Back to Journals » Open Access Journal of Clinical Trials » Volume 14
Treatment of Oropharyngeal Symptoms: A Prospective, Single-Dose, Placebo-Controlled, Randomized Clinical Trial
Authors Kapoor K , Wilhelm D, Neumeister C , Götz MR, Schwantes U, Bleckert G , Gerstenmaier L, Jambrecina A
Received 24 November 2021
Accepted for publication 10 March 2022
Published 18 March 2022 Volume 2022:14 Pages 11—23
DOI https://doi.org/10.2147/OAJCT.S331883
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Arthur E. Frankel
Katharina Kapoor,1 Dorothea Wilhelm,1 Claudia Neumeister,2 Marcus Rudolf Götz,2 Ulrich Schwantes,2 Gabriele Bleckert,3 Lilli Gerstenmaier,4 Alen Jambrecina4
1Clinical Research, Proderm GmbH, Schenefeld/Hamburg, Germany; 2Research and Development, Dr. Pfleger Arzneimittel GmbH, Bamberg, Germany; 3Statistics, Staburo GmbH, München, Germany; 4Clinical Research, CTC North GmbH & Co. KG at the University Medical Center Hamburg-Eppendorf, Hamburg, Germany
Correspondence: Claudia Neumeister, Dr. Pfleger Arzneimittel GmbH, Dr.-Robert-Pfleger-Str. 12, Bamberg, 96052, Germany, Tel +49 951 6043-161, Fax +49 951 6043-226, Email [email protected]
Purpose: Acute oropharyngeal symptoms, such as sore throat, difficulty swallowing, hoarseness, tickly throat, and dry mouth, cause great discomfort. Moistening of the impaired mucosa, caused, for example, by the common cold, air-conditioning, heated rooms, and pollen, can be achieved by providing a protective barrier through the local administration of mucoadhesives. This study investigated whether sucking and chewing a medical device (pastille) containing a specific mixture of four different polysaccharides provides instantaneous symptom-relieving effects.
Methods: This clinical study enrolled 40 patients with a sore throat (plus at least one additional acute oropharyngeal symptom). A single dose of either the new pastille or a placebo (each n = 20) was administered. The oropharyngeal symptoms, sore throat, difficulty swallowing, hoarseness, tickly throat and dry mouth were monitored on a visual analog scale at baseline and 3, 6, 10, 15, and 30 minutes after beginning sucking and chewing.
Results: Of the patients in the test group, 70% showed at least a 10% improvement regarding sore throat intensity over the observation period. Only 25% of the patients in the placebo group reported the same result. Clear improvements in symptom intensity were also found in dry mouth, tickly throat, and difficulty swallowing. For the symptom hoarseness, the effects were less pronounced.
Conclusion: Sucking and chewing of the new polysaccharides-containing pastille resulted in instant relieving effects of oropharyngeal symptoms. The effects lasted for the entire period of sucking and beyond.
Keywords: oropharyngeal symptoms, sore throat, dry mouth, polysaccharides, pastille, visual analog scale
Introduction
Acute sore throat is a highly prevalent,1,2 mostly self-limiting condition, often accompanied by oropharyngeal symptoms such as sore throat, difficulty swallowing, hoarseness, tickly throat, and dry mouth. Although it is one of the most common medical conditions resulting from consultation with a general practitioner or pharmacist, most people experiencing a sore throat do not seek medical help.3
It has been estimated that in approximately 50–95% of adults and 70% of children, sore throats are caused by infections from respiratory viruses. Bacterial infections are responsible for only 20% of cases.4,5
Environmental factors, such as airborne pollutants and allergens, cold weather and temperature, low humidity, dry air, air-conditioning, and smoking, play a significant role in developing medical respiratory tract conditions, including pharyngitis oropharyngeal symptoms and the common cold. An adult may experience two to three episodes of having a sore throat over 12 months, possibly impacting the health-related quality of life.2,6–9
As in most cases, a bacterial infection is not the cause, so antibiotics are not the recommended primary treatment for a sore throat.10,11 Most sore throat cases by complications such as fever or difficulty breathing can be treated effectively and be symptom-oriented by the patients themselves. This can be achieved through the use of over-The-counter medicines such as local analgesics and anesthetics, local antiseptic and anti-inflammatory agents, and local moisturizing and mucoadhesive formulations.12,13
However, according to the German Society of General Practice and Family Medicine guidelines, the use of local anesthetic, antiseptic and antibiotic agents is not recommended to treat sore throat due to their limited local effects and short-term effectiveness.14,15 Instead, local moisturizing therapy may be recommended if the patient requests treatment for the oropharyngeal symptoms and if other symptomatic treatments do not deliver superior efficacy.
