Back to Journals » Journal of Multidisciplinary Healthcare » Volume 15
Time to Death and Predictors Among Neonates with Esophageal Atresia in Ethiopia
Authors Misganaw NM , Sebsbie G, Adimasu M , Getaneh FB , Arage G, GebreEyesus FA , Bayih WA , Chanie ES , Bantie B , Kerebeh G, Birhanu D , Jemere T , Mengist A , Kassaw A
Received 15 March 2022
Accepted for publication 20 May 2022
Published 30 May 2022 Volume 2022:15 Pages 1225—1235
DOI https://doi.org/10.2147/JMDH.S366470
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Natnael Moges Misganaw,1 Girum Sebsbie,2 Mekonen Adimasu,2 Fekadeselassie Belege Getaneh,3 Getachew Arage,1 Fisha Alebel GebreEyesus,4 Wubet Alebachew Bayih,1 Ermias Sisay Chanie,1 Berihun Bantie,5 Gashaw Kerebeh,1 Dires Birhanu,6 Tadeg Jemere,7 Anteneh Mengist,8 Amare Kassaw1
1Debre Tabor University, College of Health Science, Department of Paediatrics and Child Health Nursing, Debre Tabor, Ethiopia; 2Addis Ababa University, College of Health Science, School of Nursing and Midwifery, Department of Paediatrics and Child Health Nursing, Addis Ababa, Ethiopia; 3Wollo University, College of Health Science, School of Nursing and Midwifery, Department of Paediatrics and Child Health Nursing, Dessie, Ethiopia; 4Wolkite University, College of Medicine and Health Science, Department of Paediatrics and Child Health Nursing, Wolkite, Ethiopia; 5Debre Tabor University, College of Health Science, Department of Adult Health Nursing, Debre Tabor, Ethiopia; 6Dilla University, College of Health Science, Department of Paediatrics and Child Health Nursing, Dilla, Ethiopia; 7Debre Tabor University, College of Health Science, Department of Biomedical Science, Debre Tabor, Ethiopia; 8Debre Tabor University, College of Health Science, Department of Public Health, Debre Tabor, Ethiopia
Correspondence: Natnael Moges Misganaw, Email [email protected]
Background: Esophageal atresia is an upper gastrointestinal tract developmental abnormality in which the upper and lower esophagus do not connect. Esophageal atresia has a higher incidence of death in sub-Saharan Africa, ranging from 30% to 80%. In Ethiopia, infants with esophageal atresia had a higher mortality rate. The assessment of time to death and predictors of esophageal atresia can help to reduce newborn mortality.
Objective: This study was aimed to investigate the time to death and predictors of neonates with esophageal atresia admitted to Tikur Anbessa Specialized Hospital, Ethiopia.
Methods: An institutional-based retrospective follow-up study was conducted among 225 neonates diagnosed with esophageal atresia. The median survival time, Kaplan–Meier failure estimation curve, and Log rank test were computed. Bivariable and multivariable Cox regression hazards models were fitted to identify the predictors of time to death. Hazard ratio with a 95% confidence interval was calculated and p-values < 0.05 were considered statistically significant.
Results: In the study, the incidence density rate of neonates diagnosed with esophageal atresia was 5.5 (95% CI, 4.7– 6.4) per 100-neonates day. The median time to death was 11 days (95% confidence interval (CI), 8.92– 13.08). Birth weight < 2500 g (adjusted hazard ratio (AHR)=1.49, 95% CI, 1.02 − 2.21), having sepsis (AHR=1.67,95% CI, 1.15– 2.44), being malnourished (AHR = 1.61, 95% CI, 1.03 − 2.58), esophageal atretic neonates without surgery (AHR = 3.72, 95% CI, 1.34– 10.38), diagnosis time at > 48 hours of admission (AHR = 1.48, 95% CI, 1.01– 2.15) and being dehydrated (AHR = 2.38, 95% CI, 1.63– 3.46) were significant predictors of time to death among esophageal atretic neonates.
Conclusion: The findings in this study highlighted the necessity of early diagnosis, proper comorbidity treatment, and timely surgical intervention to reduce infant deaths due to esophageal atresia.
