Back to Journals » Local and Regional Anesthesia » Volume 13
Timing of Transversus Abdominis Plane Block and Postoperative Pain Management
Authors Escudero-Fung M, Lehman EB, Karamchandani K
Received 26 August 2020
Accepted for publication 14 October 2020
Published 3 November 2020 Volume 2020:13 Pages 185—193
DOI https://doi.org/10.2147/LRA.S278372
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Stefan Wirz
Maria Escudero-Fung,1 Erik B Lehman,2 Kunal Karamchandani1
1Department of Anesthesiology and Perioperative Medicine, Penn State Health Milton S. Hershey Medical Center, Penn State University College of Medicine, Hershey, PA, USA; 2Department of Public Health Sciences, Penn State University, Hershey, PA, USA
Correspondence: Kunal Karamchandani
Department of Anesthesiology and Perioperative Medicine, Penn State Health Milton S. Hershey Medical Center, Penn State University College of Medicine, Mail code H-187, 500 University Dr, Hershey, PA 17033, USA
Tel +1 717 5315457
Fax +1 717 5310797
Email [email protected]
Background: Transversus abdominis plane (TAP) blocks using liposomal bupivacaine can reduce postoperative pain and opioid consumption after surgery. The impact of timing of administration of such blocks has not been determined.
Materials and Methods: A retrospective cohort study of all adult patients that underwent colorectal procedures between January 2013 and October 2015 and received TAP blocks with liposomal bupivacaine at our institution was conducted. The primary outcomes were postoperative pain scores and opioid consumption. Secondary outcomes included postoperative use of non-opioid analgesics as well as total hospital cost of admission and postoperative hospital length of stay.
Results: A total of 287 patients were identified and included in the analysis. A total of 71 patients received blocks prior to induction of general anesthesia (pre-ind), 85 patients received blocks after induction of general anesthesia but prior to surgical incision (post-ind) and 131 patients received blocks after completion of surgery (post-op). No significant differences were observed in the postoperative pain scores (either in the first 4 hours or for the entire duration of hospital stay) or opioid consumption between the pre-ind and the post-ind groups. More ketorolac was used in the post-op group compared to the pre-ind group (or= 3.36, 95% CI (1.08, 10.43); p=0.03).
Conclusion: Our findings suggest that there seems to be no difference if tap blocks with liposomal bupivacaine are performed before or after induction of anesthesia. Patient preference as well as operating room efficiency should be considered when deciding on the timing of these blocks.G
Keywords: timing of transversus abdominis plane block, liposomal bupivacaine, postoperative pain, postoperative opioid consumption
Introduction
Systemic opioids are often used to manage pain after colorectal surgical procedures. This opioid use is often associated with adverse effects ranging from nausea, vomiting, constipation and ileus to respiratory depression.1 Since return of bowel function is an important determinant of postoperative recovery for patients undergoing colorectal surgery, postoperative ileus as a result of opioid administration might prolong recovery, increase hospital length of stay and affect overall morbidity.2 Opioid-related ileus is often dose dependent, and a decrease in overall dose of opioids may translate into clinically significant improvements in outcomes. Furthermore, the reduction in opioid consumption during hospitalization may prevent continued use of prescription opioids after discharge from the hospital and eventual development of chronic opioid use.3,4
To decrease postoperative opioid consumption and improve pain management in patients undergoing abdominal surgeries, transversus abdominis plane (TAP) blocks were introduced in 20015 and have been shown to be effective in reducing postoperative opioid consumption and postoperative hospital length of stay.6,7 The recent introduction of liposomal bupivacaine (LB) which provides a 9.8-fold increase in terminal half-life compared with standard bupivacaine can extend the duration of pain relief8 and has been shown to reduce postoperative opioid consumption in patients undergoing colorectal surgery.9 However, little is known about the timing of TAP block administration with LB and its impact on postoperative pain control. Since LB has a slow onset of action, the timing of administration may be important.10 While administration of the block prior to induction of anesthesia can potentially reduce opioid requirements, provide better pain control in the immediate postoperative period and improve operating room (OR) efficiency, it can cause significant patient discomfort. The aim of this study was to explore the relationship between timing of performance of TAP block with administration of LB prior to induction of general anesthesia, versus after induction of general anesthesia but prior to surgical incision, and after completion of surgery in patients undergoing open and minimally invasive colorectal surgery. We hypothesized that patients receiving TAP blocks with LB prior to induction of general anesthesia would have better postoperative pain control and require less opioid administration during the postoperative period.
