Back to Journals » Clinical Interventions in Aging » Volume 14
Total knee arthroplasty in Japanese patients aged 80 years or older
Authors Kodaira S , Kikuchi T , Hakozaki M , Konno S
Received 7 November 2018
Accepted for publication 9 February 2019
Published 15 April 2019 Volume 2019:14 Pages 681—688
DOI https://doi.org/10.2147/CIA.S193694
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
Shunsuke Kodaira,1,2 Tadashi Kikuchi,1 Michiyuki Hakozaki,2 Shinichi Konno2
1Department of Orthopaedic Surgery, Bange Kosei General Hospital, Fukushima, Japan; 2Department of Orthopaedic Surgery, Fukushima Medical University School of Medicine, Fukushima, Japan
Objective: The population of Japan is aging rapidly, and, since the aging of patients who undergo total knee arthroplasty (TKA) is also expected, it is necessary to determine the efficacy and safety of TKA among old adult patients.
Methods: This study retrospectively analyzed the cases of patients who underwent a primary TKA for osteoarthritis at Bange Kosei General Hospital between January 2009 and June 2014 and were postoperatively followed-up for ≥1 year. Among the 2,945 knees of the 1,968 patients, 1,003 knees of 679 patients aged ≥80 years at the time of surgery were designated as the older group, and we compared their cases with those of the younger group of 1,044 knees of 673 patients aged
Results: The rates of improvement of the Japanese Orthopaedic Association (JOA) score were not significantly different between the older and younger groups. Postoperative ranges of motion were significantly improved in both groups. The number of postoperative days of hospital stay in the older group was 2 days longer than that of the younger group. Concerning postoperative complications, confusion, delayed wound healing, and acute heart failure were significantly more frequent in the older group. The frequencies of pneumonia, cerebral infarction, peroneal nerve palsy, and bedsore did not differ significantly. Loosening of implants was observed: older group, n=0 joints; younger group, n=5 joints. The number of prosthetic joint infections: older group, n=5; younger group, n=2 (non-significant).
Conclusion: The rate of improvement in the JOA score did not differ significantly between the groups. TKA is an effective and safe treatment for osteoarthritis, even in old adult patients, when the surgical indication is based on careful preoperative screening and attention to specific postoperative complications.
Keywords: osteoarthritis, knee, total knee arthroplasty, Japanese, old adults, complications, JOA score
Introduction
Total knee arthroplasty (TKA) is widely indicated for advanced osteoarthritis or rheumatoid arthritis of the knee. Numerous clinical studies have reported the efficacy and safety of TKA for old adult patients.1–5 The safety of TKA has been improved based on the recent advances in anesthesia, perioperative health care, and surgical techniques, especially for older patients.6,7 On the other hand, the relevance between effectiveness and patients’ age has not become clear, and the background of patients who benefit by receiving TKA is still unknown.8 A re-evaluation of the effectiveness and safety of TKA for old adult patients is, thus, needed. We conducted the present study to clarify the effectiveness and safety of TKA in Japanese patients aged ≥80 years with the largest-ever number of patients.
Patients and methods
Study design and ethics statement
This study was a non-invasive retrospective observational study. The opt-out method of obtaining informed consent was adopted. The patients were anonymized to protect their personal information. This study was approved by the ethical review committee of Bange Kosei General Hospital (BANRIN 17–001), and the study was performed in accordance with approved guidelines and regulations.