Keywords: esophageal atresia, time to death, Ethiopia
Introduction
Esophageal atresia (EA) is a developmental defect of the upper gastrointestinal tract in which the continuity between the upper and lower esophagus is lost. EA can occur with or without the tracheoesophageal fistula (TEF), an abnormal communication between the trachea and the esophagus.1
The incidence of EA is found to be 1.27 to 4.55 per 10,000 live births.2,3 From the total neonates with EA, 93% to 94% present with a combination of both TEF and EA, while approximately 6% to 7% of newborns manifest with only EA.2 Understanding these anatomical anomalies is vital to determine the right surgical and medical approach in this population.4 The definitive management of neonates with esophageal atresia is surgical intervention.1 However, this intricate malformation is still a difficult condition in pediatric surgical management.4,5
Esophageal atresia is considered a fetal anomaly and neonatal emergency with a significantly improved prognosis in industrialized countries. Nowadays, in high-income countries, the survival rate exceeds 95% and an increasing number of EA neonates reach adulthood due to the advancement of medical care, including neonatal and surgical procedures.4,6,7 Moreover, 100% one-week survival was reported for EA neonates without associated anomalies.8,9 Lower rates, up to 87%, are reported for EA neonates born with associated cardiac anomalies, very low birth weight (<1500 g), and long-gap EA.10,11
Mortality from EA in low- and middle-income countries (LMIC) is very high, ranging from 30% to 80%.12 In sub-Saharan Africa, this anomaly is still accountable for high morbidity and mortality and raises several questions about the management of esophageal atresia.13,14 Even though the prognosis of esophageal atresia is good in the developed world, the reverse is true in developing countries. Neonates with EA cases increase from time to time in Ethiopia, and most neonates die either before the surgical intervention or after surgical repair of the atresia due to different causes.6,15
Esophageal atresia accounts for 3% of intrauterine deaths and 27% of induced abortion among perinatally detected pregnancies.2,16,17 However, the majority of EA cases came up with live births. Of the EA live births, around 55% have associated birth defects or other anomalies.2
Despite the fact that multiple predictors of mortality have been identified in different research, the role of malnutrition, thrombocytopenia, and dehydration on EA newborn mortality has not been fully explored in prior studies. These characteristics were deemed to have an association with time to death in EA neonates based on the authors’ clinical experience. Most notably, there has never been a study of EA newborns’ time to death and predictors in Ethiopia. As a result, the goal of this study was to determine the time to death and predictors of mortality among neonates with esophageal atresia at Tikur Anbessa Specialized Hospital (TASH), and thus it can be used to guide the development of guidelines for preventing neonatal mortality due to EA in the country, thereby contributing to the country’s neonatal target of the Sustainable Development Goals (SDG) by 2030.
Methods
Study Setting, Design, Period, and Population
Institutional-based retrospective follow-up study was conducted among EA neonates admitted to NICU of Tikur Anbessa Specialized Hospital (TASH). TASH is founded in Addis Ababa, the capital of Ethiopia and seat of the African Union and United Nations World Economic Commission for Africa (Figure 1). It is the largest and best-known public hospital, established in the early 1964s.18 TASH is the single largest specialized hospital in Ethiopia, and it is the only hospital that serves as a management center for neonates having esophageal atresia in the country. In TASH, the neonatal ward is divided into four rooms: preterm critical room, preterm stable room, term room and mother side room.19 All medical charts of neonates with esophageal atresia at TASH during the study period were the source population. Data were collected from February 10 to March 10/2021.
 |
Figure 1 ArcMap of the study area with respect to regions of Ethiopia. |
Participants
From March 1, 2011, through February 30, 2021, all medical charts of infants with esophageal atresia at TASH were included. The study removed medical charts with missing information (discharge date and outcome status).
Sample Size Determination and Sampling Procedure
There were 225 eligible EA newborns admitted to TASH NICU between March 2011 and February 2021. However, because there was no known relative hazard or censoring rate of our variables from prior research in a similar scenario, it was unable to use the sample size calculation formula for survival analysis. As a result, we looked at all 225 EA cases for the study.
