Back to Journals » Neuropsychiatric Disease and Treatment » Volume 17
Treatment Continuation of Asenapine or Olanzapine in Japanese Schizophrenia Patients: A Propensity Score Matched Study
Authors Matsuzaki H, Hatano M , Iwata M, Yamada S
Received 11 October 2021
Accepted for publication 1 December 2021
Published 14 December 2021 Volume 2021:17 Pages 3655—3661
DOI https://doi.org/10.2147/NDT.S343840
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Taro Kishi
Haruna Matsuzaki,1 Masakazu Hatano,1,2 Miko Iwata,1 Shigeki Yamada1
1Department of Clinical Pharmacy, Fujita Health University School of Medicine, Toyoake, Aichi, Japan; 2Department of Psychiatry, Fujita Health University School of Medicine, Toyoake, Aichi, Japan
Correspondence: Masakazu Hatano
Fujita Health University School of Medicine, 1-98 Dengakugakubo, Kutsukake, Toyoake, Aichi, 470-1192, Japan
Tel +81 562932157
Fax +81 562934537
Email [email protected]
Objective: Asenapine is a second-generation antipsychotic agent that is classified as a multi-acting receptor-targeted antipsychotic and is similar to olanzapine. Our study aimed to compare the treatment continuation rate and reason for discontinuation of asenapine or olanzapine in schizophrenia using real-world data.
Methods: This design was a retrospective study. The primary endpoint was Kaplan–Meier estimates of the continuation rate at six months, with the propensity score method applied to adjust for potential confounders.
Results: A total of 95 patients were analyzed in this study (asenapine, n = 46; olanzapine, n = 49). Matched data were adjusted to consider six covariates (age, sex, chlorpromazine equivalent, diazepam equivalent, history of clozapine use, and history of modified electro convulsive therapy). The continuation rate at six months was 27.3% (95% CI, 15.6– 47.6) in the asenapine group and 50.8% (95% CI, 34.3– 75.3) in the olanzapine group (hazard ratio, 0.41; 95% CI, 0.21– 0.82; P = 0.0088 by the Log rank test) in matched data. Cases of discontinuation because of the lack of efficacy were almost as frequent for asenapine (13.0%) as for olanzapine (10.2%). Discontinuation due to bitter taste (6.5%) and burden of the dosing method (6.5%) were observed only with asenapine, whereas anticholinergic side effects such as dry mouth (4.1%) and constipation (2.0%) were observed only with olanzapine.
Conclusion: The low continuation rate of asenapine in real-world data may be related to specific factors such as bitter taste and burden of the dosing method.
Keywords: asenapine, olanzapine, antipsychotic agents, schizophrenia, retrospective studies, propensity score
Introduction
The mainstay of treatment for schizophrenia is pharmacotherapy with antipsychotics, and it is important to maintain and improve adherence to medication to prevent relapse. Non-adherence to antipsychotic medication has been reported to increase the risk of relapse by five times,1,2 which is a major concern for continued pharmacotherapy. In August 2009, the US Food and Drug Administration approved asenapine for the treatment of schizophrenia and bipolar I disorder. Asenapine has been shown to improve Positive and Negative Syndrome Scale (PANSS) significantly more than placebo.3 Although there is limited evidence for direct comparisons with other antipsychotics, no significant difference between asenapine and olanzapine in terms of changes to PANSS total or negative subscale scores has been reported thus far.4 In the largest network meta-analysis, asenapine was ranked toward the middle out of 32 antipsychotics in overall change in symptoms.5
Asenapine has a high affinity for dopamine (D1, D2, D3, D4), serotonin (5-HT1A, 5-HT1B, 5-HT2A, 5-HT2B, 5-HT2C, 5-HT5, 5-HT6, 5-HT7), histamine (H1, H2), and α-adrenergic (α1, α2A, α2B, α2C) receptors and acts as an antagonist for each.6 It is classified as multi-acting receptor-targeted antipsychotic, but has no affinity for muscarinic M1 receptors compared with olanzapine and quetiapine in the same category.6 This pharmacological profile provides the advantage that asenapine has a low risk of anticholinergic side effects (constipation and dry mouth, among others). In addition, asenapine has been shown in clinical trials to cause less weight gain than olanzapine.7 However, asenapine has been reported to cause oral hypoesthesia as a specific side effect in approximately 10% of patients owing to local anesthetic activity.3 A further unique feature of asenapine is that it is the only antipsychotic designed as a sublingual tablet. This is attributable to its extensive hepatic first-pass metabolism and an oral bioavailability of <2%.8 Therefore, it is recommended to avoid eating and drinking for 10 minutes after administration; however, concern that this complicated dosing method may lead to poor medication adherence exists. Sublingual tablets are known to cause the inconvenience of oral administration.9 A questionnaire survey of asenapine in Japan revealed that 32% of patients felt burdened by the dosing methods of sublingual tablets, suggesting that for of medication decreases satisfaction.10 However, the relationship between these factors and treatment continuation has generally been rarely evaluated in detail in clinical trials. The purpose of this study was to compare the continuation rates of treatment between asenapine and olanzapine, and to determine differences in the reasons for discontinuation.