Patients
We retrospectively analyzed the cases of consecutive patients (all Japanese) who underwent a primary TKA for osteoarthritis at Bange Kosei General Hospital between January 2009 and June 2014 and were postoperatively followed-up for ≥1 year. Among the 2,945 knees of these 1,968 patients (Figure 1), we designated the 1,003 knees of the 679 patients aged ≥80 years at the time of surgery as the “older group,” and we compared their cases with those of the “younger group” of the 1,044 knees of the 673 patients aged <75 years. The intermediate-age group (75≤ years <80), of 898 knees of 616 patients, the most frequent generation of TKA, were excluded from this study for the purpose of highlighting the differences of clinical outcome between the younger and older group by excluding the transitional generation. The distribution of the TKA patients is shown in Figure 1; the older-group patients were 80–94 years old, and the younger-group patients were 47–75 years old. The breakdown of follow-up period in both groups is shown in Figure 2.
  | Figure 2 The breakdown of postoperative follow-up period. The follow-up period in the younger group is significantly longer than the older group (p<0.05). |
Surgical procedure and postoperative treatment
All the operations were performed under spinal anesthesia, and an air tourniquet was not used. The TKA prosthesis used in this series was the Scorpio NRG, posterior stabilized (PS), or cruciate retaining (CR) type (Stryker, Mahwah, NJ, USA), and patellar replacement was performed in all cases. All the operations were performed or supervised by an experienced surgeon (TK).
Continuous cooling was performed until postoperative day (POD) 2, and physical therapies consisting of walking exercise and range of motion (ROM) exercise were started from POD 3 under management by physical therapists. Continuous passive motion was not performed. Discharge from the hospital was allowed when the patient was able to walk steadily and unassisted. Postoperative physical therapy was performed only during the hospital stay; ambulatory or in-home physical therapies after discharge were not performed.
Evaluation items
The six items we determined in each group and used for the between-group comparison were as follows: 1) the patient’s Japanese Orthopaedic Association (JOA) score,9 2) the pre- and postoperative ROM of the knee, 3) the number of postoperative days of hospital stay, 4) postoperative complications, 5) loosening of implants, and 6) prosthetic joint infection (PJI).
The JOA score is composed of four categories; (I) pain on walking; (II) pain on ascending or descending stairs; (III) ROM; and (IV) joint effusion (Table 1). The rate of improvement in the patient’s total JOA score [(postoperative JOA score-preoperative JOA score)/preoperative JOA score×100] was calculated, whereas the rate of improvement in each category were not calculated because “zero-point” existed in some cases.
  | Table 1 The Japanese Orthopaedic Association (JOA) score for osteoarthritic knees |
The postoperative JOA score and postoperative ROM were calculated based on the patient’s maximum score. When a TKA was performed bilaterally in the same period of hospital stay, the operations were performed one-by-one, and the number of postoperative days of hospital stay was calculated from the second operation. As postoperative complications, confusion and peroneal nerve palsy for the duration of acute phase, pneumonia, cerebral infarction, acute heart failure and bedsore in the period of hospital stay, and delayed wound healing throughout the follow-up period were evaluated. Wound healing was defined as delayed when re-suturing of a surgical wound was required.
Statistical analysis
We used the Mann–Whitney U-test for the comparisons of body weight (BW), body mass index (BMI), radiological grading (Kellgren-Lawrence [KL] grade10), femorotibial angle (FTA), JOA score, ROM, and follow-up period. We used Pearson’s chi-square test to examine correlations between two dichotomous variables of gender, the number of patients who received TKA bilaterally, the type of TKA implant, the presence of a past medical history (ie, diabetes mellitus, ischemic heart disease, and high blood pressure), and the occurrences of postoperative complications, loosening of implants, and PJI. In all examinations, a p-value <0.05 was considered significant. The data analyses were performed using Statcel 3 software (OMS Publishing, Saitama, Japan).
Results
Patients
The patients’ characteristics are summarized in Table 2. The percentage of female patients, BW, BMI, KL grade, FTA, the number of patients who received TKA bilaterally, the type of TKA implant (PS vs CR type), and past medical histories of diabetes mellitus or ischemic heart disease differed significantly between the older and younger groups, but the rate of high blood pressure did not.