Data Collection Procedure and Tool
All the available information on EA neonates’ records was checked, and the data extraction format was prepared in English to extract all the relevant information from the neonates’ charts. The initial time for the chart review was the diagnosis of EA, while the end time was the date of death, date of recovery, date of loss to follow-up, date of against, and 28 days of postnatal age. All charts of babies with EA admitted in TASH from March 2011 to February 2021 were retrieved from the registration books, and the charts of all study subjects were selected based on the eligibility criteria. Trained NICU nurses collected the data.
Data Quality Assurance and Analysis
To maintain data quality, supervisors and data collectors were trained for one day on how and what information they should collect from the targeted data sources. Data extraction forms were first checked (pretested) before data collection for their completeness and consistency using 13 (5%) of the study subjects.
Data were entered by Epi-data (version 4.6.0.2) and exported to Stata (version 16) for further analysis. Kaplan–Meier curve was used to estimate the failure curve from the observed survival times, and a comparison of the two survival curves was done using the Log rank test.
Bivariable Cox regression analysis was conducted to assess the effect of each independent variable on the outcome variable. Variables with a P-value <0.25 in the bivariable Cox regression analysis were included in the multivariable Cox regression analysis to identify the independent predictors of mortality among EA neonates. All statistical tests were considered significant at 0.05% or 5%. The Cox regression model for proportional hazard assumptions was checked by using the Schoenfeld residuals test.
Result
Sociodemographic and Neonatal Characteristics of the Study Participants
In this study, there were 248 cases of which 225 had sufficient clinical data for inclusion. The post-natal age at admission ranged from 30 minutes to 19 days with mean postnatal age of 3.3 days (SD ± 2.93) and more than half of the neonates 122 (54.2%) had postnatal age of at least 2 days at admission. The mean time of diagnosis of EA was 2.98 (SD ±2.76) days and more than half 133 (59.1%) were diagnosed with oesophageal atresia after two days of birth. Regarding gestational age at birth, 168 (74.7%) EA neonates were terms. Among 225 EA neonates, 193 (88.5%) had proximal esophageal atresia with distal TEF (type C) (Table 1).
Maternal Related Characteristics
Among mothers of the 225 EA neonates, about 51 (22.7%) of the mothers had a history of polyhydraminios. Nearly three-quarters 168 (74.7%) of the mothers had a spontaneous vaginal delivery and a significant majority 214 (95.1%) of them were born at a health facility (Table 2).
 |
Table 2 Maternal Related Characteristics of Neonates Diagnosed with Esophageal Atresia Admitted to TikurAnbesa Specialized Hospital, Addis Ababa, Ethiopia; from March 2011 to February 2021 (n = 225) |
Clinical Comorbidity Related Conditions of the EA Neonates
Aspiration pneumonia 203 (90.2%), sepsis 77 (34.2%), thrombocytopenia 100 (45.7%), malnutrition 126 (59.1%), dehydration 94 (41.8%), gastroesophageal reflux disease (GERD) 42 (18.7%), and metabolic abnormality 18 (8%) were the most common clinical comorbidities associated with esophageal atresia among all neonates included in the study.
Treatment-Related Characteristics of the EA Neonates
Among the study subjects, surgical intervention was done for 119 (52.7%) neonates with esophageal atresia. Primary repair (fistula ligation and end-to-end esophageal anastomosis) was done for 105 (88.2%) of the EA neonates, while gastrostomy was done for 14 (11.8%) of the EA neonates. Among those EA neonates who were given surgical intervention, 23 (19.3%) had surgery within three days of admission, whereas 96 (80.7%) had surgery after three days of admission. About 13 (10.9%) of the EA neonates had a surgical-related complication, and 10 (8.4%) of whom had an anastomotic leak, while only 3 (2.5%) had surgical site infection.
The Proportion of Neonatal Death Diagnosed with Esophageal Atresia
Two hundred and twenty-five neonates with EA have followed a total of 2933 neonate-days with a minimum of 1 hour to a maximum of 28 days, with a median time to death of 11 days (95% CI, 8.92–13.08). Among the deaths, 75 (46.9%) died within the first 7 days of admission, while 48 (30%) within the second week of admission. About 65 (28.9%) of the EA neonates were censored; with 18 (8%) against,40 (17.8%) discharged and 7 (3.1%) lost to follow-up.