Normally, a healthy individual’s moisturized and appropriately wetted oropharyngeal mucosa represents a protective barrier for the entry of exogenous noxious irritants, ie, by its mucociliary clearance.16,17 Therefore, one possible approach in treating oropharyngeal symptoms is the moistening of the sore, impaired mucosa by administering mucosa-protective and moisture-binding substances locally.18 Many moisture-binding substances structurally represent polysaccharides that exhibit a water-binding capacity due to their high content in hydroxyl groups. By binding water, the polysaccharides form a mucoadhesive gel where the mucoadhesive substance interacts with the mucin of the mucosa, resulting in prolonged adhesion to the mucosa.19–21
Another approach to improve the moisturization of the mucosa is by increasing the salivary flow. The stimulation of the saliva secretion from the salivary glands after gum chewing through mechanical and gustatory stimulation has been investigated and described severally.22–26 It has also been reported that gum chewing exercises increased the resting salivary secretion in older people who often suffer from reduced salivation.27
Therefore, chewable, oral formulations, such as pastilles containing moisture-binding polysaccharides, represent an option for the treatment of a sore throat by combining both of the previously described aspects: the mucoadhesive effect and the stimulation of the salivary secretion.28,29
The test product (ipalat Hydro Med® pastille, medical device) used in this study is a pastille formulation. It contains four water-binding, gel-forming agents in a flavored and sweetened base, namely gum arabic, hydroxyethyl cellulose, hyaluronic acid, and carrageenan.
Gum arabic is an edible, dried, gummy exudate from the trunk and branches of the Acacia species. This complex mixture of glycoproteins and polysaccharides is used in pharmaceutical manufacturing as a suspending and emulsifying agent, tablet binder, and pastilles.30 Hydroxyethyl cellulose is a partially substituted 2-hydroxyethyl ether of cellulose. It is used as a thickener, stabilizer, tablet-coating, and -binding agent in pharmaceutical manufacturing. It is present in preparations for treating dry eyes and dry mouth.30
Hyaluronic acid is a highly prevalent mucopolysaccharide present in human fluids and tissue that plays an important role in mucociliary clearance, tissue hydration and the defense against the spread of micro-organisms and toxic substances.31 It is extracted from cockscombs or obtained by fermentation from streptococci. It is used in many areas of medicine, for example, surgical procedures on the eye for the relief of dry eyes, intra-articular injection in the treatment of osteoarthritis, and wound care.30 Carrageenans are hydrocolloids that are extracted from red edible seaweeds. Carrageenan is used in the pharmaceutical and food industries as a suspending and gelling agent.30
When released during sucking and chewing, the polysaccharides physicochemically create a hydrogel complex. It forms a protective shield on the mucous membranes within the mouth and throat region.32 These mucoadhesive properties of the pastilles could be confirmed in mucoadhesion tests performed on the porcine buccal mucosa (ex vivo) (data not shown, internal study report Pfleger_260418_EOMPOTDIL_Final Report, study code P321, December 8, 2018). Furthermore, in a previous clinical trial, it could be shown that sucking and chewing these pastilles increased the salivary flow rate significantly and reduced the feeling of a dry mouth within the oropharyngeal cavity.29
This pilot study aimed to investigate the effect of a new pastille formulation with four different polysaccharides on oropharyngeal symptoms after single use compared to placebo to gain supportive clinical data regarding general safety and performance. Therefore, the common symptoms of a sore throat—difficulty swallowing, hoarseness, tickly throat, and dry mouth—were assessed at different points over 30 minutes, and the effect of the test product (pastille) and the placebo on symptom relief was compared.
Materials and Methods
Study Design
This pilot study was conducted as a prospective, single-center, single-dose, placebo-controlled, parallel-group, open-label, randomized clinical study at CTC North GmbH & Co KG, Hamburg, Germany. Two parallel treatment groups (test product and placebo) were compared, comprising 20 subjects each. No important changes to methods or trial outcome took place after the commencement of the trial.
The study was approved by The Ethics Committee of the Hamburg Medical Chamber (Ethikkommission der Ärztekammer Hamburg). The German Medicines and Medical Devices Agency (Bundesinstitut für Arzneimittel und Medizinprodukte) granted an exemption from the permit requirement according to §7 MPKPV (Ordinance on Clinical Trials with Medical Devices). The study was prospectively registered in the German Register of Clinical Trials (Deutsches Register Klinische Studien, DRKS), a public trials registry (DRKS-ID: DRKS00016976, Registered March 18, 2019, https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00016976).
Before conducting the study, all patients signed an informed consent form, including allowing the use of their data in this study.
For the reporting of the study results, the CONSORT guidelines were followed.
Clinical Assessment
This study’s primary objective was assessment of the relieving effect on oropharyngeal symptoms during and after sucking the test product in comparison to placebo. Therefore, the five primary endpoints—sore throat, difficulty swallowing, hoarseness, tickly throat, and dry mouth—were assessed subjectively (by questionnaire) over time (at baseline before treatment and 3, 6, 15, and 30 minutes after the start of the treatment) by the patients using a visual analog scale (VAS).
A final follow-up on general wellbeing took place 45 minutes after the start of the treatment, and the incidence, severity, device-relationship, and outcomes of adverse events (AEs) and adverse device effects (ADEs) were assessed as part of the secondary objectives for the test and the placebo.
The patients’ demographics and other baseline characteristics were also collected.