Materials and Methods
Patient Selection
The study was approved by the Penn State Health Milton S. Hershey Medical Center Review Board (Study no. 00003230), and a waiver of informed consent was granted because of the retrospective nature of the study. Patient data confidentiality was maintained in accordance with the Declaration of Helsinki. We included all adult patients undergoing colorectal procedures under general anesthesia between January 2013 and October 2015, who received a TAP block with LB. We excluded patients with documented allergy to local anesthetics. Patient data was abstracted from a prospectively maintained registry by the Department of Anesthesiology and then cross-referenced with an institutional database maintained by the Division of Colon and Rectal surgery. Patient demographics, procedure-related details, patient reported pain scores, opioid requirements after surgery and other measures of postoperative pain control were obtained from electronic medical records. Based on the timing of TAP blocks, three patient groups were identified, those that received TAP blocks prior to induction of general anesthesia (Pre-Ind), after induction of general anesthesia but prior to surgical incision (Post-Ind), and after completion of surgery (Post-Op).
TAP Block
TAP blocks were performed by, or under the supervision of attending anesthesiologists who were part of acute pain management and regional anesthesia team and had significant experience in performing the blocks. Pre-Induction TAP blocks were performed in the block room prior to transport of patients to the OR. Post-Induction TAP blocks were performed in the OR after induction of general anesthesia and administration of muscle relaxant. Our standard practice during the study period was to perform TAP blocks using the lateral approach, and all patients in the study received bilateral TAP blocks using the lateral approach. Upon identification of the TAP, a 100-mm 22-gauge needle was inserted and advanced under real-time ultrasound guidance, and entry into the plane was confirmed with hydro-dissection. In patients in whom the blocks were performed prior to induction of anesthesia, 2 mL of 2% lidocaine was used to create a skin wheal at each entry point. All patients received 10 mL of LB diluted with 10 mL of saline (a total of 20 mL) (EXPAREL; Pacira Pharmaceuticals, Inc, Parsippany, NJ), as well as 5 mL of 0.25% conventional bupivacaine on each side. No patients undergoing TAP block received either epidural or spinal anesthesia and no restrictions were placed on subsequent opioid ordering or use. Nonsteroidal anti-inflammatory drugs (eg, ketorolac or ibuprofen) and acetaminophen were ordered on an as-needed basis for pain every 6 hours, with a limit of 5 days.
Outcomes
The primary outcome of this study was to compare postoperative patient-reported pain scores and total postoperative opioid consumption between the three groups. Pain scores were measured according to a standardized 11-point numeric rating scale.11 The first reported score, denoted by “0 hours,” reflects the median maximum pain score reported by the patient in the post-anesthesia care unit (PACU) and subsequent timing of scores was based on the time of discharge from the PACU. Nursing staff, who were blinded to the timing of the TAP block, performed the pain assessments approximately every 4 hours for the entire duration of the hospitalization. Postoperative median maximum pain scores at each 4-hour interval up to 72 hours after surgery were included in this analysis. Doses of analgesic medications were summed for the duration of the index hospitalization. Intravenous and oral opioids were converted into equivalent doses of morphine for comparison across all of the patients. Secondary outcomes included, postoperative use of non-opioid analgesics (acetaminophen, ketorolac and ibuprofen), postoperative length of stay and total hospital cost for the admission. Postoperative length of stay was defined from the day of surgery to the day of discharge from the hospital. Hospital costs were obtained from the institution’s cost-accounting database, which estimates cost using a ratio of the cost: charges method, and were adjusted to year 2015 dollars using the medical care of component of the consumer price index.
