Back to Journals » Local and Regional Anesthesia » Volume 15
Transmuscular Quadratus Lumborum Block versus Infrainguinal Fascia Iliaca Nerve Block for Patients Undergoing Elective Hip Replacement: A Double-blinded, Pilot, Randomized Controlled Trial
Authors Hashmi J , Cusack B, Hughes L, Singh V, Srinivasan K
Received 8 January 2022
Accepted for publication 28 June 2022
Published 6 July 2022 Volume 2022:15 Pages 45—55
DOI https://doi.org/10.2147/LRA.S350033
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Stefan Wirz
Junaid Hashmi, Barbara Cusack, Lauren Hughes, Vikash Singh, Karthikeyan Srinivasan
Department of Anaesthesia and Intensive Care, Tallaght University Hospital, Dublin, Ireland
Correspondence: Junaid Hashmi, Department of Anaesthesia and Intensive Care, Our Lady of Lourdes Hospital, Drogheda, Louth, Ireland, Tel +353419837601, Fax +353 41 9833868, Email [email protected]
Purpose: Transmuscular quadratus lumborum (TQL) block has been described as an effective option for postoperative analgesia in patients undergoing hip replacement with single injection described as providing analgesia for up to 24 h. We hypothesize that a TQL block, when compared to fascia iliaca block (FIB), will provide better analgesia and less motor block in the initial 24-h postoperative period.
Patients and Methods: Fifty patients undergoing elective hip replacement surgery, ASA I–III, were included in the study. Patients were randomized into two groups. Patients in group A received spinal anesthesia followed by FIB. Patients in group B received spinal anesthesia followed by TQLB. Postoperative pain scores and motor block were assessed at 6 and 24 hours. The primary outcome measure was 24 h total morphine consumption. Secondary outcome measures included pain score (VNS) and motor block (modified Bromage scale) at 6 and 24 h postoperatively.
Results: There was no statistical difference in morphine consumption between the two groups (p-value 0.699). There was no difference in pain scores at 6 h (p-value 0.540) or 24 h (p-value 0.383). There was no difference in motor block at 6 h (p-value 0.497) or at 24 h (p-value 0.773).
Conclusion: Transmuscular quadratus lumborum block along with spinal anesthesia for patients undergoing elective hip replacement surgery does not reduce opioid consumption or motor weakness when compared to fascia iliaca block. The results and conclusion apply to a dose of 20 mL of 0.25% bupivacaine used in each group.
Keywords: pain scores, motor block, opioid consumption
Introduction
Total hip replacement is a commonly performed surgical procedure with up to 4500 procedures performed annually in Ireland and 400,000 procedures per year being performed in the United States.1 Moderate to severe pain in the initial postoperative period, which can delay mobilization and rehabilitation, is a particular concern among these patients.2 Peripheral nerve block forms an important component of a multimodal analgesia-based approach in such patients. The objective of multimodal analgesia in such cases is to effectively manage pain with no or minimal use of opioids.2 Fascia iliaca nerve block (FIB), femoral nerve block (FNB) and pericapsular nerve group (PENG) block are among such peripheral nerve blocks that are used across different institutions for hip replacement surgery.3 Owing to its simplicity and effectiveness FIB is currently the technique of choice in our institution. However FIB only provides a limited duration of analgesia with the single injection technique and the associated motor block can also delay early mobilization.4
Quadratus lumborum block (QLB) is a relatively new block and results have been encouraging. A study of transmuscular quadratus lumborum block (TQLB) in patients undergoing elective hip arthroplasties, has described significant reduction in length of stay and intraoperative opioid use.5 A retrospective study comparing TQLB, FNB, and FIB in patients undergoing hip arthroscopies concluded that TQL group had lower total opioid requirements and lower pain scores at discharge than patients receiving preoperative FIB/FNB blocks.6 Among the different versions of QLB the transmuscular quadratus lumborum (TQL) nerve block, owing to its spread to lumbar nerve roots and thoracic paravertebral space, has been shown to provide effective and long-lasting analgesia in a wide range of lower abdominal and pelvic surgeries involving T4-L1 sensory levels.7 We therefore tested the primary hypothesis that a single injection TQL block will significantly reduce cumulative morphine consumption in the initial postoperative period and may be an effective alternative to FIB.