Time to Death and Incidence Density Death Rate of Neonates with Esophageal Atresia
The median time to death of the entire cohort was 11 days (95% CI, 8.92–13.08). The incidence death rate of neonates diagnosed with esophageal atresia was found to be 5.5 (95% CI, 4.7–6.4) per 100-neonates’ days.
The cumulative probability of failure at the end of the first day was 0.44%, at fifth to sixth days was 25.64%, at 20–21 days was 65.51% and at the end of the follow-up was 71.56% (Figure 2).
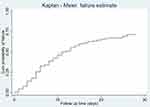 |
Figure 2 Kaplan–Meier failure curve of neonates with esophageal atresia admitted in NICU at TikurAnbesa specialized Hospital from March 2011 to February 2021(n = 225). |
Proportional hazard assumption was assessed using Kaplan-Meier failure curve, and Schoenfeld residual global test and Proportional Hazard (PH) assumption were met (chi 2 = 15, prob >chi2 = 0.3783) (Figure 3).
Predictors of Time to Death in Neonates with Esophageal Atresia
Bivariable and multivariable Cox regression was used for analysis to identify predictors of time to death for neonates with esophageal atresia from admission to discharge/death in the neonatal intensive care unit. Findings from the bivariate analysis showed that birth weight, gestational age admission source, associated anomalies, delivery place, history of maternal chronic illness, sepsis, aspiration pneumonia, malnutrition, thrombocytopenia, dehydration, time of diagnosis, time of surgery, metabolic abnormality, and type of variant were associated with time to death of neonates diagnosed with esophageal atresia at p-value <0.25 (Table 3). However, in the multivariable analysis birth weight, sepsis, dehydration, malnutrition, time of diagnosis, and time of surgery had a statistically significant association with time to death of neonates with esophageal atresia at p-value <0.05 (Table 3).
The hazard of death among neonates who had very low birth (VLBW) weight was 3.9 times higher as compared to normal birth weight neonates (AHR = 3.90, 95% CI (1.36–11.17)). Similarly, the risk of death among neonates who had low birth weight (LBW) was increased by 49% as compared to those who had normal birth weight neonates (AHR = 1.49, 95% CI (1.02–2.20)).
This finding showed that the risk of death among neonates who did not have surgical intervention was 3.73 times higher as compared to those who underwent surgical intervention before three days of life (AHR; 3.73, 95% CI (1.34–10.38)).
The hazard of death for neonates with esophageal atresia who did not have malnutrition was decreased by 39% as compared to its malnourished counterparts (AHR = 1.61, 95% CI (1.03−2.58)).
The risk of death of neonates with esophageal atresia, who were diagnosed after two days of life, was 1.48 times higher as compared to neonates diagnosed before two days of life (AHR = 1.48, 95% CI (1.01–2.15)).
Dehydrated neonates with esophageal atresia had had 2.38 times higher risk of death when compared with those who did not have dehydration (AHR = 2.38, 95% CI (1.63–3.46)).
Neonates with esophageal atresia who did not have sepsis were 33% less likely to die than their septic counterparts (AHR=1.67,95% CI (1.15–2.44)).
Discussion
The study aimed to determine the time to death of neonates with esophageal atresia and to identify predictors of time to death. Of the total of 225 neonates with esophageal atresia included in the study, 71.1% died, 17.8% were discharged, 8% went against medical advice, and 3.1% were lost to follow-up.
The proportion of deaths among neonates diagnosed with esophageal atresia admitted at NICU of TASH was 71.1%. This finding was comparable with the study conducted in Nigeria 68.4%20 but lower than prior studies conducted in Senegal 78% and Ethiopia 85.3%.13,15 This discrepancy might be due to the comparatively improved healthcare-seeking and utilization behavior of the community, and accessibility of trained health care providers in the last 10 years (study period) than ever before. Moreover, methodological variations like study period, study design, and sample size might be attributed to the discrepancy. However, our finding was significantly higher than the studies conducted in the United States 9%, Melbourne 13.5%, and Boston 5.1%21–23 which might be due to the presence of advanced medical and surgical care of neonates with esophageal atresia in western countries. Moreover, the unavailability of total parenteral nutrition (TPN) and mechanical ventilation in the NICU of TASH could be among the reasons for the higher death rate in the TASH setting.