Methods
Study Design
This design was a retrospective study based on the medical records of patients at Fujita Health University Hospital. Patients who were diagnosed with schizophrenia or schizoaffective disorder according to the definitions outlined in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition, and who were prescribed asenapine or olanzapine between September 2016 and December 2019 were included in the study. Patients who were prescribed asenapine or olanzapine for temporary use in case of worsening of symptoms or as an alternative drug when existing drugs could not be used due to surgery or ileus were excluded. From medical records, we extracted data on patient characteristics (age, sex, and treatment history) and clinical course. The total dose of each antipsychotic and benzodiazepine was calculated by converting the dose to chlorpromazine and diazepam equivalents, respectively.11 Clozapine or modified electro convulsive therapy history was assessed that because treatment continuation rates may be underestimated in treatment-resistant schizophrenia.
The primary endpoint was the continuation rate of treatment at six months. The secondary endpoint was the reason for discontinuation of each antipsychotic. The reasons for discontinuation were categorized as “within 1 month” or “1–6 months.”
Study procedures were performed in accordance with the principles of the Declaration of Helsinki, and this study was approved by the Institutional Review Board of Fujita Health University (HM19-050). Patients had the right to revoke their consent and opt out from the research.
Statistical Analysis
We used propensity score matching to adjust for potential confounders. The propensity score was estimated through a logistic regression model that considered six covariates (age, sex, chlorpromazine equivalent, diazepam equivalent, history of clozapine use, and history of modified electro convulsive therapy). We performed a nearest-neighbor matching algorithm without replacement using a caliper width equal to 0.2 of the standard deviation of the logit of the propensity score. We matched asenapine group and olanzapine group in a 1:1 ratio according to these covariates. The balance of the covariates between asenapine and olanzapine was checked using the standardized mean difference (SMD), with <10% being considered well balanced. The continuation rate of treatment with asenapine or olanzapine was calculated by the Kaplan–Meier method, and the Log rank test was performed to evaluate differences between the two groups. The Cox proportional hazards model was used to estimate the hazard ratio and 95% confidence interval for asenapine as compared with that for olanzapine). P-values were two-sided, and those less than 0.05 were considered significant. The sample size was determined from the number of subjects enrolled within the study period. All statistical analyses were performed with R 3.4.3 (The R Foundation for Statistical Computing).
Results
Patient Characteristics
Data on 99 patients who were asenapine or olanzapine were extracted from medical records, and four patients were excluded from the study owing to temporary use. Thus, 95 patients were analyzed in this study, of which 46 were in the asenapine group (mean age ± standard deviation [SD], 42.0 ± 15.3; males, 18) and 49 were in the olanzapine group (mean age ± SD, 43.8 ± 15.6; males, 18). Before propensity score matching, each treatment group differed in all characteristics except sex. After propensity score matching (33 asenapine cases matched with 33 olanzapine cases), the SMD were less than 10% for all covariates. Thus, the covariate balance in the matched data was well adjusted. The patient characteristics at baseline are summarized in Table 1.
 |
Table 1 Patient Characteristics |
Treatment Continuation Rate
The continuation rates of treatment as calculated by the Kaplan–Meier method are shown in Figure 1 (before propensity score matching) and Figure 2 (after propensity score matching). Before propensity score matching, the continuation rate at six months as calculated by the Kaplan–Meier method was 23.9% (95% CI, 14.3–40.0) for the asenapine group and 51.7% (95% CI, 37.7–71.1) for the olanzapine group (hazard ratio, 0.39; 95% CI, 0.22–0.68; P = 0.00063 by the Log rank test) (Figure 1). After propensity score matching, the continuation rate at six months was 27.3% (95% CI, 15.6–47.6) for the asenapine group and 50.8% (95% CI, 34.3–75.3) for the olanzapine group (hazard ratio, 0.41; 95% CI, 0.21–0.82; P = 0.0088 by the Log rank test) (Figure 2).