Materials and Methods
Study Design
This single-center, prospective, assessor blinded, randomized controlled trial was conducted, according to the Declaration of Helsinki principles, in patients undergoing total hip replacement surgery from June 2018 to June 2019. Ethical committee approval was granted by the Research Ethics Committee (REC) of Tallaght University Hospital, Ireland. The study was registered with and approved by a clinical trial registry (Clinicaltrials.gov identifier NCT03551860). Written informed consent was obtained from all the patients who participated in the study.
All American Society of Anesthesiology (ASA) class I–III patients aged greater than 18 years and due to undergo elective total hip replacement under spinal anesthesia were included into the study. Patients having localized infection at the site of injection of the spinal anesthetic or nerve block, history of allergy to local anesthetics, severe coagulopathy, revision hip arthroplasty surgery, poor anatomical view and those in which consent to participate was not obtained or those patients who were unable to give informed consent, were excluded from the study. Eighty-six patients were screened among which 59 met the inclusion criteria and eventually 50 were included in the study (Figure 1). All patients who were scheduled for hip replacement surgery and met study inclusion criteria were contacted preoperatively (a minimum of 24 h pre-admission) by telephone. Information about the nature and purpose of the study was provided by anesthesia personnel involved in study recruitment. A link to the study specific website was texted to the patient’s phone after their explicit verbal consent was obtained. Randomization was conducted using a computer generated randomization sequence. Group allocation and study protocol instructions were enclosed in sealed envelopes which were opened in the anesthetic room by the anesthesiologist performing the procedure. All blocks were performed by a single consultant anesthesiologist, experienced in the performance of peripheral nerve blocks, to minimize inter-individual variation in quality of blocks. Anesthesiologists in the operating theater, outcome assessors, and data analyzers were blinded to the study group allocation.
 |
Figure 1 Flow diagram of number of patients enrolled, randomized, allocated to the two groups, followed-up and analyzed. |
Management of Spinal Anesthesia and Perioperative Pain
In the anesthesia induction room baseline monitoring (NIBP, pulse oximetry and 3-lead ECG) and IV access were established. Patients in both of the groups were positioned sitting on a trolley with feet resting on a stool. Patients were requested to maintain an arched back posture with an assistants support to aid positioning. No premedication was given. Spinal anesthesia was performed under strict aseptic precautions (chlorhexidine 0.5% for skin decontamination with anesthetist performing the procedure scrubbed wearing sterile gown, cap, and sterile gloves). A 25G Whitacre needle was used and 3.2 mL 0.5% plain bupivacaine was administered.
Ultrasound Guided Fascia Iliaca Block
Following the administration of spinal anesthetic an 80 mm 22G insulated echogenic needle (Stimuplex® Ultra 360®) with 30° bevel needle was used to perform FIB. Patients were positioned supine. A linear high frequency probe (8–13 MHz) was then placed along the inguinal crease to identify the femoral artery, femoral nerve and iliacus fascia. The needle was advanced using an in-plane technique from lateral to medial side and local anesthetic was deposited under the fascia iliaca. Twenty milliliters of 0.25% bupivacaine was administered under US guidance following careful intermittent aspiration (Figure 2).
 |
Figure 2 Fascia iliaca block (infrainguinal approach). The image shows the site of injection (white arrow), femoral artery, fascia iliaca and the iliopsoas muscle. |
Ultrasound-guided Transmuscular Quadratus Lumborum Block (TQLB)
Following the administration of spinal anesthetic a 100 mm 22G insulated echogenic needle (Stimuplex® Ultra 360®) with 30° bevel needle was used to perform TQL block. Patients were positioned in lateral decubitus position with operating side up. A curvilinear low frequency probe (2–5 MHz) was placed transversely in the midaxillary line above the iliac crest at level of L2 lumbar vertebrae and the following structures were identified (i) transverse process, (ii) erector spinae muscle, (iii) quadratus lumborum muscle, and (iv) psoas major muscle. The needle was advanced using in-plane technique from posterior to anterior direction and local anesthetic was deposited in the fascial planes between psoas major and quadratus lumborum muscles, anterior to QL. Twenty milliliters of 0.25% bupivacaine was administered under US guidance following careful intermittent aspiration (Figure 3).
 |
Figure 3 Transmuscular quadratus lumborum block. The image shows the site of injection (white arrow), quadratus lumborum muscle, psoas major muscle, transverse process and the vertebral body. |
Standard Perioperative Care and Measurements of Pain
Patients received multimodal intraoperative IV medication as follows: paracetamol 1g, parecoxib 40 mg, tranexamic acid 1 g. If individual patients had a contraindication to any of these medications eg an NSAID, then these medications were omitted.
