Back to Journals » Clinical Interventions in Aging » Volume 16
Timed Up and Go: Reference Values for Community-Dwelling Older Adults with and without Arthritis and Non-Communicable Diseases: The Tromsø Study
Authors Svinøy OE , Hilde G, Bergland A, Strand BH
Received 27 November 2020
Accepted for publication 26 January 2021
Published 23 February 2021 Volume 2021:16 Pages 335—343
DOI https://doi.org/10.2147/CIA.S294512
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Nandu Goswami
Odd-Einar Svinøy,1 Gunvor Hilde,1 Astrid Bergland,1 Bjørn Heine Strand2
1Faculty of Health Sciences, Department of Physiotherapy, OsloMet – Oslo Metropolitan University, Oslo, Norway; 2Department of Chronic Diseases and Ageing, Norwegian Institute of Public Health, Oslo, Norway
Correspondence: Odd-Einar Svinøy
Faculty of Health Sciences, Department of Physiotherapy, OsloMet – Oslo Metropolitan University, PO Box 4, St. Olavs Plass, Oslo, 0130, Norway
Tel +4798443171
Email [email protected]
Purpose: The Timed Up and Go (TUG) test is used to assess a person’s mobility and balance. We aimed to provide updated reference values for TUG performance for the community-dwelling older population according to age and sex, and according to the presence of arthritis and non-communicable diseases (NCDs).
Participants and Methods: Cross-sectional data from the seventh wave (2015– 2016) of the population-based Norwegian Tromsø Study counting 5400 community-dwelling people (53% women), aged 60– 84 years were used. Reference values were presented as percentiles and means for men and women by age at five-year intervals.
Results: Median TUG score was stable during age 60– 65 years, and after age 65 years median TUG score increased significantly with age (increase by 0.14 sec per 1 year higher age in both men and women, p< 0.001). At the youngest ages (< 65 years), in both men and women, there were no differences in TUG performance for those with NCD or arthritis compared to those without these diseases. After age 65 however, those without these diseases performed significantly better (p< 0.05) in both men and women.
Conclusion: The present study provided percentile reference values for TUG performance in community-dwelling older adults in Norway by age and sex, and in subgroups of those having arthritis and NCDs. TUG scores increased with age, and performance was significantly poorer among participants with arthritis or NCDs after age 65 years. The findings may guide clinical interventions for individuals with mobility and balance disabilities.
Keywords: arthritis, geriatric assessment, non-communicable diseases, physical function, reference values, Timed Up and Go
Introduction
Physical function is a strong biomarker of health in older adults.1 Physical function declines with age, and some of the first signs of functional decline are reduced mobility, loss of muscular strength, and difficulties in performing daily activities,2 of which mobility is the most important factor for maintaining independence.3 The assessment of physical function can be useful for several purposes, such as to identify a decline in physical function, monitor the effect of exercise interventions, and provide specific information regarding physical domains, eg strength, balance and mobility. Performance-based outcome measures or standardized observer-rated observations are important tools for evaluating performance in clinical intervention practice and research studies as well as for identifying impairment.4,5 The identification of mobility impairments requires normative reference values to which an individual’s mobility score measurements can be compared.6
The Timed Up and Go (TUG) test is a simple, quick, and widely used clinical performance-based measure of mobility and balance.7 Poor TUG performance (high TUG score in seconds) may predict an increased length of hospital stay,8 mortality,9 low quality of life, low social participation,10 and the onset of difficulty with activities of daily living.11 A TUG-score of >20 seconds was identified as a cut-off point for sarcopenia by the European Working Group on Sarcopenia in Older People.12 The TUG test has shown acceptable psychometric properties and is considered an appropriate test for the general older adult population, including individuals with and without disabilities.13–18