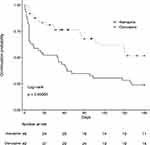 |
Figure 1 Continuation rate of treatment calculated by the Kaplan–Meier method before propensity score matching. |
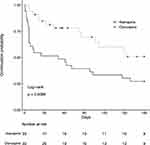 |
Figure 2 Continuation rate of treatment calculated by the Kaplan–Meier method after propensity score matching. |
Reasons for Discontinuation
Details of the reasons for discontinuation of each antipsychotic are shown in Table 2. The reasons for discontinuation observed in >10% of the patients were lack of efficacy (13.0%, 6/46 patients) and insomnia (10.9%, 5/46 patients) for asenapine, and weight gain (14.3%, 7/49 patients) and lack of efficacy (10.2%, 5/49 patients) for olanzapine. When discontinuation was limited to within one month, asenapine was most frequently discontinued due to akathisia (8.7%, 4/46 patients). Olanzapine was correlated with the highest weight gain within 1 month (6.1%, 3/49 patients) and between 1–6 months (8.2%, 4/49 patients). Discontinuations due to bitter taste (6.5%, 3/46 patients) and burden of the dosing method (6.5%, 3/46 patients) were observed only in asenapine cases, whereas anticholinergic side effects such as dry mouth (4.1%, 2/49 patients) and constipation (2.0%, 1/49 patients) were observed only in olanzapine cases. Discontinuation owing to weight gain was observed in only one of the asenapine cases.
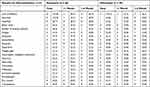 |
Table 2 Reason for Discontinuation of Each Antipsychotic |
Discussion
This study evaluated the continuation rates of treatment and reasons for discontinuation of asenapine and olanzapine using real-world data. Asenapine had a significantly lower continuation rate than olanzapine. In addition, the same result was shown in analysis using propensity score matching to account for age, sex, antipsychotic and concomitant medication dose, and treatment history. A previous meta-analysis reported that there was no difference between asenapine and olanzapine in the rate of treatment discontinuation due to adverse events or lack of efficacy, but the overall rate of treatment continuation was significantly lower for asenapine.4 Although the cause of this difference was not discussed in detail, our findings suggest that the distinct differences in reasons for discontinuation of asenapine compared to olanzapine are relevant. In other words, factors for discontinuation of asenapine treatment do not fall under the general efficacy and safety assessment.
Cases of discontinuation because of the lack of efficacy were almost as frequent for asenapine as for olanzapine, which supported the results reported in a previous meta-analysis.4 Therefore, bitter taste and burden of the dosing method were reasons for discontinuation observed only in asenapine cases, and these factors may contribute to the lower continuation rate for asenapine. Asenapine has a local anesthetic activity and is known to cause oral hypoesthesia,12 which generally resolves within one hour13 but might affect patient adherence to medication. Although the incidence of oral hypoesthesia was reported in only ~10% of cases studied in a previous randomized controlled trial,3 spontaneous reports using open questions of healthy male subjects have shown an incidence of oral paresthesia in more than 20% of cases, which was as high as 75% when mild oral paresthesia was included.14 A questionnaire survey on the experience of oral hypoesthesia when taking asenapine among schizophrenic patients in Japan similarly revealed that ~70% of patients experienced a bitter taste after asenapine administration.10 These data indicate that oral hypoesthesia occurs in the majority of patients, yet it is likely to be latent in real-world practice. Although these symptoms are generally perceived to be mild, our results suggest that oral hypoesthesia can cause patients to discontinue the medication. Moreover, all three patients who complained of bitter taste discontinued asenapine within a month, which indicates that bitter taste is one of the main reasons for early discontinuation. Therefore, informing patients about these potential side effects before they take asenapine is necessary.
Another characteristic reason for the discontinuation of asenapine is burden of the dosing method. Asenapine is the only antipsychotic that has been developed as a sublingual tablet, which requires the patient to avoid eating and drinking for 10 minutes after administration. A survey on the formulations of antipsychotics showed that 22.2% of patients complained about the dosing method.15 As with oral hypoesthesia, the burden of the dosing method is not directly associated with psychopathological mechanisms but is an important factor affecting patients’ adherence to medication. Furthermore, non-compliance with this dosing method can cause a lack of elevated blood concentrations, which may be misinterpreted as insufficient efficacy and lead to discontinuation.
In contrast, the main reasons for discontinuation of olanzapine were weight gain and anticholinergic side effects, which were rarely observed with asenapine. Compared to asenapine, olanzapine has been associated with a significantly higher risk of weight gain, and our results support this finding.5 Four out of seven patients in the present study experienced weight gain and discontinued use after one month of treatment. Continuous monitoring of patients is recommended, even in the maintenance phase. In terms of anticholinergic side effects, although constipation and dry mouth were the only reasons for discontinuation of olanzapine, a variety of other symptoms, such as dysuria and cognitive impairment, might occur in real-world practice.16 It should also be noted that these anticholinergic symptoms might appear after long-term use of more than 6 months.