In this study, septic EA neonates were at greater hazard of death than those without sepsis, and this finding accords with studies conducted in Senegal and Saudi Arabia.13,24 The similarity may be asserted by the clinical evidence that sepsis could complicate the neonates with EA and prolong surgical intervention, thus fastening their time to die. Unlike this study, a study in Indonesia revealed a non-significant association of sepsis with time to death among EA neonates.25
Neonates diagnosed with EA after two days of life had an increased hazard of association with time to death as compared to those whose diagnosis was made before 2 days of life. The possible reason might be due to the fact that delay in the diagnosis of neonates may cause severe aspiration pneumonia, dehydration, sepsis, and dependence on mechanical ventilation. Even though neonates with EA should be diagnosed during the antenatal period or within hours of birth, in our study area almost all the study neonates were referred from different health institutions in the country. As a result, the chances of having delayed diagnosis, aspiration pneumonia, dehydration, and sepsis were higher in Ethiopia when compared to developed countries. This could hurt the survival of the EA neonates in the country, which was supported by the study conducted in Turkey and Tunisia.26,27
Dehydration was significantly associated with the time to death of neonates diagnosed with EA, which is explained by the clinical practice that neonates with esophageal atresia have decreased fluid intake, inadequate breastfeeding, and excessive secretion due to atresia in the esophagus, all of which lead to dehydration. And untreated dehydration in EA neonates may end up with life-threatening complications including hypovolemic shock, heat injury, kidney failure, seizure, electrolyte imbalance, and death. This finding is supported by a study in Kenya.28
Esophageal atretic neonates whose birth weight was <2500 g had a higher hazard of death than their normal birth weight counterparts, which may be due to the fact that LBW and VLBW EA neonates are more likely to be preterm, hence suffering from preterm-related complications that may hasten their time to die. This finding was lower than the study conducted in Tunisia. However, this finding negates the study conducted in Boston and San Francisco, which revealed that birth weight did not have an association with mortality.21 The discrepancy might be attributed to the variable categorization and study design.
In this study, being malnourished was a positive predictor of time to death among neonates diagnosed with EA. This finding can be asserted by the clinical evidence that EA neonates have feeding difficulties resulting in low calories and immunity which affect their growth and development. Furthermore, in the study setting, total parenteral nutrition was not accessible, and thus EA neonates were kept NPO for a prolonged time. Consequently, EA neonates were at further risk of being malnourished, which increases their risk of mortality because malnutrition delays the time required for surgical intervention. The finding was congruent with the multi-institutional cohort study conducted in Columbus.29
The hazard of death among EA neonates who did not have surgical intervention was higher than those who were surgically intervened before three days of admission and this finding was in accordance with the study conducted in Iran.30 However, unlike the study in Iran, a significant majority of neonates diagnosed with EA in TASH received the surgical intervention after their third day of admission. This can in turn increase the risk of acquiring clinical co-morbidities which contribute to further delay in their surgical intervention, thus increasing the risk of mortality among EA neonates. Besides, in this study, 50% of the EA cases had their fistula repaired on the ninth day of admission, which was quite longer than the first 24 hours’ time in Serbia. Overall, there was a delay in surgical intervention at TASH, which might be attributed to the delay in diagnosing the EA, associated anomalies, and clinical comorbidities.
In conclusion, as compared to other studies, the proportion of newborns identified with esophageal atresia who die in TASH is high. It took an average of 11 days for someone to die. Low birth weight, presence of sepsis, having malnutrition, lack of surgery, later diagnosis, and being dehydration were associated with increased hazards of death among EA neonates. Esophageal atresia is life-threatening because it inhibits the flow of nutrients from the mouth to the lower digestive tract. As a result, all responsible agencies should endeavor to expand the esophageal atresia treatment center and provide the necessary intervention equipment, such as mechanical ventilation, suction machines, and total parenteral nutrition, in the hospital. To achieve the neonatal target of reducing neonatal mortality rate (NMR) to 12 per 1000 live births by 2030, early diagnosis and referral, improved transportation to the treatment center, timely surgical intervention, and appropriate management of clinical comorbidities with standard of care are critical.