TUG performance has further been studied in various populations with different pathological conditions, such as osteoarthritis19 and non-communicable diseases (NCDs).20–22 Osteoarthritis is associated with low physical performance23 and is considered a significant contributor to global disability and disability-adjusted life years.24 For patients undergoing total joint replacement due to late-stage hip or knee osteoarthritis, a high TUG score may predict delayed postoperative functional recovery for total hip25 and knee replacement.26 The four main types of NCDs are cancer, diabetes, chronic respiratory disease and cardiovascular disease. NCDs are associated with poorer performance on physical outcome measures.27–30 These four main types are the world’s leading cause of disabilities,31 contributing to a significant economic burden.32
Owing in part to its ease of use, association with fall risk and sensitivity, the TUG test is recommended by the Updated American Geriatrics Society/British Geriatrics Society Clinical Practice Guideline for Prevention of Falls in Older Persons.33 For the assessment of physical function in people with hip or knee arthritis, the TUG test is one of the five performance-based outcome measures recommended by the Osteoarthritis Research Society International.34
Four recent studies, in which the primary aim was to present reference values on TUG performance among older people, were from India,35 Malaysia,36 Ireland,37 and Spain.38 Of these studies, two were large-scale population-based studies.36,37 Additionally, three systematic reviews and meta-analyses presented reference values for the TUG test.39–41 To our knowledge, no former large-scale population-based study has presented percentile reference values on TUG performance for NCDs and arthritis as disease-specific subgroups.
The aim is to provide updated normative reference values on the TUG test, stratified by age, sex, and disease status, using data from the large population-based Norwegian Tromsø study. Given that TUG performance varies with age, sex, disease, and nationality, this paper will be an important addition to the current body of knowledge on reference values for TUG performance for the community-dwelling older population aged 60 years and older.
Participants and Methods
Study Population
The data used in this study stemmed from the seventh wave of the Norwegian Tromsø study conducted during 2015–2016. The Tromsø study is an observational multipurpose population-based health examination study, with seven study waves, initiated in 1974, 1979, 1986, 1994, 2001, 2008, and 2015.42 All those aged 40 years and above were invited to phase-one (n=32,591). Among the 21,083 that accepted to participate, a random sub-set of 40% were invited to a phase two examination for a more thorough clinical examination, including physical function testing. Some participants were invited to all sub-tests in phase two, while most participated in some of the tests. In all, 5444 were invited for TUG-testing and 5408 of those participated. Eight participants were either missing or unable to participate in testing due to error in testing (n=3), TUG-test >40 seconds (n=1) or being unable to perform the test (n=4). Thus, we got complete TUG-data for 5400 community-dwelling participants aged 60–84 years.
TUG Testing Procedure
Testing was performed by trained physiotherapists and nurses using the original protocol.7 During testing, the participant was seated in a chair that was 43 cm high with armrests and asked to stand up from the chair at the command “Go” (using the chair’s armrests if they preferred), walk 3 meters at their regular pace, turn, walk back again, and sit down. The participant’s TUG score in seconds was timed with a stopwatch from the command “Go” to when the participant was seated again. A high TUG score indicates poorer physical performance.
Covariates
Self-reported educational level was categorized in three groups as basic (~9 years), middle (~10–12 years), or tertiary (~13+ years). Height (cm) and weight (kg) were measured by trained personnel, and body mass index (BMI) was calculated as weight in kilos divided by squared height in meters (kg/m2). Additionally, the participants were categorized into three subgroups based on the self-report of the presence of (1) at least one of the four main NCDs, (2) arthritis, or (3) no NCD or arthritis. The four main NCDs (n=1799) were comprised of cardiovascular diseases (n=784), cancers (n=715), chronic pulmonary diseases (n=267) and diabetes (n=416).
Representativeness by Educational Level
Official registry data on educational level in Norway and in the Tromsø municipality by December 31, 2015, by age and sex43 were compared to the prevalence of self-reported tertiary education in the study population.