The rate of improvement of the JOA score
The total preoperative JOA scores of the older and younger groups were 48.1±0.3 and 51.0±0.3 points, respectively. The total postoperative JOA scores of the older and younger groups were 82.8±0.4 and 87.4±0.3 points, respectively (Figure 3). The improvement rates were 77.8%±1.5% in the older group and 76.9%±1.4% in the younger group; there was no significant between-group difference, and the postoperative improvement of knee function was equal in the two groups.
  | Figure 3 Pre- and postoperative Japanese Orthopaedic Association score (total score). |
The JOA scores in category I “pain on walking” were 11.2±0.1 points at preoperation and 25.1±0.2 points at postoperation in the older group, and 13.1±0.1 points at preoperation and 28.5±0.1 points at postoperation in the younger group (Figure 4). In this category, the JOA scores in the younger group were significantly high both at pre- and postoperation, and postoperative significant improvement was observed in both groups.
  | Figure 4 Pre- and postoperative Japanese Orthopaedic Association score (category I, pain on walking). |
The JOA scores in category II “pain on ascending or descending stairs” were 4.3±0.1 points at preoperation and 18.8±0.2 points at postoperation in the older group, and 4.7±0.1 points at preoperation and 20.1±0.1 points at postoperation in the younger group (Figure 5). In this category, the JOA scores in the younger group were significantly high both at pre- and postoperation, and postoperative significant improvement was observed in both groups.
  | Figure 5 Pre- and postoperative Japanese Orthopaedic Association score (category II, pain on ascending or descending stairs). |
The JOA scores in category III “range of motion” were 27.6±0.2 points at preoperation and 28.9±0.1 points at postoperation in the older group, and 27.6±0.2 points at preoperation and 28.8±0.1 points at postoperation in the younger group (Figure 6). In this category, the JOA scores in both groups were not different both at pre- and postoperation, and significantly improved at postoperation.
  | Figure 6 Pre- and postoperative Japanese Orthopaedic Association score (category III, range of motion). |
The JOA scores in category IV “joint effusion” were 4.9±0.2 points at preoperation and 10.0±0 points at postoperation in the older group, and 5.5±0.2 points at preoperation and 10.0±0 points at postoperation in the younger group (Figure 7). In this category, the JOA score in the younger group was significantly high at preoperation, but not different at postoperation, and significantly improved at postoperation in both groups.
  | Figure 7 Pre- and postoperative Japanese Orthopaedic Association score (category IV, joint effusion). |
ROM
The ROM values (extension/flexion) were −8.2°±0.1°/130.9±0.5 at preoperation and −0.9°±0.1°/133.4±0.5 at postoperation in the older group, and −5.6°±0.2°/130.7±0.6 at preoperation and −0.3°±0.1°/133.3±0.5 at postoperation in the younger group (Figure 8). Both groups showed significant improvement postoperation. Between the older and younger groups, postoperative ROM of extension in the younger group was significantly superior, but that of flexion was not significantly different.
  | Figure 8 Pre- and postoperative ROM values. |
Postoperative days of hospital stay
The number of postoperative days of hospital stay in the older group (18.8±0.3 days) were significantly but only 2 days longer than that in the younger group (16.8±0.2 days).
Postoperative complications
Confusion, delayed wound healing, and acute heart failure were significantly more common in the older group. Conversely, the frequencies of pneumonia, cerebral infarction, peroneal nerve palsy, and bedsores were not significantly different between the groups (Table 3).
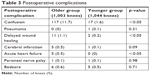  | Table 3 Postoperative complications |
Loosening of implants and PJI
The number of loosened implants was significantly higher in the younger group: five joints (0.5%) versus no joints in the older group. The number of PJIs did not differ significantly between the groups: five joints (0.5%) in the older group and two joints (0.2%) in the younger group.