The first nationwide investigation on time to death and predictors among newborns diagnosed with esophageal atresia is a strength of this study. Furthermore, malnutrition, thrombocytopenia, and dehydration were included as independent variables in this study, which had not been thoroughly studied in prior investigations. There are certain limitations to this research. Because this study relied on secondary data, the information available from the patients’ charts limited the investigation of factors for time to death. Any death noted on the medical chart of infants with EA was considered a death (event) related to esophageal atresia during the follow-up period.
Data Sharing Statement
The data are accessible from the corresponding author upon reasonable request.
Ethics Statement
This study was approved by the research ethics committee from Addis Ababa University College of Health Science and School of Nursing. A waiver of informed consent was approved from TASH to review the patient’s medical records as per Helsinki's declaration. Patient identification numbers and their names were removed for their confidentiality. A supporting letter was obtained from the TASH Quality Office. Data were only used for the purpose of this study, not for other purposes informed.
Acknowledgments
First and foremost, we would like to thank Tikur Anbessa Specialized Hospital administration staff and health care providers for their valuable support while collecting the data. Our thanks also go to all data collectors and supervisors for carrying out their responsibilities effectively during data collection.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all the areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Disclosure
We disclose that this manuscript was based on the thesis entitled “Time to death and predictors among neonates with esophageal atresia in Ethiopia”.31 The authors declare no conflicts of interest in relation to this research work.
References
1. Scott DA Esophageal atresia/tracheoesophageal fistula overview. GeneReviews [Internet]. 1–10. Available from: https://www.ncbi.nlm.nih.gov/books/%0AEsophageal.
2. Pedersen RN, Calzolari E, Husby S, Garne E, Andersen HC. Oesophageal atresia: prevalence, prenatal diagnosis and associated anomalies in 23 European regions. Arch Dis Child. 2012;97(3):227–232. doi:10.1136/archdischild-2011-300597
3. Sfeir R, Bonnard A, Khen-Dunlop N, et al. Esophageal atresia: data from a national cohort. J Pediatr Surg. 2013;48(8):1664–1669. doi:10.1016/j.jpedsurg.2013.03.075
4. Pinheiro PFM, e Silva ACS, Pereira RM. Current knowledge on esophageal atresia. World J Gastroenterol. 2012;18(28):3662–3672. doi:10.3748/wjg.v18.i28.3662
5. Mortell AE, Azizkhan RG. Esophageal atresia repair with thoracotomy: the Cincinnati contemporary experience. YSPSU. 2009;18(1):12–19.
6. Tröbs RB, Finke W, Bahr M, et al. Isolated tracheoesophageal fistula versus esophageal atresia – early morbidity and short-term outcome. A single institution series. Int J Pediatr Otorhinolaryngol. 2017;94:104–111. doi:10.1016/j.ijporl.2017.01.022
7. Bouguermouh D, Salem A. Original article Esophageal atresia: a critical review of management at a single center in Algeria. Dis Esophagus. 2014;27(1):1–6. doi:10.1111/dote.12030
8. Donoso F, Kassa AM, Gustafson E, Meurling S, Lilja HE. Outcome and management in infants with esophageal atresia – a single centre observational study. J Pediatr Surg. 2016;51(9):1421–1425. doi:10.1016/j.jpedsurg.2016.03.010
9. Cassina M, Ruol M, Pertile R, et al. Prevalence, characteristics, and survival of children with esophageal atresia: a 32-year population-based study including 1,417,724 consecutive newborns. Birth Defects Res Part A Clin Mol Teratol. 2016;106(7):542–548. doi:10.1002/bdra.23493
10. Sulkowski JP, Cooper JN, Lopez JJ, et al. Morbidity and mortality in patients with esophageal atresia. Surgery. 2014;156(2):1–17. doi:10.1016/j.surg.2014.03.016
11. Powell L, Frawley J, Crameri J, Teague WJ, Frawley GP. Oesophageal atresia: are “long gap” patients at greater anesthetic risk? Paediatr Anaesth. 2018;28(3):249–256. doi:10.1111/pan.13336
12. Alslaim HS, Banooni AB, Shaltaf A, Novotny NM. Tracheoesophageal fistula in the developing world: are we ready for thoracoscopic repair? Pediatr Surg Int. 2020;36(5):649–654. doi:10.1007/s00383-020-04639-7
13. Fall M, Mbaye PA, Horace HJ, et al. Oesophageal atresia: diagnosis and prognosis in Dakar, Senegal. Afr J Paediatr Surg. 2015;12(3):187–190. doi:10.4103/0189-6725.170196
14. Bandré E, Niandolo K, de Pediatrie AWA. Oesophageal atresia: management in sub Saharan countries. europepmc.org [Internet]; 2010 [cited November 1, 2020]: 2. Available from: https://europepmc.org/article/med/20034771.