Statistical Methods
Percentiles for TUG scores (5th, 10th, 25th, 50th, 75th, 90th, and 95th percentiles) were estimated using quantile regression, while the mean and standard deviation (SD) were estimated using linear regression. In both regression settings, age was included as a restricted cubic spline with four knots at a default knot location (ie 60, 66, 71, and 80 years). Models were run separately for men and women. SD was estimated from the regression model and was the standard error of the forecasted value. This corresponded to the SD and is a measure of the variation of the actual values. Sex-specific reference values at specific ages at five-year intervals (ie 60, 65, 70, 75, and 80 years) were then predicted post hoc from the fitted regression models. Stata/SE 15.0 for Windows (StataCorp LLC, 4905 Lakeway Drive, College Station, TX, 77,845, USA) was used for all statistical analyses.
Ethics Approval and Consent to Participate
This research was conducted in accordance with the Declaration of Helsinki. The Regional Committee for Medical and Health Research Ethics, REC South East, approved the study (2016/389). Written informed consent was obtained from all participants in the Tromsø Study.
Results
Of the 5400 participants who had complete TUG data, 2904 (53%) were women. The mean age was 68.8 (SD 6.1) years for men and 69.0 (SD 6.1) years for women (Table 1). Men had significantly (p<0.01) higher BMI than women; 27.7 kg/m2 vs 27.1 kg/m2. Men had a significantly higher level of education compared to women. Women had a significantly higher prevalence of arthritis compared to men (38% vs 18%), while men had the highest prevalence of NCD (39% vs 28%). Among men and women, 51% and 46%, respectively, had neither arthritis nor NCD.
 |
Table 1 Background Characteristics |
Median TUG score was stable during age 60–64 years, but from the age 65 years and onwards the median TUG score significantly increased with age in both men and women (Figure 1). In Table 2 we present TUG scores at exact ages based on quantile regression, where TUG increased by 0.14 sec per 1 year higher age in both men and women (p<0.001) (Table 2). In men, median (50th percentile) TUG score for 60-year-olds was 8.0 seconds, for 70-year-olds it was 8.4 seconds, and for 80-year-olds it was 10.2 seconds. The corresponding TUG scores for women were 8.0 seconds for 60-year olds, which was from the same as for men (p>0.05), 8.7 seconds for 70-year olds, significantly differing from men (p<0.01), and 10.3 seconds for 80-year olds where there were no significant differences between men and women (p>0.05). For 60-year-old men, the 5th percentile of TUG score/performance was 6.0 seconds, whereas the 95th percentile was 11.0 seconds. Corresponding numbers in women were 6.0 and 10.0 seconds, respectively. The variations in TUG scores were higher at older ages; in 84-year-old men, the 5th percentile was 7.0 seconds, and the 95th percentile was 17.1 seconds. In women TUG scores for the corresponding percentiles were 8.2 and 18.6 seconds, respectively (Table 2).
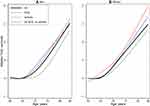 |
Figure 1 Timed Up and Go in seconds, by sex and diagnosis. (A) Men, (B) Women. Abbreviations: NCD, non-communicable diseases; TUG, Timed Up and Go. |
 |
Table 2 Timed Up and Go (TUG) Reference Values in Seconds, at Exact Ages, Disease Groups and Sex |
At the youngest ages, until about age 65 years, in both men and women, there were no differences in TUG performance for those with NCD or arthritis compared to those without these diseases (Table 2, Figure 1). After age 65 years, however, those without these diseases performed significantly better than those with these diseases (p<0.05) in both men and women. For all three groups, TUG performance score increased with age, especially after the age of 65 years. However, the onset of this increase in TUG performance score occurred at a later age among men without arthritis or NCDs compared to those with such diseases (Figure 1).
The study population was slightly biased regarding education, with a higher prevalence of higher education compared to the general Norwegian population and the population in the municipality of Tromsø; The prevalence of tertiary education (~13+ years) in men aged 70- to 74-years was 27% in the general Norwegian population and likewise in Tromsø,43 but it was somewhat higher (39%) in the Tromsø study population. The corresponding numbers for women were 20%, 22%, and 26%, respectively. For the age group 75–79 years, the population-based prevalence of tertiary education among men was 23% (in the general Norwegian population), 26% in Tromsø, and 35% in the Tromsø study population, and among women, the corresponding prevalence was 16%, 17%, and 22%, respectively.