In the postanesthesia recovery unit (PACU), morphine 2 mg increments up to a maximum of 10mg were given intravenously by recovery nursing staff every 5 min if the patient reported VNS>4. In patients needing more than 10 mg of morphine in recovery, the anesthetist was requested to review the patient. Postoperatively all patients were prescribed regular oral paracetamol 1g every 6 h and oral celecoxib 200 mg every 12 h. Antiemetics (ondansetron 4 mg every 8 h and cyclizine 50 mg every 8 h) were prescribed for patients to be administered as required. All patients were explained about morphine PCA preoperatively and all patients received morphine PCA (1 mg/mL concentration, 1 mg dose, 5 min lockout period, and max 40 mg in 4 h) in the postoperative period for 24 h. Institutional protocol for morphine PCA (CADDR-Solis Pump, Figure 4) was used, in which criteria for evaluation and steps for management of side effects of morphine such as respiratory depression, sedation, nausea, vomiting, pruritus, are detailed. Although in case of respiratory depression, high sedation scores and/or difficulty in managing other side effects the anesthesia registrar on call has to be informed.
 |
Figure 4 Morphine PCA pump (CADDR-solis pump). |
Outcome Measure
The primary outcome was total morphine consumption, within the first 24 h, in both the groups. The secondary outcome was verbal numerical scale (VNS) for pain at rest and on movement, ranging from 0–10 where 0 is no pain and 10 is maximum possible pain. Also the motor power in the lower limbs was assessed using the modified Bromage scale.
Sample Size and Statistical Analysis
Based on previous study26 a sample size of 46 patients (23 per group) was calculated. This was based on a 50% reduction in morphine consumption with power of 80%, beta error of 0.2 and alpha error of 0.05%. To allow for potential patient drop out and loss to follow-up, a total of 50 patients were recruited. We chose 50% reduction as TQL block has been shown to have broader dermatomal cover (T4-S1) and longer duration of action (up to 24 h) which should lead to better pain related outcomes for total hip arthroplasty.
Normally distributed data are presented as mean ±standard deviation. A comparison between groups was performed using the unpaired t-test and the chi-squared test. The comparison of VNS for pain between groups was performed using the Mann–Whitney U-test. A comparison of motor block between the two groups was performed using the chi-squared test. A p-value of <0.05 was considered to represent a statistically significant difference.
Results
A total of 86 patients were screened and 59 patients were deemed eligible for study inclusion. Fifty patients consented and were randomized in the study. Two of these patients, one from Group A and one from Group B, were converted to general anesthetic due to inadequate block intraoperatively (Figure 1) and were excluded from the study.
There was no difference between the groups based on the demographic variables of the American Society of Anesthesiologists (ASA) Classification, Sex, and Weight (Table 1).
 |
Table 1 Comparison of Baseline Characteristics of Study Participants Between Groups |
There was no statistically significant difference between the groups based on the use of type of analgesics perioperatively (Table 2), duration of surgery (Table 3), 24 h morphine consumption, 6 and 24 h pain scores at rest or movement (Table 4). There was no difference in motor block characteristics between the two groups at 6 h (Table 5) and 24 h, respectively (Table 6).
 |
Table 2 Comparison of Analgesia Use Between Groups |
 |
Table 3 Comparison of Duration of Surgery, Morphine Use and Postoperative Pain Scale Between the Groups |
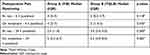 |
Table 4 Comparison of Postoperative Pain Using Verbal Rating Scale Between the Groups |
 |
Table 5 Comparison of Motor Block (Modified Bromage Scale) at Six Hours Post Block Between the Groups |
 |
Table 6 Comparison of Motor Block (Modified Bromage Scale) at 24 Hours Post Block Between the Groups |
Discussion
Transmuscular QLB did not reduce 24 h opioid consumption compared to infrainguinal fascia iliaca block for total hip replacement. To our knowledge this is the first randomized study which prospectively evaluates transmuscular quadratus lumborum block against fascia iliaca block in patients undergoing hip replacement (posterior surgical approach) under spinal anesthesia.
