Back to Journals » Patient Preference and Adherence » Volume 12
Time preference, outcome expectancy, and self-management in patients with type 2 diabetes
Authors Karl FM, Holle R , Schwettmann L, Peters A, Laxy M
Received 23 May 2018
Accepted for publication 21 July 2018
Published 26 September 2018 Volume 2018:12 Pages 1937—1945
DOI https://doi.org/10.2147/PPA.S175045
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Florian M Karl,1,2 Rolf Holle,1,2 Lars Schwettmann,1 Annette Peters,2,3 Michael Laxy1,2
1Institute of Health Economics and Health Care Management, Helmholtz Zentrum München (GmbH), German Research Center for Environmental Health, Neuherberg, Germany; 2German Center for Diabetes Research (DZD), Neuherberg, Germany; 3Institute of Epidemiology II, Helmholtz Zentrum München (GmbH), German Research Center for Environmental Health, Neuherberg, Germany
Background: Patient self-management is crucial to prevent complications and mortality in type 2 diabetes. From an economic perspective, time preference predicts short-sighted decision making and thus might help to explain non-adherence to self-anagement recommendations. However, recent studies on this association have shown mixed results.
Purpose: In this study, we tested whether the combination of time preference and outcome expectancy can improve the predictions of self-management behavior.
Patients and methods: Data from 665 patients with type 2 diabetes were obtained from the cross-sectional KORA (Cooperative Health Research in the Region of Augsburg) GEFU 4 study. Time preference and outcome expectancy were measured by one question each, which were answered on a 4-point Likert scale. Their association with six self-managing behaviors was tested in logistic and linear regression analyses. Likewise, we examined the association between self-management and the interaction of outcome expectancy and time preference.
Results: A high time preference was associated with a significantly lower sum of self-management behaviors (β=-0.29, 95% CI [-0.54, -0.04]). Higher outcome expectancy was associated with a higher self-management score (β=0.21, 95% CI [-0.03, 0.45]). The interaction model showed that low time preference was only associated with better self-management when combined with a high outcome expectancy (β=0.05, 95% CI [-0.28, 0.39] vs β=0.27, 95% CI [-0.09, 0.63]).
Conclusion: Time preference and outcome expectancy are interrelated predictors of patient self-management and could be used to identify and to intervene on patients with a potentially poor self-management.
Keywords: behavioral economics, adherence, temporal discounting, health behavior
Introduction
Self-managing behavior in patients with type 2 diabetes is crucial in the prevention of disease progression and development of comorbidity.1 In addition, a study described an association between self-management and mortality in type 2 diabetes.2 Therefore, a large morbidity and mortality burden could be prevented by enabling patients to adhere to recommended self-management.3–5
Self-management in type 2 diabetes includes, among other behaviors, monitoring of blood sugar, blood pressure, and body weight, conducting regular foot care, having a dietary plan, and keeping a diabetes diary.5,6
Although great effort has been put into supporting patient self-management, adherence to recommended self-management remains challenging for many patients.7 Review articles by Egginton et al8 and Elissen et al9 have shown that adherence to recommended care and the effect of interventions vary greatly across different studies and patient populations.
Self-management in patients with diabetes represents choices between immediate smaller (dis)utility activities, such as self-monitoring of blood glucose, and (dis)utility that may be bigger but distant in time such as diabetic complications. These kinds of intertemporal choices are also subject to economic theory.10
In economics, the preference for smaller but immediate over larger later rewards is called time preference. The trigger for time preferences is called temporal discounting and stands for a decrease in expected utility that is related to the period of delay.11 The more an individual discounts future (dis)utility, the more likely the individual is to prefer smaller immediate utility over timely distant but bigger utility or, vice versa, larger later disutility over smaller immediate disutility. Although time preference with regard to a health outcome can be rational for many reasons, eg, a short life expectancy, many studies have described a variance in time preferences which was not solely explained by interindividual differences in health-related characteristics, eg, age or disease status.11 Therefore, low adherence rates to recommended self-management might be related to patients’ temporal discounting. A relatively high depreciation of future (dis)utilities is coterminous with a relatively high time preference, ie, preferring smaller immediate over larger later utilities and also preferring larger later disutility over smaller immediate disutility.12 Subsequently, the term “high time preference” will be used instead of “high depreciation rate”, because we do not use a rate but a preference in our analysis.