Discussion
The present study provides updated reference values for TUG scores in community-dwelling older adults in Norway, by age, sex, and disease status. TUG scores increased with age, and the increase was especially prominent after 65 years of age. Participants with arthritis or NCDs performed significantly poorer on the TUG test after age 65 years than did participants without these diseases. To the best of our knowledge, this is the first large-scale population-based study providing sex- and age-specific percentile reference values for TUG among participants with arthritis or NCDs.
Increasing age is associated with a decline in physical performance.2,5 Our results show poorer TUG performance with increased age and are consistent with previous population-based studies.35–38 In this context, it is important to highlight the prominent increase in TUG score after the age of 65. The present study demonstrated a significant trend toward age-related functional decline. Between the ages 70 and 75 years, women had poorer TUG performance than men at the same ages. This underscores the importance of regular physical activity interventions that may improve, or at least delay the loss of, physical function and mobility among older adults.44,45
The participants in our study performed better on the TUG test than participants in a comparable large-scale population-based study from Malaysia that included 2084 community-dwelling older adults aged 60–90 years.36 For comparison, the mean TUG score for Malaysian men and women in the age group of 60–64 years was 10.4 seconds; for the corresponding mean score in our study, it was 8.2 seconds in men and 8.1 seconds in women. For the age group of 75–79 years, those in the Malaysian study scored 12.6 seconds, whereas men in our study scored 10.0 seconds and women 10.5 seconds.
This difference may be explained by country-specific differences, such as socioeconomic status.46 Research has shown that socioeconomic status is associated with later-life physical performance.47–49 In contrast with Malaysia, Norway is characterized by a high level of welfare, as it has one of the highest levels of income per capita in the world, and 34% of the population have tertiary education (ie a university or college).50
Another large-scale study using the original protocol of Podsiadlo and Richardson was conducted in Ireland.37 TUG performance in Ireland and Norway seems similar, but a direct comparison is difficult as participants in the study from Ireland were stratified by height. In a Spanish study38 presenting the TUG scores of 308 individuals aged 71–99 years, the participants scored somewhat better in the lower age-specific percentiles (ie the 5th and 10th percentiles) compared to the participants in our study; the opposite was the case for those in the 50th percentile and likewise for those in the upper percentiles (ie 90th and 95th percentile). However, a direct comparison cannot be made as the Spanish study used a different procedure, asking participants to perform the test “as quickly as possible”.
Likewise, comparing population-based reference values from a study conducted in India35 is not feasible because a different testing procedure was used, with participants being asked to conduct the test, “as quickly they feel safe and comfortable.” In former meta-analyses,39–41 it is problematic to compare meta-reference values when they are based on aggregated data from primary studies having differences in test instructions and testing procedures. An added limitation is that these reviews relied mostly on small studies.
Updated reference values for performance-based physical function are important, as they characterize what is normal in a defined population at a specific point or period.51 For clinicians, such reference values are important because a clinical test score without a reference value is difficult to interpret. Percentiles indicate a person’s performance relative to the expected level for their age, sex, and other characteristics.52 In research, we rely on reference values to evaluate individual or group scores to observe how the scores compare to the group’s average values for age, country, sex, or other characteristics.53 Reference values give meaning to a clinical test score and enable clinicians to create treatment goals or to tailor treatment for individual patients.51 In addition to reference values for the general population, it may also be of interest to obtain reference values for subgroups in the population. For example, it is valuable to see how groups with highly prevalent diseases score in comparison to the general population.
Low physical performance is associated with arthritis23 and NCD27–30 which is in line with our findings in the older age groups (>65 years), as well as the findings of Ibrahim et al. In contrast to Ibrahim et al, we presented age- and sex-specific percentile reference values for the disease groups.