Statistical Analysis
Statistical analysis was performed to compare all outcomes across the three groups. Chi-square tests, Kruskal Wallis tests, and analysis of variance (ANOVA) were used to assess any differences between the study groups with respect to demographics and operative data (Table 1). Group comparisons, not listed in Table 1, were performed using pairwise two-sample t-tests for ANOVA adjusted for multiple comparisons using Tukey’s method or pairwise Wilcoxon Rank Sum tests for the Kruskal Wallis tests adjusted for multiple comparisons using the Bonferroni correction. Quantile regression of the median was used to compare postoperative pain scores between the three study groups, while adjusting for possible confounders like surgery duration, surgical approach and intraoperative opioid use. Opioid use, acetaminophen use, length of stay, and total cost were compared using the same quantile regression of the median but only adjusting for surgery duration and approach (Table 2). Since only a subset of patients in all three TAP block study groups received ketorolac and ibuprofen, a subgroup analyses was performed for these medications using logistic regression while adjusting for surgery duration and approach (Table 2). Group comparisons for quantile regression and for logistic regression were adjusted for multiple comparisons using the Bonferroni correction. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC).
 |
Table 1 Demographic and Operative Data by Groups |
 |
Table 2 Comparison of Postoperative Outcomes Between the Study Groups |
Results
Patient Demographics
In total, 287 patients were identified and included in the analysis, of which 71 patients belonged to the Pre-Ind group, 85 and 131 patients were part of the Post-Ind and Post-Op groups, respectively. The three study groups did not differ significantly with regard to age, sex, race/ethnicity, body mass index (BMI), American Society of Anesthesiology physical status (ASAPS) classification, and distribution of underlying diseases (Table 1). Similar proportions of patients underwent non-elective procedures, defined as those admitted to the hospital prior to the day of surgery. With regards to the types of procedures, the majority in each cohort were partial colectomies or proctectomies, followed by stoma-related procedures and total abdominal colectomies or proctocolectomies. The distribution of types of procedures did not differ significantly between groups (p=0.25), nor did the proportion of patients undergoing ileostomy or colostomy creation (Table 1). The duration of surgery and surgical approach (open vs laparoscopic/robotic) were significantly different between the three TAP timing groups (p=0.02 and p=0.01, respectively) and thus they were included as a covariate in all statistical analyses. The Post-Op group had a higher incidence of open surgery than the pre-induction and post-induction group (29.3% vs 11.8% and 13.9%, respectively). The median time difference between the performance of block and surgical incision in the Pre-Indand the Post-Ind group was significantly different (77.5 minutes vs 35.5 minutes, respectively, p<0.001).
Pain Scores
The median pain scores in the first 4 hours after surgery were comparable between the pre-induction and post-induction groups (0.78 vs 1.03, p=1.0), but patients in the postoperative group had significantly higher median pain scores in the first 4 hours as compared to the patients in the pre and post-induction groups. (0.78 vs 5.93 and 1.03 vs 5.93, respectively, p<0.001). Postoperative pain scores were not significantly different among the three groups for the remainder of the postoperative stay leading up to 72 hours and the three groups converged to have similar pain scores after the first 4-hour interval (Figure 1).
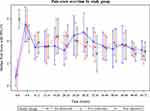 |
Figure 1 Pain scores over time in the study groups. |
Analgesic Requirements, Postoperative Length of Stay and Costs
The cumulative intravenous and oral opioid use as well as total acetaminophen consumption were not significantly different between the three groups (Table 2 and Figure 2). The median postoperative length of stay and median total cost for the index hospitalization also did not differ between the study groups (Table 2). However, ketorolac use was significantly higher in the Post-Op group. (OR= 3.36, 95% CI (1.08, 10.43); p=0.03).
 |
Figure 2 Consumption of opioids and acetaminophen between the study groups. |
Discussion
In this retrospective analysis of patients that underwent laparoscopic or open colorectal surgery and received TAP blocks with LB, we found that there was no difference in patient self-reported pain scores or cumulative postoperative oral and intravenous opioid consumption amongst those that received the blocks before or after induction of general anesthesia. Patients who received TAP blocks at the end of surgery, however, had higher pain scores in the immediate postoperative period as compared to those in whom they were performed prior to the start of surgery. Our findings suggest that TAP blocks with LB should be performed prior to the end of surgery but can be performed either before or after induction of general anesthesia.