In economic theory, the expected utility of a behavior represents the product of a payoff that is associated with a certain decision or behavior and the probability of this payoff being realized. In the case of intertemporal choices, the expected utility is then multiplied by an individual’s temporal discounting factor.13 In this study, we approached the measurement of perceived utility in health investments through outcome expectancy. Psychosocial models, such as the Health Action Process Approach and the Health Belief Model, use outcome expectancy to summarize the subjective beliefs about a possible outcome and the probability of its actual occurrence as a result of the behavior of interest.14–16 Although an expected outcome is not equal to an expected utility, we proposed outcome expectancy as a proxy for expected utility in a case where utility is difficult to quantify, ie, health.
Within this study, we aimed to assess the relationship between time preference, outcome expectancy, and combinations of time preference and outcome expectancy with self-management behavior in patients with type 2 diabetes. Despite contributing to the discussion on the relevance of both factors in the health domain, the analysis of the combinations of time preference and outcome expectancy shows whether the inclusion of (health) behavior-specific utility measures could improve predictions of time preference in future studies.
Literature review
An overview of the relationship between time preference and health behavior is given in the studies by Story et al11 and Lawless et al.12 Both concluded that a high time preference, ie, a relatively strong depreciation of timely distant (dis)utilities, is associated with unhealthy behavior, eg, smoking, an unhealthy diet, or alcohol consumption. However, studies on diabetes-specific behaviors are scarce. One study on the association between time preference and patient self-management was performed by Sloan et al.17 They reported no significant association between time preference and the testing of HbA1c or cholesterol concentration during the past year or engagement in physical exercise and regular medication intake. A possible reason for the nonsignificant result might be the low threshold for adherence, eg, testing blood glucose once a year. Emoto et al18 reported higher retinopathy rates in individuals with high time preference. Other recent articles by van der Pol et al19 and Shuval et al20 are also related to diabetes but they examined the association between time preference and general health behaviors. Specifically, van Der Pol et al reported lower adherence rates after dietary and physical activity advice in participants with a high time preference. Shuval et al20 found more frequent fast-food consumption in individuals with high time preference.
Outcome expectancy was found to be significantly associated with higher adherence to blood glucose monitoring.21 Furthermore, Wu et al22 reported a significant association with better self-management (diet, exercise, medication, blood sugar, and foot care over the past 7 days). Other studies by Williams and Bond23 and Gibson et al24 reported a similar relationship. When we consider outcome expectancy as a proxy for expected utility, there is a clear link between time preference and outcome expectancy in economic theory. However, we found no empirical studies on the interaction of time preference and outcome expectancy.
Theoretical framework
The idea of predicting health behavior based on expected utility was introduced by Grossman.25 His assumption was that individuals consume and invest health capital with the aim of utility maximization. As a result, the expected utility of a health investment determines its demand.26 Usually, the expected utility of an investment is described by:
| (1) |
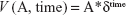
where U(A) is the utility of a behavior and p is the probability of this utility being realized.11 In our study, we assumed outcome expectancy as a proxy for p*U(A). For timely distant utilities, the expression changes to:11,13
| (2) |
In this study, time preference is represented by the temporal discounting factor δ, which exponentially decreases the expected utility over time. If we assume outcome expectancy as a proxy for expected utility, the expression demonstrates that the effect of time preference becomes larger or smaller depending on the outcome expectancy and vice versa. To test this, we examined the associations between the four different combinations of dichotomized outcome expectancy (low/high) and dichotomized time preference (low/high) and patient self-management.
Materials and methods
We used data from the German KORA GEFU 4 study (Cooperative Health Research in the Region of Augsburg, Health Follow-up 4). GEFU 4 is a cross-sectional, population-based study conducted from 2015 to 2017 that included all eligible participants from four independent cross-sectional surveys: S1 (n=4,022, 1984–1985), S2 (n=4,940, 1989–1990), S3 (n=4,856, 1994–1995), and S4 (n=4,261, 1999–2001) with responses from 9,035 individuals. The self-administered questionnaire was completed only by participants who had affirmed in a previous questionnaire or telephone interview that a physician had diagnosed them with diabetes (n=749). Furthermore, only participants with type 2 diabetes (n=665) answered questions that aimed to detect outcome expectancy and time preference in participants.