Discussion
In the present series of patients, the JOA scores at both pre- and postoperation were significantly better in the younger group compared to the older group, but the rate of improvement in this score did not differ significantly between the groups. In categories I “pain on walking” and II “pain on ascending or descending stairs” of the JOA scores, the older group showed remarkable improvement. This result indicated that “relieving the pain on motion,” the main purpose of TKA, was achieved. Moreover, from the result of category IV “joint effusion,” TKA reduced joint effusion. Similarly, a significant postoperative improvement of ROM in extension and flexion was also observed in both groups. These results indicate that TKA for osteoarthritis is effective even in very old patients, as it is in younger patients.
In the present study, the period of hospital stay was much longer than previous study in Western country.11 In Japan, postoperative physical therapy is usually continued until the patients’ ability of walking becomes steady. Thus, the result of the present study accurately reflects the current status in Japan. The delayed postoperative rehabilitation schedule in old adult patients is due to their decreased physical strength and cognitive function, and postoperative confusion may prolong the period of hospital stay. However, in the present study, the number of postoperative days of hospital stay in the old adult patients was only 2 days longer than that of the younger group; a longer hospital stay was not required even among these patients ≥80 years old.
Although an improvement of knee function by TKA is expected, the risk of surgical complications is unavoidable,12 and thus efforts to prevent complications from the preoperative period onward as much as possible are required. We observed that confusion, delayed wound healing, and acute heart failure were significantly frequent in the older group; in particular, confusion occurred in >10% of the older-group patients. Conversely, the frequencies of pneumonia, cerebral infarction, peroneal nerve palsy, and bedsores were not significantly different between the older and younger groups. Although several precautions against confusion are advocated,13,14 a standard precaution has not been established in practice. Usually, confusion is a transient condition that occurs based on dementia, and it rarely influences the final prognosis; nevertheless, preoperative detailed information obtained from the patients and their family members about confusion as well as optimal perioperative patient care is required.
Acute heart failure is a severe, life-threatening complication. Belmont et al15 reported that the rates of postoperative cardiac complications in a primary TKA and total hip arthroplasty series was 0.33%, and they noted that, age ≥80 years, high blood pressure requiring medication, and past history of cardiac disease were the three most significant predictors. A careful preoperative evaluation of the risk of heart failure is, thus, mandatory, especially in older patients.
Meehan et al16 reported that short-term results (at 1 year) showed a 4.7-times higher risk of aseptic mechanical failure and a 1.8-times higher risk of PJI in younger patients (aged <50 years) compared with patients aged ≥65 years. In the present study, though the postoperative follow-up period was not very long (1–6 years), loosening of the implant was not observed in the older group. We speculate that the older patients are not as active as the younger patients, resulting in decreased mechanical stress on their implants. Although the difference was not significant, the number of patients who suffered a PJI was larger in our older patients compared to the younger patients. We suspect that reduced immune activity due to aging was the main cause of this result.
The limitations of this study are as follows. Possible confounding factors were not controlled, and evaluation items were not added because the study was a retrospective cohort study. The postoperative follow-up period (minimum 1 year) was not very long, in particular, the follow-up period (Figure 2) was significantly different between the younger and older groups. However, since the therapeutic effects of TKA usually reaches a plateau within 12 months, this limitation was thought to not influence the results concerning the JOA scores or ROM in the present study. The loosening of implants and the risk of PJI should be carefully observed over a longer period.
Conclusion
We evaluated the clinical outcomes of primary TKA for osteoarthritis in Japanese patients aged ≥80 years and compared them with those of patients aged <75 years. The rate of improvement in the JOA score and the ROM values were not significantly different between the two groups, and the number of postoperative days of hospital stay in the older patients was only 2 days longer than that of the younger patients. Concerning postoperative complications, the frequencies of pneumonia, cerebral infarction, peroneal nerve palsy, and bedsores were not significantly different between the groups, but confusion, delayed wound healing, and acute heart failure were significantly more frequent in the older group. Although no patient in the older group suffered loosening of implants, PJIs tended to be frequent in the older group. Even in these patients aged ≥80 years, our results demonstrate that careful preoperative screening and peri-/postoperative management will achieve safe and satisfactory outcomes of TKA in patients over 80 years old, similar to the outcomes of younger patients.