Study Treatment
A single dose of either test product (one pastille) or placebo (5x5 cm piece Parafilm “M”) (Table 1) was administered to the patients, who were instructed to suck and chew. The treatment duration for the placebo was a predefined period of five minutes. The test product was sucked/chewed until it was completely dissolved.
 |
Table 1 Study Treatments |
The patient information leaflet states the test product is a class I, CE-certified medical device (ipalat Hydro Med® pastille). It is intended to treat painful symptoms caused by irritation and/or inflammation of the mucous membranes in the oral cavity and the pharynx area, including swelling, redness, sore throat, difficulty swallowing, hoarseness, tickly throat, and dry mouth. The main ingredients are released upon sucking/chewing of the test product, intensively stimulating the salivary flow rate. Physicochemically, a mucoadhesive hydrogel complex is created, forming a protective barrier for the oropharyngeal cavity’s lasting moisturization and protection from irritating influences. The placebo, Parafilm “M,” is a tasteless wax used in other studies for the mechanical stimulation of saliva.33
Patients
This clinical study enrolled a total of 40 patients (21 female and 19 male patients). Patients who provided written informed consent and were eligible for the study were randomized in a 1:1 ratio to receive either the test product or placebo treatment. A permuted block randomization with equal treatment allocation ratio (test treatment: placebo treatment, 1:1) and a fixed block size of 10 was performed. Each block consisted of equal numbers of the two treatments where the order of treatments within the block was randomly permuted. The random allocation sequence was generated in a reproducible way by Staburo GmbH, Munich, Germany, employing the SAS-procedure’ PROC PLAN’ and uploaded in a digital format to the electronic case report form (eCRF) system of the study. Access to the allocation sequence in the eCRF system was restricted to one data manager of CTC North GmbH & Co. KG. The recruitment period lasted from March 20, 2019, until March 27, 2019 (last patient, last visit).
At screening, a physical examination of patients with oropharyngeal symptoms was performed, which included the checking of the general health condition, the mouth (furred tongue, answer option: “yes” or “no”), the throat (redness and/or swelling) and other conditions (eg, allergies). Redness and/or swelling of the pharyngeal cavity were assessed by the Investigator as previously described.34–36
The main inclusion criteria were: patients ≥ 18 years of age, with redness and/or swelling of the oropharyngeal cavity, symptomatic sore throat with an intensity of ≥ 40 mm on a VAS ranging from 0 to 100 mm, and at least one further symptom (difficulty swallowing, hoarseness, tickly throat or dry mouth) with the intensity of ≥ 40 mm on the VAS.
The main exclusion criteria were: pregnant or nursing women, oropharyngeal symptoms for more than two days, fever (≥ 38.5°C) on the day of the treatment, a prior visit to the doctor due to the acute oropharyngeal symptoms, intake of medication and/or medical devices for the treatment of oropharyngeal symptoms on the day before and on the day of the treatment, intake of analgesics 24 hours before and on the day of the treatment, pre-existing chewing and swallowing disorders and hypersensitivity to one of the ingredients.
Statistical Analysis
For this exploratory study, no formal sample size calculation was performed. A sample size of 40 patients was considered sufficient to meet the objectives of this clinical study.
Data management and analysis were done by CTC North GmbH & Co. KG. Source data were initially captured on paper and later transcribed into a tested, validated electronic case report form (double checked). According to the data validation plan, automatic edit and consistency checks were performed to ensure data validity and accuracy immediately at the point of entry into the clinical database. The database application used to capture electronic clinical trial data was fully 21 CFR Part 11 compliant. Data were analyzed using the statistics software SAS® version 9.4 or higher (SAS Institute Inc., NC, USA). All five primary endpoints were evaluated with descriptive statistics over time and by treatment group. For each patient, only those symptoms which did not exist at baseline were not followed up at the later points.
For each symptom, the patient-reported scores (VAS between 0 mm and 100 mm) for the time points 3, 6, 10, 15, and 30 minutes were analyzed descriptively (absolute symptom intensity (SI)). Based on the absolute SI difference (SID) was calculated from the SI at each assessment time by subtracting the baseline value (change from baseline symptom intensity).
Additionally, the percentage symptom intensity difference (PSID) was derived by expressing the SID per assessment time as a percentage of the baseline value (percentage change from baseline symptom intensity). For each patient and symptom, the summary measure over time “mean PSID” was obtained by the numerical integration of the linearly interpolated data points, that is, PSID values with corresponding assessment points. For a specific patient and symptom, the “mean PSID” can be interpreted as the mean percent change in symptom intensity from baseline over the 30 minutes.
All analyses of the five primary endpoints have been based on the full analysis set (FAS).
The analyses of AEs have been based on the safety population.
Results
Study Population
Forty patients, ranging from 20 to 60 years of age (mean age 34.9 years), with a mean bodyweight of 79.6 kg, a mean height of 174.0 cm completed this study and qualified for the FAS. There were no drop-outs. The study population comprised 21 (52.5%) female and 19 (47.5%) male patients. The majority of the patients were of Caucasian ethnicity (Caucasian: 92.5%; Black or African-American: 7.5%). No patient had any prior or concomitant medications.
