisfaction with their care may impact on treatment success.
Patient reported outcome measures (PROMs) are increasingly being used to evaluate patient experience in various disease management areas. These outcomes measure the impact of a treatment on the quality of life of patients. In addition to these measures, there has been a recent emphasis on assessing the views of patients on the care they receive within the clinical service they attend for their treatment. Therefore, there has been a surge in the use of both PROMs and patient-reported experience measures11 to better qualify the overall satisfaction with a service and treatment.6 Patient satisfaction of anti-VEGF therapy for nAMD has not been evaluated in a real-life setting to date.
The only available disease-specific instrument for measuring treatment satisfaction is the Macular Disease Treatment Satisfaction Questionnaire (MacTSQ) and it has been used in the Inhibit VEGF in Age-related choroidal Neovascularisation (IVAN) trial that investigated the comparative effectiveness of two anti-VEGF agents and different treatment regimens for nAMD.6,12,13
Ranibizumab is the first intravitreal anti-VEGF licensed for nAMD. Currently, the recommended approach for ranibizumab in the National Health Service (NHS) is monthly monitoring appointments until stability is reached, followed by pro-re-nata dosing based on visual acuity and morphological outcomes.
The aims of this study were to assess the treatment satisfaction of patients on ranibizumab therapy for nAMD using MacTSQ and evaluate the factors, including PROMs, that influence the treatment satisfaction score. This was assessed in the context of a caregiver burden study for patients on ranibizumab therapy for nAMD.
Ethics
The study was approved by the National Research Ethics Service Committee (13/WA/0032) and conducted according to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all the participants prior to completion of the non-incentivized questionnaire.
Methods
Study design and patients
This cross-sectional questionnaire-based survey was conducted on 250 patient–caregiver pairs from three public ophthalmic treatment centers in the UK (North London, South London, and East Anglia).14 The pairs were recruited from a convenience sample of patients utilizing these three centers for ranibizumab treatment of nAMD. To be eligible for ranibizumab therapy, the eye had to have a clinic-based visual acuity measurement of 24–73 early treatment diabetic retinopathy study (ETDRS) letters due to nAMD, with potential for improvement as recommended by the National Institute for Health and Care Excellence.15 The protocol for treatment of nAMD is similar in all the three centers, with clinical audits from each center indicating equivalent treatment outcomes. All the patients were initiated on a loading phase of monthly ranibizumab therapy for 3 months followed by 4–6 weekly review and pro-re-nata dosing. In a routine clinic appointment, the patients underwent visual acuity tests, a macular scan using optical coherence tomography, slit-lamp biomicroscopy, and were then injected with ranibizumab if deemed necessary. The clinic visit time ranged from 1–4 hours, depending on the waiting time for evaluation and treatment.
Survey tool
The MacTSQ was developed to provide a means of evaluating satisfaction with therapies for macular disease.12 The instrument is based on the Retinopathy Treatment Satisfaction Questionnaire,16 with questions specific to diabetic retinopathy being replaced by items important to patients with macular disease. The MacTSQ is a tool of 12 questions, with response options ranging on a 6-point Likert scale to rate level of satisfaction from not at all satisfied to completely satisfied, generating a range of possible total scores from 0 to 72 (Table 1). The MacTSQ provides two subscale scores: impact of treatment (range 0–36) and information provision and convenience (range 0–36).
  | Table 1 Macular Treatment Satisfaction Questionnaire (MacTSQ) |
In addition, the generic Client Service Questionnaire (CSQ-8) was also recorded to evaluate the satisfaction with health service. The CSQ-8 score is a unidimensional questionnaire that assesses the satisfaction of the service provided and does not necessarily measure the outcome of treatment. The eight questions are scored from 1 to 4, with a total maximum score of 32 (Table 2).17,18
  | Table 2 Client Service Questionnaire (CSQ-8) |
The other factors that were recorded were the demographic data, duration of AMD, number of appointments, number of ranibizumab injections, visual acuity of both eyes recorded as better and worse eye, change in visual acuity since the commencement of treatment, vision-related quality of life questionnaires (25-item National Eye Institute Visual Function Questionnaire)19 and macular disease-specific-related quality of life (MacDQoL).20 The health-related quality of life was assessed using EQ-5D-3L questionnaires.21 The EQ-5D-3L is a generic measure of health-related quality of life; it comprises five items from which a single index score can be calculated and anchored at 0 (equivalent to death) and 1.0 (“full health”).
Statistical analysis
Descriptive statistics of demographic data and Likert scale responses included counts and proportions, means (and standard deviations), and medians (and interquartile ranges). The primary outcome variable was the mean MacTSQ total score of satisfaction. Secondary outcomes included the mean subscale scores of MacTSQ and mean CSQ-8 score. Correlation matrix between covariates of the MacTSQ score were computed to assess candidacy for inclusion into a hierarchical model to assess the factors that are independently associated with MacTSQ score. All statistical analysis was completed using SPSS 20.0 (IBM Corporation, Armonk, NY, USA).
Results
A total of 273 patients were approached to recruit 250 pairs of patients and their caregivers (91.5% response rate). The characteristic of the patients are summarized in Table 3.