Strengths and Limitations
This study is, to the authors’ knowledge, among the largest of its kind in which the TUG testing procedure is consistent with the original protocol of Podsiadlo and Richardson which represents the most widely used version of the TUG,54 and used in recent large-scale population-based studies.36,37 The large number of participants in this study is a strength as it enables us to establish reference values for subgroups of the general population by age and sex as well as by the presence of arthritis or NCD. Another strength of this study is that the TUG testing was performed by trained health professionals. In addition, an administration manual was provided to help ensure test standardization. Furthermore, all tests were performed at the same location, increasing the validity of the reference values. This is important, as TUG scores across different studies can be difficult to compare due to procedural differences. Some researchers55,56 have raised concerns about the comparability of TUG scores if the testing procedure was not performed in the same manner, which might make the pooling of data difficult.
The study does, however, have some limitations. Considering that the participants in this study were invited for testing, the sample is likely skewed because there is a chance that well-functioning participants were more prone to participate. Additional evidence of this is that the educational level was higher in the study population than it was in Tromsø at large, and in the general population in Norway. Furthermore, participants in multiple Tromsø study waves had lower mortality compared to individuals participating only once,42 making it plausible that the overall health and function of participating individuals was higher than that of non-participating individuals. Thus, the reference values are applicable for community-dwelling participants able and willing to participate and undertake a complete assessment. Also, the participants’ disease status was self-reported and we had no objective test verifying whether arthritis or NCD was present or not, which might place some respondents in the wrong disease groups and thereby underestimate or overestimate the true TUG difference between the disease-free population and the various disease groups (arthritis or NCD). Participants over the age of 84 did not participate in physical testing, thus we no data on the oldest age groups. We do not have information about the participants’ use of medication. Studies show that drug interactions may alter gait speed in the elderly population.57 Lastly, we did not have data specifying the severity of the arthritis nor the joint affected. A clinician should be aware of this as hand arthritis, for example, would affect TUG scores less than would hip or knee arthritis.
Conclusion
The present study provides TUG reference values in community-dwelling older adults in Norway by age, sex, and disease status. TUG performance was poorer with increased age, and at higher ages, performance was poorer among participants with arthritis or NCDs. Our data provide information about the impact of the diseases and could guide decisions regarding interventions.
Data Sharing Statement
The data supporting the conclusions of this article are available at www.tromsoundersokelsen.no.
Acknowledgments
We are grateful to the Tromsø research group for conducting this health assessment study and to the participants of the study.
Author Contributions
OES: preparation of manuscript and analysis and interpretation of data. GH: preparation of manuscript and interpretation of data. AB: study design, acquisition of data and subjects, and preparation of the manuscript. BHS: study concept and design, acquisition of subjects and data, analysis and interpretation of data, and preparation of the manuscript. All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Vestergaard S, Patel KV, Bandinelli S, Ferrucci L, Guralnik JM. Characteristics of 400-meter walk test performance and subsequent mortality in older adults. Rejuvenation Res. 2009;12(3):177–184. doi:10.1089/rej.2009.0853
2. den Ouden ME, Schuurmans MJ, Arts IE, van der Schouw YT. Physical performance characteristics related to disability in older persons: a systematic review. Maturitas. 2011;69(3):208–219. doi:10.1016/j.maturitas.2011.04.008
3. Miller RR, Roubenoff R. Emerging interventions for elderly patients-the promise of regenerative medicine. Clin Pharmacol Ther. 2019;105(1):53–60. doi:10.1002/cpt.1272
4. Stratford PW, Kennedy DM. Performance measures were necessary to obtain a complete picture of osteoarthritic patients. J Clin Epidemiol. 2006;59(2):160–167. doi:10.1016/j.jclinepi.2005.07.012
5. Tangen GG, Robinson HS. Measuring physical performance in highly active older adults: associations with age and gender? Aging Clin Exp Res. 2020;32(2):229–237. doi:10.1007/s40520-019-01190-x
6. Mitrushina M, Boone K, Razani J, D’Elia L. Handbook of Normative Data for Neuropsychological Assessment. Oxford University Press; 2005.