One AE (headache) occurred in this clinical trial in the placebo group. The AE was evaluated as not related to study treatment. None of the patients dropped out of this study.
All patients (20 each in the test product and placebo group) met the inclusion criteria (redness and/or swelling of the pharyngeal cavity, sore throat, and at least one further oropharyngeal symptom) at baseline. Not all patients stated all additional symptoms and, hence, for the symptoms: difficulty swallowing, hoarseness, tickly throat, and dry mouth, patient numbers varied.
Symptom Intensity (SI)
In general, higher VAS values correspond to a higher intensity of the respective symptom.
Sore Throat
For the patients who sucked the test product, the mean VAS for sore throat fell by 20.2 mm VAS (baseline: 65.8 ± 14.3; 30 minutes after treatment start: 45.6 ± 19.2), while the mean sore throat score for the placebo decreased by 5.9 mm VAS (baseline: 66.0 ± 12.0; 30 minutes after the start of treatment: 60.1 ± 18.1). Figure 1 shows the PSID—mean intensity over time (baseline to 30 minutes)—by treatment for the symptom sore throat (mean PSID from baseline over 30 minutes: −19.9% test product; −7.7% placebo).
 |
Figure 1 Intensity of sore throat: percent symptom intensity difference–mean intensity over time by treatment, n = 20 (test product) and n = 20 (placebo). |
Difficulty Swallowing
The mean VAS for difficulty swallowing was reduced by 19.7 mm VAS (baseline: 69.1 ± 18.7; 30 minutes after the start of treatment: 49.4 ± 18.0) for the patients sucking the test product and by 2.4 mm VAS for the patients chewing the placebo (baseline: 59.6 ± 20.8; 30 minutes after the start of treatment: 57.2 ± 20.2). Figure 2 shows the corresponding PSID by treatment for difficulty swallowing symptoms (mean PSID from baseline over 30 minutes: −18.3% test product; −0.1% placebo).
 |
Figure 2 Intensity of difficulty swallowing: percent symptom intensity difference–mean intensity over time by treatment, n = 16 (test product) and n = 16 (placebo). |
Hoarseness
Concerning hoarseness, the mean VAS decreased by 11.3 mm VAS (baseline: 67.5 ± 16.1; 30 minutes after the start of treatment: 56.2 ± 19.0) for the test product and by 5.8 mm VAS for the placebo (baseline: 60.2 ± 20.5; 30 minutes after the start of treatment: 54.4 ± 17.4). Figure 3 shows the corresponding PSID by treatment for the symptom hoarseness (mean PSID from baseline over 30 minutes: −9.0% test product; −4.3% placebo).
 |
Figure 3 Intensity of hoarseness: percent symptom intensity difference–mean intensity over time by treatment, n = 13 (test product) and n = 13 (placebo). |
Tickly Throat
Figure 4 shows the corresponding PSID by treatment for the tickly throat (mean PSID from baseline over 30 minutes: −23.8% test product; −12.3% placebo). The symptom intensity for tickly throat fell by 20.5 mm VAS for the test product (baseline: 64.0 ± 24.9; 30 minutes after the start of treatment: 43.5 ± 19.0). For the placebo, a symptom reduction of 8.5 mm VAS occurred (baseline: 63.9 ± 22.2; 30 minutes after the start of treatment: 55.4 ± 21.1).
 |
Figure 4 Intensity of tickly throat: percent symptom intensity difference–mean intensity over time by treatment, n = 17 (test product) and n = 15 (placebo). |
Dry Mouth
Figure 5 shows the corresponding PSID by treatment for the symptom dry mouth (mean PSID from baseline over 30 minutes: −32.8% test product; −16.7% placebo). The dry mouth feeling decreased almost by 50% and was reduced on average by 35.2 mm VAS (baseline: 76.8 ± 17.7; 30 minutes after the start of treatment: 41.6 ± 18.0) for the test product. A less pronounced reduction in dry mouth feeling was evident for the placebo, accounting for 8.3 mm VAS on average (baseline: 57.7 ± 17.2; 30 minutes after the start of treatment: 49.4 ± 18.8).
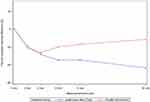 |
Figure 5 Intensity of dry mouth: percent symptom intensity difference–mean intensity over time by treatment, n = 12 (test product) and n = 11 (placebo). |
Overall, a higher reduction of the intensity of the symptoms occurred for all five parameters 30 minutes after the start of the treatment with the test product, ranging from 11.3 mm VAS to 35.2 mm VAS. For the placebo, the symptom intensities declined on average between 2.4 mm VAS and 8.3 mm VAS. Placebo treatment had a small immediate relieving effect, but only the test product showed continuous symptom improvement in terms of intensity compared to the placebo group.
Furthermore, during the assessment period, the relief of the symptom of dry mouth accounted for almost 50% and was, therefore, the highest among the five parameters in the test product group. A comparable magnitude reduced the symptoms of a sore throat, difficulty swallowing and tickly throat. The lowest relief after treatment with the test product was observed for the parameter hoarseness.