Postoperative pain after colorectal surgery poses challenges for both the anesthesia and surgical teams and merits a comprehensive multimodal pain management strategy. TAP blocks have been used with good results in patients undergoing abdominal surgeries12–14 and are increasingly being used as part of the early recovery after surgery (ERAS) protocols with significant opioid-sparing effect.15 One of the biggest limitations of TAP blocks is the short duration of pain relief that is provided with the use of conventional local anesthetics. The use of continuous infusions via indwelling catheters can overcome this limitation but poses the added risk of infection as well as requiring specialized infusion pumps and monitoring. The recent approval of the use of LB in TAP blocks provides the flexibility of providing long-duration effect with a single injection. However, the timing of TAP blocks with LB is often debated amongst the providers.
There are several different approaches for administering ultrasound-guided TAP block. These include the lateral approach, covering nerves T10–12, providing lower abdominal wall analgesia, from the midline to the midclavicular line. The posterior approach, covering T9–12, providing analgesia at the anterior abdominal and lateral wall, and finally the subcostal approach, covering T6–9, providing analgesia at the upper abdomen. When comparing analgesic effects of TAP blocks, a meta-analysis showed that posterior approach appeared to produce longer-lasting analgesia compared to the lateral approach.16 In our study, we performed bilateral TAP blocks using the lateral approach which was the standard practice at our institution. Since most of the colorectal procedures involve a lower abdominal incision, this approach was adopted after discussions between the colorectal surgeons and the acute pain management and regional anesthesia team. Surgeon-performed TAP blocks under direct visualization are also a viable option, and are increasingly being used. Thus far, there is limited evidence suggesting that such surgeon-performed TAP blocks are better than ultrasound-guided TAP blocks for patients undergoing colorectal surgery.17 Although it is unlikely, that surgeon-performed TAP blocks would have changed our results, a randomized control trial comparing the two techniques in an appropriate sample of patients would be ideal.
In our analysis, we observed no difference with respect to postoperative pain control and opioid consumption between patients who received a TAP block prior to induction of anesthesia or after induction of anesthesia. There was a significant time difference between the performance of the block and surgical incision between these two groups, indicating appropriate separation within the groups. In order to avoid the effect of confounding variables such as duration of surgery, intraoperative opioid use and open vs laparoscopic surgery, we adjusted the outcomes for these variables. This is an important finding, since the performance of regional anesthesia blocks in awake patients versus those under general anesthesia has been a matter of debate, with no demonstratable benefit of either.18 While it is true that OR is the second most expensive part of surgical care19 and each minute of OR time can cost about $36 to $37,20 the OR time should be utilized judiciously. On the other hand, patient discomfort and the challenges of safe administration of regional blocks outside the OR, including the need for appropriate physical space, hemodynamic monitoring and nursing care should be factored into decision-making as well. We also did not find any difference in the total cost of hospitalization between these two groups, thus highlighting that the timing of TAP block administration can be tailored to patient needs and institutional logistics without affecting outcomes or costs.
The other major finding in our study is the reporting of higher pain scores in the immediate postoperative period by patients that received the TAP blocks at the conclusion of surgery versus those that received them prior to the surgical incision. This is consistent with prior reports of pre-incisional performance of TAP blocks being associated with reduced severity of acute pain, analgesic requirements and incidence of chronic pain as compared to blockade at the end of surgery.21 Preoperative administration of TAP block aligns with the clinical concept of preemptive analgesia, a strategy that involves introduction of analgesia before the introduction of noxious stimuli with the goal of preventing sensitization of the nervous system to subsequent stimuli that could amplify pain.22 Furthermore, for patients undergoing colorectal surgery, where there is potential for stoma creation, TAP block administration prior to surgery decreases the changes of accidental puncture of the exteriorized hollow viscous organ and contamination of the block site. Often times, there is a push by the surgical team to perform TAP blocks at the end of surgery to increase OR efficiency and also the decision on TAP blocks is delayed until the start of surgery. Our results and the published literature clearly indicate that the administration of pre-incision TAP blocks provide the best possible pain relief especially in the immediate postoperative period and may help decrease the time spent in PACU.