7. Podsiadlo D, Richardson S. The timed “up & go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. doi:10.1111/j.1532-5415.1991.tb01616.x
8. Poitras S, Au K, Wood K, Dervin G, Beaulé PE. Predicting hospital length of stay and short-term function after hip or knee arthroplasty: are both performance and comorbidity measures useful? Int Orthop. 2018;42(10):2295–2300. doi:10.1007/s00264-018-3833-y
9. Bergland A, Jørgensen L, Emaus N, Strand BH. Mobility as a predictor of all-cause mortality in older men and women: 11.8 year follow-up in the Tromsø study. BMC Health Serv Res. 2017;17:1–7
10. Ekström H, Dahlin-Ivanoff S, Elmståhl S. Effects of walking speed and results of timed get-up-and-go tests on quality of life and social participation in elderly individuals with a history of osteoporosis-related fractures. J Aging Health. 2011;23(8):1379–1399. doi:10.1177/0898264311418504
11. Wennie Huang WN, Perera S, VanSwearingen J, Studenski S. Performance measures predict onset of activity of daily living difficulty in community-dwelling older adults. J Am Geriatr Soc. 2010;58(5):844–852. doi:10.1111/j.1532-5415.2010.02820.x
12. Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31. doi:10.1093/ageing/afy169
13. Botolfsen P, Helbostad JL. Reliabilitet av den norske versjonen av Timed Up and Go (TUG). Fysioterapeuten. 2010;5:Fag 2–10.
14. Albarrati A, Nazer R. Utility of timed up and go in outpatient cardiology clinics. Rehabil Nurs. 2020;45(1):39–44. doi:10.1097/rnj.0000000000000163
15. Christopher A, Kraft E, Olenick H, Kiesling R, Doty A. The reliability and validity of the timed up and go as a clinical tool in individuals with and without disabilities across a lifespan: a systematic review. Disabil Rehabil. 2019;1–15. doi:10.1080/09638288.2019.1682066
16. Ozcan Kahraman B, Ozsoy I, Akdeniz B, et al. Test-retest reliability and validity of the timed up and go test and 30-second sit to stand test in patients with pulmonary hypertension. Int J Cardiol. 2020;304:159–163. doi:10.1016/j.ijcard.2020.01.028
17. Rydwik E, Bergland A, Forsén L, Frändin K. Psychometric properties of timed up and go in elderly people: a systematic review. Phys Occup Ther Geriatr. 2011;29(2):102–125. doi:10.3109/02703181.2011.564725
18. Yuksel E, Unver B, Kalkan S, Karatosun V. Reliability and minimal detectable change of the 2-minute walk test and timed up and go test in patients with total hip arthroplasty. Hip Int. 2020;1120700019888614. doi:10.1177/1120700019888614
19. Zasadzka E, Borowicz AM, Roszak M, Pawlaczyk M. Assessment of the risk of falling with the use of timed up and go test in the elderly with lower extremity osteoarthritis. Clin Interv Aging. 2015;10:1289–1298. doi:10.2147/CIA.S86001
20. Guerrero N, Bunout D, Hirsch S, et al. Premature loss of muscle mass and function in type 2 diabetes. Diabetes Res Clin Pract. 2016;117:32–38. doi:10.1016/j.diabres.2016.04.011
21. Morishita S, Mitobe Y, Tsubaki A, et al. Differences in balance function between cancer survivors and healthy subjects: a Pilot Study. Integr Cancer Ther. 2018;17(4):1144–1149. doi:10.1177/1534735418790387
22. Overcash J, Ford N, Erdeljac HP, et al. Comprehensive geriatric assessment in oncology: best practices in caring for older patients. J Adv Pract Oncol. 2018;9(6):640–644.