Disclosure
The authors report no conflicts of interest in this work.
References
Laskin RS. Total knee replacement in patients older than 85 years. Clin Orthop Relat Res. 1999;367:43–49. | ||
Belmar CJ, Barth P, Lonner JH, Lotke PA. Total knee arthroplasty in patients 90 years of age and older. J Arthroplasty. 1999;14(8):911–914. | ||
Joshi AB, Markovic L, Gill G. Knee arthroplasty in octogenarians: results at 10 years. J Arthroplasty. 2003;18(3):295–298. doi:10.1054/arth.2003.50063 | ||
Pagnano MW, McLamb LA, Trousdale RT. Total knee arthroplasty for patients 90 years of age and older. Clin Orthop Relat Res. 2004;418:179–183. doi:10.1097/00003086-200401000-00029 | ||
Kuo FC, Hsu CH, Chen WS, Wang JW. Total knee arthroplasty in carefully selected patients aged 80 years or older. J Orthop Surg Res. 2014;9:61. doi:10.1186/s13018-014-0061-z | ||
Abdel MP, Chalmers BP, Taunton MJ, et al. Intravenous versus topical tranexamic acid in total knee arthroplasty: both effective in a randomized clinical trial of 640 patients. J Bone Joint Surg Am. 2018;100(12):1023–1029. doi:10.2106/JBJS.17.00908 | ||
Tsukada S, Wakui M, Hoshino A. Postoperative epidural analgesia compared with intraoperative periarticular injection for pain control following total knee arthroplasty under spinal anesthesia a randomized controlled trial. J Bone Joint Surg Am. 2014;96(17):1433–1438. doi:10.2106/JBJS.M.01098 | ||
Kane RL, Saleh KJ, Wilt TJ, Bershadsky B. The functional outcome of total knee arthroplasty. J Bone Joint Surg Am. 2005;87(8):1719–1724. doi:10.2106/JBJS.D.02714 | ||
Koshino T. Japanese Orthopaedic Association knee scoring system. J Jpn Orthop Assoc. 1988;62:900–902. In Japanese. | ||
Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. | ||
Sutton JC 3rd, Antoniou J, Epure LM, Huk OL, Zukor DJ, Bergeron SG. Hospital discharge within 2 days following total hip or knee arthroplasty dose not increase major-complication and readmission rate. J Bone Joint Surg Am. 2016;98(17):1419–1428. doi:10.2106/JBJS.15.01109 | ||
Skou ST, Roos EM, Laursen MB, et al. A randomized, controlled trial of total knee replacement. N Engl J Med. 2015;373(17):1597–1606. doi:10.1056/NEJMoa1505467 | ||
Clayer M, Bruckner J. Occult hypoxia after femoral neck fracture and elective hip surgery. Clin Orthop Relat Res. 2000;370:265–271. doi:10.1097/00003086-200001000-00027 | ||
Larsen KA, Kelly SE, Stern TA, et al. Administration of olanzapine to prevent postoperative confusion in elderly joint-replacement patients: a randomized, controlled trial. Psychosomatics. 2010;51(5):409–418. doi:10.1176/appi.psy.51.5.409 | ||
Belmont PJ Jr, Goodman GP, Kusnezov NA, et al. Postoperative myocardial infarction and cardiac arrest following primary total knee and hip arthroplasty: rates, risk factors, and time of occurrence. J Bone Joint Surg Am. 2014;96(24):2025–2031. doi:10.2106/JBJS.N.00153 | ||
Meehan JP, Danielsen B, Kim SH, Jamali AA, White RH. Younger age is associated with a higher risk of early periprosthetic joint infection and aseptic mechanical failure after total knee arthroplasty. J Bone Joint Surg Am. 2014;96(7):529–535. doi:10.2106/JBJS.M.00545 |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.