Self-management
Measures of self-management included the following: monitoring of body weight (at least once per week), conducting regular foot care (checking for wounds at least once per week), measuring blood sugar (at least once a day for patients treated with insulin and at least once a week for all others), measuring blood pressure (at least once per week), keeping a diabetes diary, and having a diet plan. Participants were asked to consider the past 6 months for their answers. Furthermore, we combined these six self-managing behaviors into a score where 1 point was attributed per criterion in each individual, as proposed by Arnold-Wörner et al.27 A similar score is known to be highly predictive of all-cause mortality in patients with type 2 diabetes.2
Time preference
Time preference for health-related outcomes is not stable compared with time preference in monetary decision-making.11,28 Therefore, the temporal discounting rate for the different self-management domains is difficult to capture. We approached this issue according to the method of Sloan et al17 by applying a single indicator question that assessed whether participants preferred immediate pleasure over long-term health. Participants were asked to respond to this statement: “My present well-being is more important to me than my future health status”. Responses were given on a 4-point Likert scale (“strongly disagree” [1] to “strongly agree” [4]). To measure time preference, we set “agree” and “strongly agree” to 1 (high time preference) and “disagree” and “strongly disagree” to 0 (low time preference). Furthermore, to test the plausibility of our time preference measure, we asked participants to respond to the following statement: “It is not worth keeping a healthy diet and being physical active because the effort in the present outweighs the future benefits”. We set “agree” and “strongly agree” to 1 (agree) and “disagree” and “strongly disagree” to 0 (disagree).
Outcome expectancy
Outcome expectancies, as described in the Health Action Process Approach, summarize the subjective beliefs about a possible outcome and the probability that it will actually occur as a result of a certain action.16 The overall key dimensions in self-management are physical activity and dietary behavior.5 Thus, we used them to approximate general outcome expectancy with regard to self-management. Participants were asked to respond to this statement: “I can prevent my disease from progression if I am physically active and have a healthy diet”. Responses were given on a 4-point Likert scale (“strongly disagree” [1] to “strongly agree” [4]). To measure outcome expectancies, we used the median as cutoff (median equaled 3 and mean equaled 3.32) and assigned “strongly agree” to 1 (high outcome expectancy) and “agree”, “disagree”, and “strongly disagree” to 0 (low outcome expectancy). Furthermore, to test the plausibility of our outcome expectancy measure later on, we asked participants whether they agreed or disagreed with the following statement: “I could have prevented myself from developing type 2 diabetes if I had been more physically active and had a healthier diet”.
Covariates
We assessed sociodemographic information: sex, age, and education (primary education, ≤10 years of school; secondary/tertiary education, >10 years of school). Furthermore, we assumed that insulin treatment might have functioned as a health shock and thus have altered health behavior and preferences.29 Thus, we assessed whether participants’ treatment regimens included the injection of insulin. In addition, we asked participants to state whether they had ever participated in a diabetes education program that had not happened as part of routine care or during a hospital stay.
Statistical analyses
In the first step, we reported participants’ characteristics with regard to sociodemographics, treatment regimen, and self-management. To examine the determinants of outcome expectancy and time preference measures, we regressed these on age, sex, education, participation in an educational program, and treatment regimen using logistic regression models.
We analyzed the association between outcome expectancy, time preference, and the different self-management behaviors and their sum score using logistic and linear regression models.
To examine the four possible combinations between high and low outcome expectancy and high and low time preference, we used regression models that included dummies for the respective combinations. Individuals who combined low outcome expectancy with high time preference, and thus with the lowest expected values, were used as reference. All models were adjusted for age, sex, education, participation in a diabetes education program, and treatment with insulin. In all analyses, P-values of <0.05 were assumed to be statistically significant. Analyses were performed using RStudio (Boston, MA, USA).30
Sensitivity analyses
Although the two measures of time preference and outcome expectancy are not on an interval scale, we tested them as metric predictors (1–4) in similar models to the main analyses. To test the combination of both factors, we recoded the time preference measure so that a “very high time preference” was coded as “0” and a “very low time preference” was coded as “4”. In the combined model, we used the product of outcome expectancy and time preference (1–16) as a predictor.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the ethics committee of the Bavarian Medical Association (approval number: 08064) and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Results
Characteristics
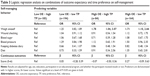
Of the 664 patients with type 2 diabetes in our study, the mean age was 71 years (42–93 years). Moreover, 55.3% were men and 40.5% had higher school education. Therapy regimens included insulin use in 19.5% of our participants. Details are given in Table 1.
  | Table 1 Characteristics of the patients with type 2 diabetes |
Determinants and plausibility of outcome expectancy and time preference measures
Logistic regression analysis on the associations of diverse patient characteristics with our outcome expectancy and time preference measures showed that individuals who had participated in an educational program were more likely to have a high outcome expectancy (OR: 1.64, 95% CI [1.18, 2.30]). Moreover, age was a significant predictor of high time preference, ie, the older the participants were, the higher their chance of having a high time preference (OR: 1.68, 95% CI [1.39, 2.04]).