Treatment satisfaction scores
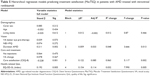
The mean MacTSQ total score was 52.7±8.9. The mean subscale scores of information provision and impact of treatment were 27.6±3.9 and 25.0±6.5 respectively. The mean total CSQ-8 score was 24.8±2.0. Correlation of MacTSQ with other variables is shown in Table 4.
The hierarchal model in Table 5 explains ~15% of the observed variance in the MacTSQ score with satisfaction with the health service, duration of AMD, and health-related quality of life being the only significant determinants within the model.
Discussion
To our knowledge, this is the first study to evaluate patient satisfaction for outcomes in nAMD treated with anti-VEGF therapy in a real-life setting. One of the main findings is that traditional clinical outcomes of visual acuity improvement and stabilization are not clearly prioritized by patients over outcomes related to the process of care.
The most important factors that determined the satisfaction were the service provided at the clinic (CSQ-8), health-related quality of life (EQ-5D-3L), and duration of AMD.
Visual acuity changes were rated as less important than one would have expected. The perception of being reviewed and injected regularly over a long period of time seems to influence the MacTSQ score more positively than the actual change in visual acuity from the treatment.
The mean change in visual acuity from baseline was 4.9 letters, which is similar to other real-life visual outcomes with ranibizumab.9,10 Both the change in visual acuity and the visual acuity on the date of interview did not determine the satisfaction score. One may attribute this to the fact that ~50% of patients had good visual acuity of at least 74 ETDRS letters in the better-seeing eye in this study. However, the MacTSQ scores were also evaluated in the REPAIR study that evaluated ranibizumab for myopic choroidal neovascularization.22 Despite a younger population (mean 55 years old) and less number of injections, the MacTSQ score did not correlate with visual acuity change or baseline visual acuity of the study eye. The scores also did not vary between the study eye being the better or the worse seeing eye. Therefore, the results of this study further substantiate the fact that the MacTSQ score is independent of visual acuity scores.
The mean MacTSQ score on patients with AMD treated with ranibizumab in real life in this study was 52.7 compared with the median of 66 in the randomized clinical trial IVAN, which compared ranibizumab and bevacizumab for AMD, indicating that satisfaction among patients in real life is lower than for those in clinical trials. This may be explained by the fact that patients generally find participation in retinal clinical trials to be a positive experience.23 The services provided in clinical trials are more patient-centered and patients are more involved in the decision-making process. Moreover, exclusion criteria in clinical trials usually result in a healthier cohort being recruited.
This study also showed that health-related quality of life is a factor that determined patient satisfaction. The mean EQ-5D-3L score in this study was 0.68 compared to 0.85 in the IVAN trial and this difference may also explain the higher satisfaction score in IVAN trial compared to this study. However, the mean EQ-5D-3L visual analog score and the utility score in this study were within the range of previous cross-sectional studies on nAMD (range 0.64–0.89 and 64–82, respectively) providing further evidence of the generalizability of this study.24,25
Another finding of this study was that there was no correlation between either 25-item National Eye Institute Visual Function Questionnaire or MacDQoL with treatment satisfaction. Therefore, this study further highlights that PROMs and patient-reported experience measures may not always correlate and therefore both these outcomes should be measured together to fully evaluate patients’ views of their symptoms, health-related quality of life, and satisfaction with treatment.
A major strength of this study is that this is the first study that has evaluated treatment satisfaction with anti-VEGF for AMD in real life. The study also prospectively evaluated all potential factors that could influence patient satisfaction with this therapy in a representative clinic catering to a diverse population. Additionally, an independent interviewer rather than a health care provider conducted the survey to reduce the response bias.
The study limitations included its cross-sectional design. We were also not able to evaluate the input of other medical conditions and relied on EQ-5D-3L. However, drug appraisals on this condition are also reliant on EQ-5D-3L.
A final area of limitation could be a selection bias. The sample was one of convenience with ambulant clients who attended the hospital visit with an unpaid carer and had volunteered for the study. It is possible that patients who are generally not overly burdened by their condition could have been more likely to volunteer, or the responses may have been in a more positive direction than for the broader community of people with nAMD. However, the effect of this would be to underplay (rather than overplay) the level of satisfaction.
In summary, this study provides an insight into treatment satisfaction of patients receiving ranibizumab therapy for nAMD and the factors that contribute to the burden. Future research in this area needs to validate these findings in different health systems in prospective comparative and longitudinal studies.
Acknowledgments
This study was funded by Macula Society and Bayer Plc Limited. The research was funded by unrestricted research grant from Macula Society, London and Bayer Plc and the National Institute for Health Research (NIHR) Biomedical Research Centre based at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. SS, RC-N, PH have received a proportion of their funding from the Department of Health’s NIHR Biomedical Research Centre for Ophthalmology at Moorfields Eye Hospital and University College London, Institute of Ophthalmology. SS, consultancy, payment for lectures/speaker bureaus, and travel support (Novartis, Allergan, Bayer); PH, consultancy and grant support (Novartis, Allergan, Bayer); and BB, consultancy and grant support (Novartis, Allergan, Bayer).