For the placebo, the highest relief was evident for tickly throat and dry mouth symptoms during the assessment period. While a comparable reduction in the VAS was observed for the symptoms of sore throat and hoarseness, the lowest symptom relief for the placebo occurred for the parameter difficulty swallowing. In addition to Figures 1-5, the descriptive statistics on the SIs are provided in Supplementary Table 1 of the Supplementary Data. Furthermore, for each symptom and each treatment summary statistics over time are shown graphically in terms of boxplots for percent symptom intensity difference (PSID) in Supplementary Figures 1-5 of the Supplementary Data.
Mean Percent Symptom Intensity Difference (Mean PSID)
For each patient and symptom, the mean PSID described the mean percent change of symptom intensity from baseline over 30 minutes and served to assess changes in perception of the symptoms (improvement, no change, worsening). In order to assess symptom improvement, the proportion of patients reporting a mean PSID from baseline over the 30 minutes of at least 10%, 25%, 50%, and 75% was calculated by the treatment group.
An improvement in the symptom intensity of at least 10% was observed in the majority of the patients (53.8%–83.3%, Table 2) for all five symptoms 30 minutes sucking/chewing the test product. In comparison, the mean PSID of at least 10% for the placebo was between 12.5% and 54.5%.
 |
Table 2 Mean Percent Symptom Intensity Difference (Mean PSID) of at Least 10%–(FAS) |
An improvement of at least 25% for the symptom intensity was observed in 50.0% and 41.2% of the patients receiving the test product for the symptoms of dry mouth and tickly throat, followed by 31.3%, 25.0%, and 15.4% for the symptoms: difficulty swallowing, sore throat and hoarseness, respectively. Compared to this, at least 25% improvement in the placebo group was observed in less than half of the percentages of the test product for each symptom. An improvement in the symptom intensity of at least 50% and 75% was observed in less than 20% of the subjects concerning the five symptoms (supplementary Data, Supplementary Tables 2-6).
Discussion
Acute oropharyngeal symptoms such as a sore throat, difficulty swallowing, hoarseness, tickly throat, and dry mouth are commonly treated with various topical over-The-counter products, including gargles, sprays, pastilles, and lozenges. Their main properties aim to target the sore area directly, provide a local, immediate, and prolonged soothing and pain-relieving effect, and be effective for a variety of oropharyngeal symptoms while displaying a good safety profile. Pastilles and lozenges usually provide the most sustained delivery of active ingredients within the oropharyngeal cavity.37
Many of these topical formulations contain analgesic, anesthetic, antiseptic and anti-inflammatory active ingredients and have shown a positive outcome in clinical trials.38–41
As the guideline for managing a sore throat, the German Society of General Practice and Family Medicine recommend moisturizing substances acting on the function of the pharyngeal mucous, this clinical study investigated a new pastille formulation, containing the four polysaccharides gum arabic, hydroxyethylcellulose, sodium hyaluronate, and carrageenan, for the treatment of oropharyngeal symptoms after a single-dose administration in comparison to placebo.
In this study, for all five parameters investigated (sore throat, difficulty swallowing, hoarseness, tickly throat, and dry mouth), a reduction in the absolute symptom intensity was observed 30 minutes after the treatment with the test product. The symptom of a dry mouth was relieved the most after sucking/chewing the test product. This finding is in line with the result of a previous clinical trial where the test product significantly improved the symptom of a dry mouth.29 Sucking and chewing of the placebo reduced the symptoms only slightly.
Considering the descriptive nature of the results and the inter-individual study design (which generally contributes to a higher variability when comparing the data sets of different treatments), these findings indicate a better relief of the oropharyngeal symptoms after sucking/chewing the test product as compared to the placebo.
However, the baseline VAS values for the symptom of a dry mouth of the test product and the placebo group differed markedly, which may also have contributed to the most prominent relief of the symptom of a dry mouth after administration of the test product. Although the relief of the symptoms was more pronounced after administering the test product than after the placebo administration, any conclusions on the magnitude of the symptom relief should be drawn cautiously.
As described earlier in this study, the overall symptom relief can be attributed to the mechanical stimulation during sucking and chewing, which leads to increased salivary secretion and, in turn, improves moisturization of the oropharyngeal mucosa.
The just-described mechanisms may also explain why a slight symptom relief was also observed after sucking/chewing the placebo during this study. The mechanical action of sucking/chewing the placebo stimulated salivary secretion, and through increased oropharyngeal moisturization, symptom relief was perceived. However, the absence of any gustatory or mucoadhesive effects resulted in an overall less pronounced symptom-relieving effect.