Our study has several limitations. We used the propensity score method to control for potential confounders but were only able to adjust for six covariates in total, including age, sex, antipsychotic and concomitant medication dose, and treatment history. Other confounders, such as psychiatric symptoms, co-morbid medical/physical health disorders, and concomitant medications (non-psychiatric), could not be considered owing to the lack of information in the medical records. Furthermore, the present study revealed the difference in reasons for discontinuation of asenapine compared with olanzapine, but the data were only numerically compared and not statistically analyzed due to the small sample size. Therefore, these factors must be analyzed using a larger data set.
In conclusion, real-world data suggest that asenapine has a significantly lower treatment continuation rate than olanzapine. Part of this difference may be due to the bitter taste and burden of the dosing method experienced when taking asenapine. Although these are not directly related to psychopathological mechanisms and are generally non-serious factors, they can lead to poor adherence to medication. To help ensure patients continue asenapine treatment, it is important to inform them of the side effect of bitter taste before the drug is administered, as well as confirm the dosing method regularly.
Acknowledgments
The authors would like to thank MARUZEN-YUSHODO Co., Ltd. for the English language editing.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Robinson D, Woerner MG, Alvir JMJ, et al. Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Arch Gen Psychiatry. 1999;56(3):241–247. doi:10.1001/archpsyc.56.3.241
2. Caseiro O, Pérez-Iglesias R, Mata I, et al. Predicting relapse after a first episode of non-affective psychosis: a three-year follow-up study. J Psychiatr Res. 2012;46(8):1099–1105. doi:10.1016/j.jpsychires.2012.05.001
3. Kinoshita T, Bai YM, Kim JH, Miyake M, Oshima N. Efficacy and safety of asenapine in Asian patients with an acute exacerbation of schizophrenia: a multicentre, randomized, double-blind, 6-week, placebo-controlled study. Psychopharmacology (Berl). 2016;233(14):2663–2674. doi:10.1007/s00213-016-4295-9
4. Orr C, Deshpande S, Sawh S, Jones PM, Vasudev K. Asenapine for the treatment of psychotic disorders: a systematic review and meta-analysis. Can J Psychiatry. 2017;62(2):123–137. doi:10.1177/0706743716661324
5. Huhn M, Nikolakopoulou A, Schneider-Thoma J, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019;394(10202):939–951. doi:10.1016/S0140-6736(19)31135-3
6. Citrome L. Asenapine review, part I: chemistry, receptor affinity profile, pharmacokinetics and metabolism. Expert Opin Drug Metab Toxicol. 2014;10(6):893–903. doi:10.1517/17425255.2014.908185
7. Kemp DE, Zhao J, Cazorla P, et al. Weight change and metabolic effects of asenapine in patients with schizophrenia and bipolar disorder. J Clin Psychiatry. 2014;75(3):238–245. doi:10.4088/JCP.12m08271
8. Balaraman R, Gandhi H. Asenapine, a new sublingual atypical antipsychotic. J Pharmacol Pharmacother. 2010;1(1):60–61. doi:10.4103/0976-500X.64538
9. Zhou M, Derakhshanian S, Rath A, et al. Asenapine transdermal patch for the management of schizophrenia. Psychopharmacol Bull. 2020;50(4):60–82.
10. Kamei H, Kuno M, Takeuchi I, et al. A survey of schizophrenia patients’ satisfaction with a second-generation antipsychotic agent, sublingual asenapine. Jpn J Clin Psychopharmacol. 2018;21(11):1495–1506.
11. Inada T, Inagaki A. Psychotropic dose equivalence in Japan. Psychiatry Clin Neurosci. 2015;69(8):440–447. doi:10.1111/pcn.12275
12. Citrome L. Asenapine review, part II: clinical efficacy, safety and tolerability. Expert Opin Drug Saf. 2014;13(6):803–830. doi:10.1517/14740338.2014.908183
13. Vieta E, Montes JM. A review of asenapine in the treatment of bipolar disorder. Clin Drug Investig. 2018;38(2):87–99. doi:10.1007/s40261-017-0592-2
14. Gerrits M, De Greef R, Peeters P. Effect of absorption site on the pharmacokinetics of sublingual asenapine in healthy male subjects. Biopharm Drug Dispos. 2010;31(5–6):351–357. doi:10.1002/bdd.718
15. Hatano M, Takeuchi I, Yamashita K, et al. Satisfaction survey on antipsychotic formulations by schizophrenia patients in Japan. Clin Psychopharmacol Neurosci. 2021;19(4):610–617. doi:10.9758/cpn.2021.19.4.610
16. Quinn TJ, Myint PK, McCleery J, Taylor-Rowan M, Stewart C. Anticholinergic burden (prognostic factor) for prediction of dementia or cognitive decline in older adults with no known cognitive syndrome. Cochrane Database Syst Rev. 2020;2020(2). doi:10.1002/14651858.cd013521
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