While the exact mechanism of analgesia provided by TQLB is not fully understood it is considered that the spread of local anesthetic through the thoracolumbar fascia and the endothoracic fascia into the paravertebral space provides analgesia.8 Various studies have shown that QLB provides opioid sparing benefits and effective analgesia in hip surgeries.9–12 However most of these studies on QLB for hip surgeries have either used anterior approach to QLB or are limited to case reports.13,14 Also in the randomized studies on QLB for hip surgeries, QLB was shown to be superior when compared to a control group in which no block was used.9,15
There are different versions of quadratus lumborum block based upon the site of injection relative to the quadratus lumborum muscle. QL1 or lateral QLB refers to the deposition of local anesthetic lateral to the QL muscle. QL2 or posterior QLB refers to injection posterior to the QL muscle QL3 or anterior QLB, also referred to as the transmuscular approach due to the typical needle approach, refers to injection anterior to the QL muscle at the level of the L4 vertebral body.16
Of all the variants of QLB we chose TQLB for a few reasons. Previous cadaveric studies have shown that only TQLB consistently spreads to lumbar nerve roots as well as within the psoas major and the quadratus lumborum muscle while other variants had an unreliable spread.17,18 Also the patients need to be positioned in lateral position for the surgery which makes it easier to perform TQLB. TQLB works at the paravertebral level, preferentially blocking lower thoracic segments while the caudad spread is limited to the iliac crest.7,19 We believe this can provide analgesia to the hip area but may not significantly cause quadriceps weakness which is supplied by L3, 4, 5. In contrast fascia iliaca block consistently causes quadriceps weakness4,20 with incidence up to 4%.21 Adequate pain control with minimal or no muscle weakness is vital in ensuring early ambulation in the postoperative period. Early ambulation after hip surgeries has been shown to be associated with reduced complications and death.22 Therefore, we wanted to compare TQLB with fascia iliaca block which is the standard in our institution.
FIB is a technically straightforward block to perform with easier target visualization by using a linear probe. TQLB is a deeper block requiring use of a curvilinear probe and is technically more challenging to perform as the planes may not be very obvious. This may necessitate the use of saline to hydro-dissect the space prior to local anesthetic injection. There is no benefit in replacing an easy block with a relatively difficult one unless there is a definite clinical benefit. Hence we powered the study for a large effect size.
However, the results of this randomized controlled trial demonstrate that in patients undergoing elective hip replacement surgery the TQL single injection nerve block does not lead to a statistically significant reduction in morphine consumption or motor block in the initial postoperative period when compared to FIB single nerve injection block. One possible reason for lack of difference in morphine consumption was that we compared TQLB to fascia iliaca block. In contrast, previous studies on QLB, compared its effectiveness against no block.9,15
The lack of motor block was most likely due to the fact that the study was not powered to detect the difference in this secondary outcome. It is therefore possible that small differences in motor block might have been missed. Although one study has mentioned a higher incidence of motor weakness in the group receiving TQLB in comparison to the group receiving lateral QLB in patients undergoing percutaneous nephrolithotomy,23 but there is no clear evidence yet about the incidence of motor block after QLB in general, and TQL in particular, in patients undergoing hip surgery. In our study one patient from each group had complete motor weakness at 6 h and two patients from each group had “almost complete” block at 6 h. But this was attributed to residual effect of spinal anesthesia.
The study has some limitations. The study was conducted in a single center and included a small number of patients, therefore it is possible that a smaller effect size might have been missed.
TQL block is a deeper block and technically more challenging compared to fascia iliaca block. We believe that at least a 50% reduction is needed to justify its routine use especially if it is going to replace a simple and easier block like fascia iliaca block.
Although the study has a small sample size it is adequately powered to have picked up this effect if it had happened. There is a chance though that we might have missed a smaller reduction in opioid consumption. Detecting smaller differences, however, would have increased the sample size significantly, which would have made it impossible for us to do this study in a single center.