The better symptom relief after administration of the test product in this study can be further ascribed to forming a muco-protective film. Normally, the salivary mucins and proteins contained in the saliva lubricate the oropharyngeal mucosa and form a protective barrier against exogenous noxious agents.43,44 Lubrication and hydration result from the interaction of the negatively charged moieties of the mucin (glycosylated region) with water molecules from the saliva.45
Therefore, upon contact with the saliva, the water-binding, gel-forming polysaccharides contained in the test product (gum arabic, hydroxyethylcellulose, sodium hyaluronate, carrageenan) form a mucoadhesive solution (hydrogel complex32) which interacts with the mucin of the mucosa, forming a protective film. This interaction, in turn, has a positive, soothing effect on the oropharyngeal symptoms.22,46
The formation of a muco-protective film and, in turn, a soothing effect are likely to present over a prolonged period, as gum arabic was present in saliva samples up to 10 minutes after administration of the pastille, beyond cessation of the sucking/chewing activity.29
In this pilot study, the test product was sucked/chewed until complete dissolution (mean duration of 9.45 ± 2.89 minutes), while the treatment duration for the placebo was predefined to five minutes. Likely, the longer treatment time for the test product (in comparison to the placebo) may have contributed to the overall more pronounced and prolonged symptom relief.
A relatively swift increase in saliva secretion upon chewing, with a maximum being reached after approximately 1 minute, has previously already been described.42 Therefore, for the four symptoms of a sore throat, difficulty swallowing, hoarseness, and tickly throat, maximum relief was evident up to approximately three minutes after the start of sucking/chewing the placebo. This period may be representative of the onset and maximum effect of the mechanical stimulation of saliva secretion.
The overall highest relief of the dry mouth symptom may also be explained by the fact that this symptom responded the best to an increased salivary flow rate due to its physicochemical nature. In contrast, for the other symptoms, more complex physiological and immunological pathways may also be involved.
Concerning the product’s safety, only one adverse event (headache) occurred in the placebo group, and this was evaluated as not being related to the study treatment. This is in line with the good tolerability of the pastille shown in the previous study.29 Hence, there were no concerns regarding the safety of the test product.
Lastly, when interpreting these study results, the population size varied to assess the five symptoms and was relatively small (< 20 patients in each group). However, the results show a promising effect on oropharyngeal symptoms, already after just a single-dose application. An investigation in a larger study population including a coordinated treatment duration over a couple of consecutive days (more representative of the prevalence/duration of oropharyngeal symptoms) may reveal even more pronounced effects.
Conclusion
This study indicates that oropharyngeal symptoms such as a sore throat, difficulty swallowing, hoarseness, tickly throat, and dry mouth are alleviated after single-dose administration for at least 30 minutes after sucking/chewing the test product. Most patients profited from the administration of the mucoadhesive hydrogel complex to alleviate the symptoms.
This finding adds to our previous Research on salivary secretion. Initially, within the first 3 to 6 minutes, the symptom-relieving effect can most likely be ascribed to both an increase in salivary secretion upon sucking/chewing and the formation of a mucoadhesive hydrogel complex on the oropharyngeal mucosa. After that, the symptom relief likely continues due to the moisturizing and lubricating effect of the mucoadhesive hydrogel complex.
Overall, the test product was well-tolerated and provided a greater symptom relief than mechanical stimulation of saliva secretion after administration of the placebo.
Abbreviations
ADE, adverse device effects; AE, adverse event; BfArM, Bundesinstitut für Arzneimittel und Medizinprodukte; BL, baseline; FAS, full analysis set; MPKPV, Verordnung über klinische Prüfungen von Medizinprodukten (Ordinance on Clinical Trials with Medical Devices); OCT medicines, over-the-counter medicines; PSID, percentage symptom intensity difference; SI, symptom intensity; SID, symptom intensity difference; VAS, visual analog scale (ranging from 0 mm to 100 mm).
Data Sharing Statement
The datasets used and/or analyzed during the current study and the full trial protocol are available on reasonable request from CTC North GmbH & Co. KG and Dr. Pfleger Arzneimittel GmbH.
Ethics Approval
The study was conducted in accordance with the ethical principles based on the current version of the Declaration of Helsinki.47 The approval of the Ethics Committee and the exemption from the permit requirement of the BfArM (according to §7 MPKPV) were obtained before the start of the clinical trial. Copies of the approval documents were forwarded to the sponsor and were included in the Clinical Investigation Report. No substantial amendments occurred within this clinical trial.
Consent to Participate
Before obtaining the patient’s consent, information was given by the Investigator in language and at a level of complexity understandable to the patient in both verbal and written form. Before participation in the study, the written consent form was signed and personally dated by the patient and the Investigator. The patient received a copy of the signed and dated consent form.
Acknowledgments
The authors would like to thank Dr. Carlos Heras Bautista for their contribution to the tables shown in this publication. The authors would like to thank Enago for the English language review.
Author Contributions
All authors made a significant contribution to the work reported. KK, DW have drafted and revised the article. CN, MRG, US, LG, AJ took part in the conceptualization, design and conduct of the clinical trial and interpretation of the data as well as in revising and critically reviewing the article. GB was responsible for the statistical analysis and preparation of the figures. All authors have substantially revised and critically reviewed the article and agreed on the journal to which the article has been submitted. All authors read and approved the final version that was published and agree to be accountable for all aspects of the work.