15. Amare M, Habtamu A. Assessment of the outcomes of neonates with the diagnosis of esophageal atresia and/or tracheoesophageal fistula admitted to Tikur Anbessa specialized hospital- neonatal intensive care unit. Ethiop J Pediatr. 2013;10:13.
16. van Lennep M, Singendonk MMJ, Dall’Oglio L, et al. Oesophageal atresia. Nat Rev Dis Prim. 2019;5(1). doi:10.1038/s41572-019-0077-0.
17. Nassar N, Leoncini E, Amar E, et al. Prevalence of esophageal atresia among 18 international birth defects surveillance programs. Birth Defects Res Part A Clin Mol Teratol. 2012;94(11):893–899. doi:10.1002/bdra.23067
18. Ababa A, Hailu S Black lion hospital total enrollment: 2015;2015.
19. NICU reference guide AAU. 2011.
20. Ekenze SO, Ajuzieogu OV, Nwankwo EP. Effect of cardiac banding and improved anaesthetic care on outcome of oesophageal atresia in a developing country. J Trop Pediatr. 2018;64:1–5.
21. Lazow SP, Aribindi VK, Staffa SJ, et al. Predictors of index admission mortality and morbidity in contemporary esophageal atresia patients. J Pediatr Surg. 2020;55:2–8.
22. Wang B, Tashiro J, Allan BJ, et al. A nationwide analysis of clinical outcomes among newborns with esophageal atresia and tracheoesophageal fistulas in the United States. J Surg Res. 2014;190(2):604–612. doi:10.1016/j.jss.2014.04.033
23. Tanny SPT, Fearon E, Hawley A, et al. Predictors of mortality after primary discharge from hospital in patients. J Pediatr. 2019:1–6. doi:10.1016/j.jpeds.2019.12.031
24. Al-Salem AH, Kothari M, Oquaish M, Khogeer S, Desouky MS. Morbidity and mortality in esophageal atresia and tracheoesophageal fistula: a 20-year review. Ann Pediatr Surg. 2013;9(3):93–98. doi:10.1097/01.XPS.0000430524.83127.5d
25. Purniti PS. Sensitization to indoor allergens and frequency of asthma exacerbations in children. Paediatr Indones. 2011;51(4):207–212.
26. Ammar S, Sellami S, Sellami I, et al. Management of esophageal atresia and early predictive factors of mortality and morbidity in a developing country. Dis Esophagus. 2019;32:1–6.
27. Karakus SC, Ozokutan BH, Bakal U, et al. Delayed diagnosis: an important prognostic factor for oesophageal atresia in developing countries. J Paediatr Child Health. 2016;52(12):1090–1094. doi:10.1111/jpc.13354
28. Akech S, Rotich B, Chepkirui M, Ayieko P, Irimu G, English M. The prevalence and management of dehydration amongst neonatal admissions to general paediatric wards in Kenya-a clinical audit. J Trop Pediatr. 2018;64(6):516–522. doi:10.1093/tropej/fmx108
29. Sulkowski JP, Cooper JN, Lopez JJ, et al. Morbidity and mortality in patients with esophageal atresia. Surgery. 2014;156(2):1–7.
30. Davari HA, Hosseinpour M, Nasiri GM, Kiani G. Mortality in esophageal atresia: assessment of probable risk factors (10 years’ experience). J Res Med Sci. 2012;17(6):540–542.
31. Misganaw NM. Time to death and predictors among neonates with esophageal atresia in Ethiopia [thesis]. Addis Ababa: Addis Ababa University;; 2021.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