With regard to the plausibility questions, high outcome expectancy was significantly associated with agreement with the following statement: “I could have prevented myself from developing type 2 diabetes if I had been more physically active and had a healthier diet” (OR: 2.69, 95% CI [1.93, 3.77]). Individuals with high time preference were significantly more likely to agree with the statement: “It is not worth keeping a healthy diet and being physically active because the effort in the present outweighs the future benefits” (OR: 4.38, 95% CI [3.01, 6.43]). Details are given in Table S1.
Correlation between outcome expectancy and time preference was −0.17 (P=0.0002). The partial correlation was −0.18 (P=0.001).
Regression analysis: outcome expectancy, time preference, and patient self-management
Table 2 presents the logistic regression analysis for patient self-management and the linear regression analysis for the self-management score. High outcome expectancy was significantly associated with adhering to the recommendation to monitor body weight on at least a weekly basis (OR =1.55, 95% CI [1.14, 2.20]). Otherwise, no other association of high outcome expectancy with self-management behavior was statistically significant. However, all mean effect estimates indicated that high outcome expectancy is associated with a higher probability of adhering to the recommended self-management.
Individuals with high time preference were less likely to adhere to the recommended amount of monitoring of their blood sugar (OR: 0.69, 95% CI [0.46, 1.03], P=0.07). In addition, the probability of measuring blood pressure with sufficient frequency was lower in individuals with high time preference (OR: 0.71, 95% CI [0.51, 1.01], P=0.05). Moreover, all coefficients (except for keeping a diabetes diary) indicated that individuals with a high time preference were less likely to be adherent to the recommended self-management. The overall self-management score was significantly lower (β=−0.29, 95% CI [−0.57, −0.05]) in individuals with high time preference.
Regression analysis: combinations of outcome expectancy and time preference and patient self-management
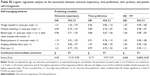
Table 3 summarizes the results of the logistic regression analysis on the association between dummy coded combinations of outcome expectancy (high/low) and time preference (high/low). Individuals with low outcome expectancy and high time preference were used as reference (n=185). These individuals were assumed to have the lowest expected utility with regard to self-management and therefore were assumed to have the lowest adherence rates.
Overall, we found that individuals with high outcome expectancy and low time preference had the highest mean adherence scores (β=0.27, 95% CI [−0.09, 0.63], P=0.14). With regard to the single self-managing behaviors, these individuals were more likely to monitor their body weight (OR =1.71, 95% CI [1.10, 2.66]) and blood pressure (OR: 1.50, 95% CI [0.96, 2.35], P=0.08) on a sufficiently regular basis.
Regression analysis: sensitivity analysis
The results of the sensitivity analysis are presented in Table S2. The β coefficient of the product of outcome expectancy and time preference, which predicted the sum score of self-managing behaviors, was the only statistically significant predictor (β=0.04, 95% CI [0.003, 0.07]).
Discussion
Using proxy questions on outcome expectancy and time preference from a population-based study, we analyzed their association with patients’ self management in patients with type 2 diabetes. The results suggest that high time preference is associated with lower overall self-management. However, the associations with most of the single behavioral aspects are only small, and therefore the association only becomes significant when summarized in a score. High outcome expectancy was associated with higher adherence rates, although only the association with body weight monitoring was of statistical significance. We argued that the association of outcome expectancy or time preference with self-management depends on the expression of time preference and outcome expectancy. Our results suggest that individuals who combine high outcome expectancies with low time preference actually have the highest adherence rates.
Time preference and outcome expectancy were negatively correlated with each other. As we assumed the independence of both, this was surprising at first. However, we know that time preference is context dependent, and O’Donoghue and Rabin13 pointed out that context equals an individual’s likes and dislikes. Therefore, one possible explanation for the correlation might be that our time preference measure partly included a valuation of future health. Nonetheless, the results showed that time preference and outcome expectancy had distinct effects on the association with patients’ self-management. Individuals with a high outcome expectancy and low time preference had higher adherence rates than those with one or both values pointing in the opposite direction. Future studies could examine the interaction of a behavior-specific outcome expectancy and a behavior-neutral time preference measure.