Funding
This study was designed by Dr. Pfleger Arzneimittel GmbH in cooperation with CTC North GmbH & Co. KG. Clinical conduct, data collection, data entry, interpretation of data, and writing of the study report were performed by CTC North GmbH & Co. KG. Statistical analysis was done by Staburo GmbH, Munich, Germany, a subcontractor of CTC North GmbH & Co. KG. Writing of the manuscript was done by proDERM GmbH. Review and discussion of the manuscript were performed by proDERM GmbH in cooperation with Dr. Pfleger Arzneimittel GmbH and CTC North GmbH & Co. KG. The study was funded by Dr. Pfleger Arzneimittel GmbH, Dr.-Robert-Pfleger-Str. 12, 96052 Bamberg, Germany. The test products were provided by Dr. Pfleger Arzneimittel GmbH.
Disclosure
The authors of this manuscript either had a contractual service agreement with the sponsor (proDERM Institute for Applied Dermatological Research and CTC North GmbH & Co. KG and Staburo GmbH (subcontractor)) or were employed by the sponsor itself (Dr. Pfleger Arzneimittel GmbH).
References
1. Danchin MH, Rogers S, Selvaraj G, et al. The burden of group A streptococcal pharyngitis in Melbourne families. Indian J Med Res. 2004;119(Suppl May 2004):
2. Addey D, Shephard A. Incidence, causes, severity and treatment of throat discomfort: a four-region online questionnaire survey. Ear Nose Throat Disorders. 2012;12(9):875.
3. Hannaford P, Simpson J, Bisset A, Davis A, McKerrow W, Mills R. The prevalence of ear, nose and throat problems in the community: results from a national cross-sectional postal survey in Scotland. Fam Pract. 2005;22(3):
4. Summers A. Sore throats. Accid Emerg Nurs. 2005;13(1):15–17.
5. Worrall G. Acute sore throat. Can Fam Physician. 2007;57(7):1961–1962.
6. Schwartz J. Air pollution and the duration of acute respiratory symptoms. Arch Environ Health. 1992;47(2):116–122.
7. Triche EW, Belanger K, Bracken MB, et al. Indoor heating sources and respiratory symptoms in non-smoking women. Epidemiology. 2005;16(3):377–384.
8. Becker W, Naumann H, Pfaltz C. Ear, Nose and Throat Diseases: A Pocket Reference. New York: Thieme Medical Publishers; 1989.
9. Mäkinen T, Juvonen R, Jokelainen J, et al. Cold temperature and low humidity are associated with increased occurrence of respiratory tract infections. Respir Med. 2009;103(3):456–462.
10. Marshall S. Giving advice on sore throats. Pharm J. 2008;280:127–130.
11. Del Mar C, Glasziou P, Spinks A. Antibiotics for sore throat. Cochrane Database Syst Rev. 2006;11:CD000023.
12. Oxford J, Leuwer M. Acute sore throat revisited: clinical and experimental evidence for efficacy of over-The-counter AMC/DCBA throat lozenges. Int J Clin Pract. 2011;65(5):524–530.
13. Dao VA, Overhagen S, Bilstein A, Kolot C, Sonnemann U, Mösges R. Ectoine lozenges in the treatment of acute viral pharyngitis: a prospective, active-controlled clinical study. Eur Arch Otorhinolaryngol. 2019;276(3):775–783.
14. Wächtler H, Chenot J. Die Halsschmerz-Leitlinie der Deutschen Gesellschaft für Allgemeinmedizin und Familienmedizin. HNO. 2011;59(5):
15. Wittig T. GeloRevoice versus Isländisch Moos und Kochsalz. Pharm Ztg. 2015;160(14):
16. Hong-Seop KHO. Understanding of Xerostomia and Strategies for the Development of Artificial Saliva. Chine J Dental Res. 2014;17(2):
17. Gupta A, Singh TK, Saxsena A. Role of oral care to prevent VAP in mechanically ventilated Intensive Care Unit patients. Saudi J Anaesth. 2016;10(1):95–97.
18. Boni J, Plohmann B, Sauerland S. Boehringer Ingelheim International GmbH, Sanofi Aventis Deutschland GmbH (current assignee). Lozenge for treating a sore throat, hoarseness, and associated dry cough and for treating inflammatory diseases of the oral cavity and of the pharynx. European Patent Office EP2981275A1. 2016. Available from: https://worldwide.espacenet.com/patent/search/family/047997281/publication/EP2981275A1?q=EP2981275A1.
19. Malviya R, Srivastava P, Kulkarni GT. Applications of Mucilages in Drug Delivery–A Review. Advan Biol Res. 2011;5(1):
20. Nerkar PP, Gattani S. In vivo, in vitro evaluation of linseed mucilage based buccal mucoadhesive microspheres of venlafaxine. Drug Deliv. 2011;18(2):111–121.
21. Hartleb H, Lang C, Wegener T, Staigner C. Erkältungsbedingte Anwendung einer Kombination aus Isländisch Moos, Hyaluronsäure und Hydrogelkomplex. Zeitschrift für Phytotherapie. 2016;37:4–8.