23. Edwards MH, van der Pas S, Denkinger MD, et al. Relationships between physical performance and knee and hip osteoarthritis: findings from the European Project on Osteoarthritis (EPOSA). Age Ageing. 2014;43(6):806–813. doi:10.1093/ageing/afu068
24. Kyu HH, Abate D, Abate KH, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1859–1922.
25. Elings J, van der Sluis G, Goldbohm RA, et al. Development of a risk stratification model for delayed inpatient recovery of physical activities in patients undergoing total hip replacement. J Orthop Sports Phys Ther. 2016;46(3):135–143. doi:10.2519/jospt.2016.6124
26. van der Sluis G, Goldbohm RA, Elings JE, et al. Pre-operative functional mobility as an independent determinant of inpatient functional recovery after total knee arthroplasty during three periods that coincided with changes in clinical pathways. Bone Joint J. 2017;99-b(2):211–217. doi:10.1302/0301-620X.99B2.BJJ-2016-0508.R1
27. Al Haddad MA, John M, Hussain S, Bolton CE. Role of the timed up and go test in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev. 2016;36(1):49–55. doi:10.1097/HCR.0000000000000143
28. Moreira Bde S, Sampaio RF, Furtado SR, Dias RC, Kirkwood RN. The relationship between diabetes mellitus, geriatric syndromes, physical function, and gait: a review of the literature. Curr Diabetes Rev. 2016;12(3):240–251. doi:10.2174/1573399811666150615142746
29. Son KY, Shin DW, Lee JE, Kim SH, Yun JM, Cho B. Association of timed up and go test outcomes with future incidence of cardiovascular disease and mortality in adults aged 66 years: Korean national representative longitudinal study over 5.7 years. BMC Geriatr. 2020;20(1):111. doi:10.1186/s12877-020-01509-8
30. Verweij NM, Schiphorst AH, Pronk A, van den Bos F, Hamaker ME. Physical performance measures for predicting outcome in cancer patients: a systematic review. Acta Oncol. 2016;55(12):1386–1391. doi:10.1080/0284186X.2016.1219047
31. IHME. Global Burden of Disease Study 2016 (GBD 2016) Results. Seattle, United States: Institute for Health Metrics and Evaluation; 2016.
32. Chen S, Kuhn M, Prettner K, Bloom DE, Husain MJ. The macroeconomic burden of noncommunicable diseases in the United States: estimates and projections. PLoS One. 2018;13(11):e0206702. doi:10.1371/journal.pone.0206702
33. American Geriatrics Society [AGS], British Geriactrics Society [BGS], American Academy of Orthopaedic Surgeons Panel on Falls Prevention [AAOS]. Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of orthopaedic surgeons panel on falls prevention. J Am Geriatr Soc. 2001;49(5):664–672.
34. Dobson F, Hinman RS, Roos EM, et al. OARSI recommended performance-based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthr Cartil. 2013;21(8):1042–1052. doi:10.1016/j.joca.2013.05.002
35. Khant N, Dani VB, Patel P, Rathod R. Establishing the reference value for “timed up-and-go” test in healthy adults of Gujarat, India. J Educ Health Promot. 2018;7(1):62. doi:10.4103/jehp.jehp_12_18
36. Ibrahim A, Singh DKA, Shahar S, Ginsberg SD. ‘Timed up and go’ test: age, gender and cognitive impairment stratified normative values of older adults. PLoS One. 2017;12(10):e0185641. doi:10.1371/journal.pone.0185641
37. Kenny RA, Coen RF, Frewen J, Donoghue OA, Cronin H, Savva GM. Normative values of cognitive and physical function in older adults: findings from the Irish Longitudinal Study on Ageing. J Am Geriatr Soc. 2013;61(Suppl 2):S279–S290. doi:10.1111/jgs.12195
38. Pondal M, Del Ser T. Normative data and determinants for the timed “up and go” test in a population-based sample of elderly individuals without gait disturbances. J Geriatr Phys Ther. 2008;31(2):57–63. doi:10.1519/00139143-200831020-00004
39. Bohannon RW. Reference values for the timed up and go test: a descriptive meta-analysis. J Geriatr Phys Ther. 2006;29(2):64–68. doi:10.1519/00139143-200608000-00004
40. Kamide N, Takahashi K, Shiba Y. Reference values for the timed up and go test in healthy Japanese elderly people: determination using the methodology of meta-analysis. Geriatr Gerontol Int. 2011;11(4):445–451. doi:10.1111/j.1447-0594.2011.00704.x
41. Long J, Cai T, Huang X, Zhou Y, Kuang J, Wu L. Reference value for the TUGT in healthy older people: a systematic review and meta-analysis. Geriatric Nurs. 2019;41(3):325–330. doi:10.1016/j.gerinurse.2019.11.012
42. Jacobsen BK, Eggen AE, Mathiesen EB, Wilsgaard T, Njølstad I. Cohort profile: the Tromso Study. Int J Epidemiol. 2012;41(4):961–967. doi:10.1093/ije/dyr049