We did not observe any difference in the cumulative postoperative oral and intravenous opioid use or total acetaminophen consumption between the three groups but observed that patients in the Post-Op group required more ketorolac. Since the administration of opioids as well as adjunct pain medications was not guided by a standard protocol, variation in prescriber practices could partly account for these discordant findings. While studies have reported decrease in postoperative opioid consumption in patients who received preoperative versus postoperative TAP blocks, they did not use LB which tends to have a longer duration of action and could explain our results. We also found no significant differences with regards to length of stay between the three groups.
Our study has limitations. This was a single-center retrospective analysis at a tertiary care academic institution. Additionally, the performance of TAP blocks as well as surgical approach was not standardized. This type of variability is, however, not uncommon in large academic institutions. Although the three study groups were similar with respect to demographic data, a study with a matched numerical distribution of patients among the three groups would have been ideal. Operative data such as surgical approach (open vs laparoscopic/robotic) and median surgery duration were also significantly different among the groups. To limit their confounding effects, they were included in all analyses as covariates. The administration of intraoperative and postoperative narcotics, intraoperative steroids as well as adjunct pain medicines was based on provider preferences and might have affected the outcomes. Additionally, we did not exclude patients with pre-existing kidney disease, which would have affected the administration of NSAIDs and we also did not account for pre-operative opioid use, which could have impacted postoperative pain management. Lastly, when comparing hospital costs between our study groups, a time-driven activity-based costing analysis would have strengthened the analysis.23 However, this approach is still in its nascent stages with regards to anesthesia procedures and frankly we are limited in our resources to conduct such analysis.
Conclusion
In this single-center retrospective analysis of patients who received TAP blocks with LB for colorectal surgery, we found that there was no difference in patient-reported pain scores, opioid consumption or total hospitalization costs in patients that received these blocks before or after induction of anesthesia. Also, pre-incisional TAP blocks were associated with significantly lower patient reported pain scores in the immediate postoperative period. These findings suggest that there is definitive utility in performing TAP blocks with LB prior to the end of surgery, however, there seems to be no difference if they are performed before or after induction of anesthesia. Factors such as patient preference, anesthesia provider skills, operating room efficiency, and space for block administration can be used to determine the optimal pre-operative time for TAP block performance without affecting postoperative pain control or hospital costs.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
The authors have no sources of funding to declare for this manuscript.
Disclosure
The authors declare no conflicts of interest.
References
1. Oderda GM, Said Q, Evans RS, et al. Opioid-related adverse drug events in surgical hospitalizations: impact on costs and length of stay. Ann Pharmacother. 2007;41(3):400–406. doi:10.1345/aph.1H386
2. Tevis SE, Kennedy GD. Postoperative complications: looking forward to a safer future. Clin Colon Rectal Surg. 2016;29(3):246–252. doi:10.1055/s-0036-1584501
3. Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg 2017;152(6):e170504–e170504.
4. Hah JM, Bateman BT, Ratliff J, Curtin C, Sun E. Chronic opioid use after surgery: implications for perioperative management in the face of the opioid epidemic. Anesth Analg. 2017;125(5):1733–1740. doi:10.1213/ANE.0000000000002458
5. Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia. 2001;56(10):1024–1026.