Disclosure
Phil Hykin, Ben Burton and Sobha Sivaprasad have received travel grants, research grants and attended advisory boards of Allergan, Bayer and Novartis. The authors report no other conflicts of interest in this work.
References
Fine SL, Berger JW, Maguire MG, Ho AC. Age-related macular degeneration. N Engl J Med. 2000;342(7):483–492. | ||
Evans JR, Smeeth L, Fletcher AE. Risk of admission to a nursing home among older people with visual impairment in Great Britain. Arch Ophthalmol. 2008;126(10):1428–1433. | ||
Freeman EE, Egleston BL, West SK, Bandeen-Roche K, Rubin G. Visual acuity change and mortality in older adults. Invest Ophthalmol Vis Sci. 2005;46(11):4040–4045. | ||
Buys L, Roberto KA, Miller E, Blieszner R. Prevalence and predictors of depressive symptoms among rural older Australians and Americans. Aust J Rural Health. 2008;16(1):33–39. | ||
Wang JJ, Mitchell P, Smith W, Leeder SR. Factors associated with use of community support services in an older Australian population. Aust N Z J Public Health. 1999;23(2):147–153. | ||
Chakravarthy U, Harding SP, Rogers CA, et al; IVAN study investigators. Alternative treatments to inhibit VEGF in age-related choroidal neovascularisation: 2-year findings of the IVAN randomised controlled trial. Lancet. 2013;382(9900):1258–1267. | ||
Maguire MG, Ying GS, et al; CATT Research Group, Martin DF. Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med. 2011;364(20):1897–1908. | ||
Schmidt-Erfurth U, Kaiser PK, Korobelnik JF, et al. Intravitreal aflibercept injection for neovascular age-related degeneration: ninety-six-week results of the VIEW studies. Ophthalmology. 2014;121(1):193–201. | ||
Holz FG, Tadayoni R, Beatty S, et al. Multi-country real-life experience of anti-vascular endothelial growth factor therapy for wet age-related macular degeneration. Br J Ophthalmol. 2015;99(2):220–226. | ||
Writing Committee for the UK Age-Related Macular Degeneration EMR Users Group. The neovascular age-related macular degeneration database: multicenter study of 92976 ranibizumab injections: report 1: visual acuity. Ophthalmology. 2014;121(5):1092–1101. | ||
Darzi A. High Quality Care for all: NHS Next Stage Review Final Report. London: Department of Health; 2008. | ||
Mitchell J, Brose LS, Bradley C. Design of a measure of satisfaction with treatment for macular degeneration (MacTSQ). Qual Life Res. 2007;A-120:2. | ||
Brose LS, Bradley C. Psychometric development of the Retinopathy Treatment Satisfaction Questionnaire (RetTSQ). Psychol Health Med. 2009:14(6):740–754. | ||
Gohil R, Crosby-Nwaobi R, Forbes A, Burton B, Hykin P, Sivaprasad S. Caregiver burden in patients receiving ranibizumab therapy for neovascular age related macular degeneration. PLoS One. 2015;10(6):e0129361. | ||
Macular degeneration (age-related) – ranibizumab and pegaptanib [TA155]. London: NICE. Available from: www.nice.org. Accessed April 18, 2016. | ||
Woodcock A, Plowright R, Kennedy-Martin T, Hirsch A, ffytche T, Bradley C. Development of the new Retinopathy Treatment Satisfaction Questionnaire (RetTSQ). Proceedings of Vision 2005; International Congress Series. 2005;1282:342–346. | ||
Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann. 1979;2:197–207. | ||
Malde S, Dowson C, Fraser O, et al. Patient experience and satisfaction with Onabotulinumtoxin A for refractory overactive bladder. BJU Int. 2015;116(3):443–449. | ||
Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD; National Eye Institute Visual Function Questionnaire Field Test Investigators. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001;119(7);1050–1058. | ||
Mitchell J, Wolffsohn JS, Woodcock A, et al. Psychometric evaluation of the MacDQoL individualised measures of the impact of macular degeneration on quality of life. Health Qual Life Outcomes. 2005;3:25. | ||
Brooks R EuroQol. The current state of play. Health Policy. 1996: 37:53–72. | ||
Amoaku WM, Gale RP, Lotery AJ, et al. Satisfaction and well-being in patients with myopic choroidal neovascularization treated with ranibizumab in the REPAIR study. PLoS One. 2015;10(6):e0128403. | ||
Au CP, Fardell N, Williams M, Fraser-Bell S, Campain A, Gillies M. Patient experiences in retinal trials: a cross-sectional study. BMC Ophthalmol. 2015;15:80. | ||
van Asten F, Evers-Birkenkamp KU, van Lith-Verhoeven JJ, et al. A prospective, observational, open-label, multicentre study to investigate the daily treatment practice of ranibizumab in patients with neovascular age-related macular degeneration. Acta Ophthalmol. 2015;93(2):126–133. | ||
Finger RP, Hoffmann AE, Fenwick EK, et al. Patients’ preferences in treatment for neovascular age-related macular degeneration in clinical routine. Br J Ophthalmol. 2012;96(7):997–1002. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.