43. Microdata. Official Registry Data on Education Level in Tromsø at December 31, 2015. 2015.
44. Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020–2028. doi:10.1001/jama.2018.14854
45. Dipietro L, Campbell WW, Buchner DM, et al. Physical activity, injurious falls, and physical function in aging: an umbrella review. Med Sci Sports Exerc. 2019;51(6):1303–1313. doi:10.1249/MSS.0000000000001942
46. Sousa AC, Guerra RO, Thanh Tu M, Phillips SP, Guralnik JM, Zunzunegui M-V. Lifecourse adversity and physical performance across countries among men and women aged 65–74. PLoS One. 2014;9(8):e102299. doi:10.1371/journal.pone.0102299
47. Noppert GA, Brown CS, Chanti-Ketterl M, et al. The impact of multiple dimensions of socioeconomic status on physical functioning across the life course. Gerontol Geriatr Med. 2018;4:2333721418794021.
48. Hurst L, Stafford M, Cooper R, Hardy R, Richards M, Kuh D. Lifetime socioeconomic inequalities in physical and cognitive aging. Am J Public Health. 2013;103(9):1641–1648. doi:10.2105/AJPH.2013.301240
49. Haas S, Krueger P, Rohlfsen L. Race/ethnic and nativity disparities in later life physical performance: the role of health and socioeconomic status over the life course. J Gerontol B Psychol Sci Soc Sci. 2012;67B(2):238–248. doi:10.1093/geronb/gbr155
50. Statistics Norway [SSB]. Educational attainment of the population. 2020. Available from: https://www.ssb.no/en/utniv.
51. O’Connor PJ. Normative data: their definition, interpretation, and importance for primary care physicians. Fam Med. 1990;22(4):307–311.
52. Fawcett A. Principle of Assessment and Outcome Measure for Occupational Therapists and Physiotherapists. Hoboken: Wiley; 2009.
53. Jacobsen EL, Bye A, Aass N, et al. Norwegian reference values for the short-form health survey 36: development over time. Qual Life Res. 2018;27(5):1201–1212. doi:10.1007/s11136-017-1684-4
54. Schoene D, Wu SM-S, Mikolaizak AS, et al. Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: systematic review and meta-analysis. J Am Geriatr Soc. 2013;61(2):202–208. doi:10.1111/jgs.12106
55. Bergmann JHM, Alexiou C, Smith ICH. Procedural differences directly affect timed up and go times. J Am Geriatr Soc. 2009;57(11):2168–2169. doi:10.1111/j.1532-5415.2009.02547.x
56. Siggeirsdottir K, Jonsson BY, Jonsson H
57. Naples JG, Marcum ZA, Perera S, et al. Impact of drug–drug and drug–disease interactions on gait speed in community-dwelling older adults. Drugs Aging. 2016;33(6):411–418. doi:10.1007/s40266-016-0373-2
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