Another potential limitation of the study is that we used the modified Bromage scale for motor weakness assessment. This scale measures the level of motor block based on the patient’s ability to move their lower extremities, but both the knee flexion and foot movements can still be performed despite quadricep muscle weakness. Yet it is a simple and reproducible system to measure the motor block and measures weakness in hip flexors (which are important for ambulation) effectively. In addition, the modified Bromage scale has been consistently used in numerous studies comparing fascia iliaca block/quadratus lumborum block.24,25 Hence we decided to go ahead with it.
While the study has its limitations yet it adds to the growing evidence that TQLB has so far demonstrated no major advantages over a simple, practical, and effective block like FIB in patients undergoing hip replacement surgery. Furthermore, our study showed that there is no difference in the degree of motor block between the two groups.
Conclusion
In conclusion, TQLB failed to demonstrate any advantage over FIB in terms of reduction in morphine usage, better pain control or less motor weakness in patients undergoing elective primary hip replacement surgery. Further studies with a larger sample size will be required to evaluate for the presence of a smaller effect size.
Data Sharing Statement
The de-identified clinical trial data (study protocol, clinical data and results) which supports the findings of this study is available on reasonable request to the corresponding author. It will be available following publication and will end at five years after publication.
Acknowledgments
The authors received a grant to the sum of €1000 from the Irish Society of Regional Anaesthesia for conducting this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Petis SM, Howard JL, Lanting BA, Marsh JD, Vasarhelyi EM. In-hospital cost analysis of total hip arthroplasty: does surgical approach matter? J Arthroplasty. 2016;31(1):53–58. doi:10.1016/j.arth.2015.08.034
2. Gaffney CJ, Pelt CE, Gililland JM, Peters CL. Perioperative pain management in hip and knee arthroplasty. Orthop Clin North Am. 2017;48(4):407–419. doi:10.1016/j.ocl.2017.05.001
3. Jyoti D, Promil K, Hari K. Review of current practices of peripheral nerve blocks for hip fracture and surgery. Curr Anesthesiol Rep. 2020;10:259–266. doi:10.1007/s40140-020-00393-7
4. Matthias B, Edward NY, Zhang AL. Preoperative fascia iliaca block does not improve analgesia after arthroscopic hip surgery but causes quadriceps muscles weakness: a randomized, double-blind trial. Anaesthesiology. 2018;129:536–554. doi:10.1097/ALN.0000000000002321
5. Stuart GM, Ryan HC, Iqbal U, Olabisi IO, Hurd B. Transmuscular quadratus lumborum block reduces length of stay in patients receiving total hip arthroplasty. Anesth Pain Med. 2018;8(6):e80233. doi:10.5812/aapm.80233
6. Blackwell RE, Kushelev M, Norton J, Pettit R, Vasileff WK. A comparative analysis of the quadratus lumborum block versus femoral nerve and fascia iliaca blocks in hip arthroscopy. Arthrosc Sports Med Rehabil. 2020;3(1):e7–e13. doi:10.1016/j.asmr.2020.08.002
7. Dam M, Moriggl B, Hansen CK, Hoermann R, Bendtsen TF, Børglum J. The pathway of injectate spread with the transmuscular quadratus lumborum block: a cadaver study. Anesth Analg. 2018;125:303–312. doi:10.1213/ANE.0000000000001922
8. Akerman M, Pejčić N, Veličković I. A review of the quadratus lumborum block and ERAS. Front Med. 2018;5:44. doi:10.3389/fmed.2018.00044
9. Kukreja P, MacBeth L, Sturdivant A, et al. Anterior quadratus lumborum block analgesia for total hip arthroplasty: a randomized, controlled study. Reg Anesth Pain Med. 2019;44:1075–1079.
10. Christopher LM, Bruce BD, Jason J, Vonda JW. Quadratus lumborum block provides improved immediate postoperative analgesia and decreased opioid use compared with a multimodal pain regimen following hip arthroscopy. J Hip Preserv Surg. 2018;5(3):233–239. doi:10.1093/jhps/hny024
11. Parras T, Blanco R. Randomized trial comparing the transversus abdominis plane block posterior approach or quadratus lumborum block type I with femoral block for postoperative analgesia in femoral neck fracture, both ultrasound-guided. Rev Esp Anestesiol Reanim. 2016;63(3):141–148.