22. Jenkins G, Edgar W. The effect of daily gum-chewing on salivary flow rates in man. J Dent Res. 1989;68(5):
23. Jensen J, Karatsaidis A, Brodin P. Salivary secretion: stimulatory effects of chewing-gum versus paraffin tablets. Eur J Oral Sci. 1998;106(4):
24. Jensen Kjeilen J, Brodin P, Aars H, Berg T. Parotid salivary flow in response to mechanical and gustatory stimulation in man. Acta Physiol Scand. 1987;131(2):
25. Souza LR, Oliveira MVM, Basile JR, et al. Anatomical and Physiopathological Aspects of Oral Cavity and Oropharynx Components Related to Oropharyngeal Dysphagia. Seminars in Dysphagia. 2015. doi:10.5772/60766
26. Bots CP, Brand HS, Veerman BM, van Amerongen BM. Preferences and saliva stimulation of eight different chewing gums. Int Dent J. 2004;54:
27. Nakagawa K, Matsuo K, Takagi D, et al. Effects of gum chewing exercises on saliva secretion and occlusal force in community-dwelling elderly individuals: a pilot study. Geriatr Gerontol Int. 2017;17(1):
28. Patel S, Goyal A. Applications of Natural Polymer Gum Arabic: a Review. Int J Food Properties. 2015;18:986–998.
29. Bielfeldt S, Wilhelm D, Neumeister C, Schwantes U, Wilhelm KP. Effect of a newly developed pastille on the salivary flow rate in subjects with dry mouth symptoms: a randomized, controlled, monocentric clinical study. BMC Oral Health. 2021;21:117.
30. Brayfield A. Martindale: The Complete Drug Reference
31. Pignataro L, Marchisio P, Ibba T, Torretta S. Topically administered hyaluronic acid in the upper airway: a narrative review. Letter to the editor. Int J Immunopathol Pharmacol. 2018;32:
32. Gebrauchsinformation ipalat® Hydro Med Lutschpastillen [package insert]; Dr. Pfleger Arzneimittel GmbH, Stand August 2018; 2018, Available from: www.ipalat.de.
33. Gittings S, Turnball N, Henry B, Roberts CJ, Gershkovich P. Characterisation of human saliva as a platform for oral dissolution medium development. Eur J Pharmaceutics Biopharmaceutics. 2015;91:16–24.
34. Bethke G, Reichart P. Schweregradbestimmung des oralen Lichen planus mit einem neuen klinischen Index. Oral Maxillofac Surg. 2005;9(3):152–160.
35. Bethke G Die topische Therapie des oralen Lichen planus mit Methylprednisolonaceponat versus Triamcinolonacetonid. Eine prospektive, randomisierte, doppelblinde, placebokontrollierte, klinische, immunhistologische und mikrobiologische Studie. Berlin: charité Zentrum für Zahn-, Mund- und Kieferheilkunde - Universitätsmedizin Berlin; 2009. Available from: www.diss.fu-berlin.de/diss/receive/FUDISS_thesis_000000007039.
36. Saric A. Aktuelle Leitlinie zur Behandlung des Lichen ruber planus Mucosae- Eine Konklusion der Literatur. Universitätsklinik für Zahnmedizin und Mundgesundheit Graz; 2009.
37. Limb M, Connor A, Pickford M, et al. Scintigraphy can be used to compare delivery of sore throat formulations. Int J Clin Pract. 2009;63(4):
38. Bouroubi A, Donazzolo Y, Donth F, et al. Pain relief of sore throat with a new anti-inflammatory throat lozenge, ibuprofen 25 mg: a randomised, double-blind, placebo-controlled, international Phase III study. Int J Clin Pract. 2017;71:e12961. doi:10.1111/ijcp.12961
39. Schachtel BP, Shephard A, Shea T, et al. Flurbiprofen 8.75 mg lozenges for treating sore throat symptoms: a randomized, double-blind, placebo-controlled study. Pain Manag. 2016;6(6):
40. Hayward GN, Hay AD, Moore MV, et al. Effect of Oral Dexamethasone Without Immediate Antibiotics vs. Placebo on Acute Sore Throat in Adults, A Randomized Clinical Trial. JAMA. 2017;317(15):1535–1543.
41. De Mey C, Koelsch S, Richter E, Pohlmann T, Sousa R. Efficacy and safety of ambroxol lozenges in the treatment of acute uncomplicated sore throat—a pooled analysis. Drug Res. 2016;66(7):384–392.
42. Dawes C, Macpherson LMD. Effects of Nine Different Chewing-Gums and Lozenges on Salivary Flow Rate and pH. Caries Res. 1992;26:
43. Pedersen AML, Sorensen CE, Protor GB, Carpenter GH. Salivary functions in mastication, taste and textural perception, swallowing and initial digestion. Oral Dis. 2018;24:1399–1416.
44. Mikos AG, Peppas NA. Measurement of the surface tension of mucin solutions. Int J Pharm. 1989;53:1–5.
45. Coles JM, Chang DP, Zauscher S. Molecular mechanisms of aqueous boundary lubrication by mucinous glycoproteins. Curr Opin Colloid Interface Sci. 2010;15:406–416.
46. Malviya R, Srivastava P, Kulkarni GT. Applications of Mucilages in Drug Delivery - A Review. Advan Biol Res. 2011;5(1):
47. World Medical Association. Declaration of Helsinki. Ethical principles for medical research involving human subjects.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