6. Conaghan P, Maxwell-Armstrong C, Bedforth N, et al. Efficacy of transversus abdominis plane blocks in laparoscopic colorectal resections. Surg Endosc. 2010;24(10):2480–2484. doi:10.1007/s00464-010-0989-y
7. De Oliveira GS, Castro-Alves LJ, Nader A, Kendall MC, McCarthy RJ. Transversus abdominis plane block to ameliorate postoperative pain outcomes after laparoscopic surgery: a meta-analysis of randomized controlled trials. Anesth Analg. 2014;118(2):454–463. doi:10.1213/ANE.0000000000000066
8. Bergese SD, Ramamoorthy S, Patou G, Bramlett K, Gorfine SR, Candiotti KA. Efficacy profile of liposome bupivacaine, a novel formulation of bupivacaine for postsurgical analgesia. J Pain Res. 2012;5:107–116. doi:10.2147/JPR.S30861
9. Stokes AL, Adhikary SD, Quintili A, et al. Liposomal bupivacaine use in transversus abdominis plane blocks reduces pain and postoperative intravenous opioid requirement after colorectal surgery. Dis Colon Rectum. 2017;60(2):170–177. doi:10.1097/DCR.0000000000000747
10. Chahar P, Cummings KC. Liposomal bupivacaine: a review of a new bupivacaine formulation. J Pain Res. 2012;5:257–264.
11. Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994;58(3):387–392. doi:10.1016/0304-3959(94)90133-3
12. Carney J, McDonnell JG, Ochana A, Bhinder R, Laffey JG. The transversus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg. 2008;107(6):2056–2060. doi:10.1213/ane.0b013e3181871313
13. Keller DS, Ermlich BO, Schiltz N, et al. The effect of transversus abdominis plane blocks on postoperative pain in laparoscopic colorectal surgery: a prospective, randomized, double-blind trial. Dis Colon Rectum. 2014;57(11):1290–1297. doi:10.1097/DCR.0000000000000211
14. Sternlicht A, Shapiro M, Robelen G, Vellayappan U, Tuerk IA. Infiltration of liposome bupivacaine into the transversus abdominis plane for postsurgical analgesia in robotic laparoscopic prostatectomy: a pilot study. Local Reg Anesth. 2014;7:69–74.
15. Felling DR, Jackson MW, Ferraro J, et al. Liposomal bupivacaine transversus abdominis plane block versus epidural analgesia in a colon and rectal surgery enhanced recovery pathway: a randomized clinical trial. Dis Colon Rectum. 2018;61(10):1196–1204. doi:10.1097/DCR.0000000000001211
16. Abdallah FW, Laffey JG, Halpern SH, Brull R. Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: a meta-analysis. Br J Anaesth. 2013;111(5):721–735. doi:10.1093/bja/aet214
17. Wong DJ, Curran T, Poylin VY, Cataldo TE. Surgeon-delivered laparoscopic transversus abdominis plane blocks are non-inferior to anesthesia-delivered ultrasound-guided transversus abdominis plane blocks: a blinded, randomized non-inferiority trial. Surg Endosc. 2020;34(7):3011–3019. doi:10.1007/s00464-019-07097-y
18. Kessler P, Steinfeldt T, Gogarten W, et al. [Peripheral regional anesthesia in patients under general anesthesia: risk assessment with respect to parasthesia, injection pain and nerve damage]. Anaesthesist. 2013;62(6):483–488. German. doi:10.1007/s00101-013-2190-x
19. Stey AM, Brook RH, Needleman J, et al. Hospital costs by cost center of inpatient hospitalization for medicare patients undergoing major abdominal surgery. J Am Coll Surg. 2015;220(2):207–217 e211. doi:10.1016/j.jamcollsurg.2014.10.021
20. Childers CP, Maggard-Gibbons M. Understanding costs of care in the operating room. JAMA Surg. 2018;153(4):e176233. doi:10.1001/jamasurg.2017.6233
21. Amr YM, Amin SM. Comparative study between effect of pre- versus post-incisional transversus abdominis plane block on acute and chronic post-abdominal hysterectomy pain. Anesth Essays Res. 2011;5(1):77–82. doi:10.4103/0259-1162.84199
22. Kissin I, Weiskopf R. Preemptive analgesia. Anesthesiology. 2000;93(4):1138–1143. doi:10.1097/00000542-200010000-00040
23. Martin JA, Mayhew CR, Morris AJ, Bader AM, Tsai MH, Urman RD. Using time-driven activity-based costing as a key component of the value platform: a pilot analysis of colonoscopy, aortic valve replacement and carpal tunnel release procedures. J Clin Med Res. 2018;10(4):314–320. doi:10.14740/jocmr3350w
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