12. Desmet M, Vermeylen K, Van HI. A longitudinal supra-inguinal fascia iliaca compartment block reduces morphine consumption after total hip arthroplasty. Reg Anesth Pain Med. 2017;327(3):327–333.
13. La Colla L, Ben-David B, Merman R. Quadratus lumborum block as an alternative to lumbar plexus block for hip surgery: a report of 2 cases. AA Pract. 2017;8(1):4–6.
14. Hockett MM, Hembrador S, Lee A. Continuous quadratus lumborum block for postoperative pain in total Hip arthroplasty: a case report. AA Case Rep. 2016;7(6):129–131. doi:10.1213/XAA.0000000000000363
15. Kim YJ, Kim HT, Kim HJ, et al. Ultrasound-guided anterior quadratus lumborum block reduces postoperative opioid consumption and related side effects in patients undergoing total hip replacement arthroplasty: a propensity score-matched cohort study. J Clin Med. 2021;10(20):4632. doi:10.3390/jcm10204632
16. Elsharkawy H, El-Boghdadly K, Barrington M. Quadratus lumborum block: anatomical concepts, mechanisms and techniques. Anesthesiology. 2019;130:322–335. doi:10.1097/ALN.0000000000002524
17. Carline L, McLeod GA, Lamb C, Colvin L. A cadaver study comparing spread of dye and nerve involvement after three different quadratus lumborum blocks. Br J Anaesth. 2016;117(3):387–394. doi:10.1093/bja/aew224
18. Adhikary SD, El-Boghdadly K, Nasralah Z, Sarwani N, Nixon AM, Chin KJ. A radiologic and anatomic assessment of injectate spread following transmuscular quadratus lumborum block in cadavers. Anaesthesia. 2017;72(1):73–79. doi:10.1111/anae.13647
19. Kadam VR, Roelof MVW, Guy LL, Venkatesan T. Anatomical and ultrasound description of two transmuscular quadratus lumborum block approaches at L2 level and their application in abdominal surgery. Anaesth Intensive Care. 2019;47(2):141–145. doi:10.1177/0310057X19839931
20. Paul JE, Arya A, Hurlburt L. Femoral nerve block improves analgesia outcomes after total knee arthroplasty: a meta-analysis of randomized controlled trials. Anaesthesiology. 2010;113:1144–1162. doi:10.1097/ALN.0b013e3181f4b18
21. Dai W, Hu X, Hu X, et al. The effect of fascia iliaca block on postoperative pain and analgesic consumption for patients undergoing primary total hip arthroplasty: a meta-analysis of randomized controlled trials. J Orthop Surg Res. 2021;16:444. doi:10.1186/s13018-021-02585-1
22. Manuel B, Valentin N, Christoph PH, Ciritsis B. Influence of mobilization and weight bearing on in-hospital outcome in geriatric patients with hip fractures. SICOT-J. 2019;5:4. doi:10.1051/sicotj/2019005
23. Chen L, Ji J, Tian Y, et al. Retrospective study of quadratus lumborum block for postoperative analgesia in patients undergoing percutaneous nephrolithotomy. BMC Anesthesiol. 2020;20:217. doi:10.1186/s12871-020-01134-3
24. Sophia MB, Biboulet P, Swisser F. Posterior quadratus lumborum block in total hip arthroplasty: a randomized controlled trial. Anesthesiology. 2021;134:722–733. doi:10.1097/ALN.0000000000003745
25. Shaimaa F, Mostafa G, EidRehab S. Patient-controlled fascia iliaca compartment block versus fentanyl patient-controlled intravenous analgesia in patients undergoing femur fracture surgery. Egypt J Anaesth. 2018;34(1):9–13. doi:10.1016/j.egja.2017.12.002
26. Cagla B, Ozlem O, Eker H, Murat H, Aribogan A. Postoperative analgesic efficacy of fascia iliaca block versus periarticular injection for total knee arthroplasty. J Clin Anesth. 2016;35:404–410. doi:10.1016/j.jclinane.2016.08.030
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