The weak but steady association of time preference with the diverse self-management behaviors is typical for reported results on the association between time preference and health behavior.11 For example, whereas Mørkbak et al10 found a consistent and robust association of time preference with smoking and physical inactivity, Takagi et al31 reported a very small contribution of time preference in explaining health behavior. The authors are not aware of any other studies that examined the association between time preference and the specific self-management behaviors targeted within this study. Nonetheless, the significantly lower overall adherence in individuals with high time preference showed that this perceptional variance in patients is relevant for improving adherence rates. Our finding that individuals who combined low time preference with high outcome expectancy had the highest overall adherence rate (Table 3) is in line with our hypothesis, and the formulations were made by O’Donoghue and Rabin.13
Our analysis has some limitations. First, the data are based on self-report and are therefore likely to suffer from recall bias. Second, we had no information about the patients’ literacy levels with regard to the self-management behaviors. Therefore, there might be participants who did not act as recommended simply because they did not know better. However, we adjusted our models for participation in a patient education program and thus hoped to have reduced the literacy bias. Third, outcome expectancy was measured with regard to general health behavior but applied to specific self-management behaviors. Future study could profit from behavior-specific outcome expectancy measures. Finally, we are aware of the simplicity with regard to our time preference measure and the resulting difficulty in ensuring a valid representation of the phenomenon. However, the association of time preference with age and education is in line with the previous study.10 Furthermore, our approach follows the example of Sloan et al17 by assessing health-related time preference by a single item.
A general issue of studies that examine the association between time preference and health behavior is that they do not include “costs” in their model. Payoffs received in the future might be related to higher transaction costs and uncertainty. A common solution is to use a front-end delay for all possible outcomes.13 However, health behavior study is mostly based on the decision between the immediate and certain costs (self-management) and uncertain larger health threats (diabetic complications). Therefore, future studies could profit from assessing the perceived costs of the respective health investments to further improve their models.
This study showed that time preference predictions about patient self-management are dependent on outcome expectancy, in line with the comments by O’Donoghue and Rabin.13 This has not yet been applied in other studies on time preference and patient self-management. Based on the results of this study, future study could profit from including behavior-specific outcome expectancy when examining the association of time preference with health behavior or patient self-management.
Approaches to improve patient self-management by overcoming self-control issues that might arise from time preference are manifold. Sen et al32 reported an increase in the adherence to daily blood glucose monitoring after installing a lottery incentive with an expected value of US $2.80 or US $1.40 per day. In another study, Gopalan et al33 reported that the enrollment in an incentive-based healthy food program, ie, 25% cash back on healthy food purchases, was significantly increased by text messages that pointed at the positive health outcomes of healthy food. In combination, these studies support the idea that the effects of time preference are interrelated with outcome expectancy. Other successful approaches to overcome self-control issues with regard to self-management include monthly interactive reminders or social support through a prior selected adherence partner.34,35 In conclusion, knowledge about outcome expectancy and time preference could help to target improvement in patients’ self-management.
Disclosure
The authors report no conflicts of interest in this work.
References
American Diabetes Association, American Diabetes Association, Association AD. 5. Prevention or Delay of Type 2 Diabetes: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S51–S54. | ||
Laxy M, Mielck A, Hunger M, et al. The association between patient-reported self-management behavior, intermediate clinical outcomes, and mortality in patients with type 2 diabetes: results from the KORA-A study. Diabetes Care. 2014;37(6):1604–1612. | ||
Ulrich S, Holle R, Wacker M, et al. Cost burden of type 2 diabetes in Germany: results from the population-based KORA studies. BMJ Open. 2016;6(11):e012527. | ||
Mielck A, Vogelmann M, Leidl R. Health-related quality of life and socioeconomic status: inequalities among adults with a chronic disease. Health Qual Life Outcomes. 2014;12(1):58. | ||
Powers MA, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Educator. 2017;43(1):40–53. | ||
Beck J, Greenwood DA, Blanton L, et al. 2017 National Standards for Diabetes Self-Management Education and Support. Diabetes Educ. 2017;43(5):449–464. | ||
Jensen ML, Jørgensen ME, Hansen EH, Aagaard L, Carstensen B. Long-term patterns of adherence to medication therapy among patients with type 2 diabetes mellitus in Denmark: The importance of initiation. PLoS One. 2017;12(6):e0179546. | ||
Egginton JS, Ridgeway JL, Shah ND, et al. Care management for Type 2 diabetes in the United States: a systematic review and meta-analysis. BMC Health Serv Res. 2012;12(1):72. | ||
Elissen AM, Steuten LM, Lemmens LC, et al. Meta-analysis of the effectiveness of chronic care management for diabetes: investigating heterogeneity in outcomes. J Eval Clin Pract. 2013;19(5):753–762. | ||
Mørkbak MR, Gyrd-Hansen D, Kjær T. Can present biasedness explain early onset of diabetes and subsequent disease progression? Exploring causal inference by linking survey and register data. Soc Sci Med. 2017;186:34–42. | ||
Story GW, Vlaev I, Seymour B, Darzi A, Dolan RJ. Does temporal discounting explain unhealthy behavior? A systematic review and reinforcement learning perspective. Front Behav Neurosci. 2014;8:76. | ||
Lawless L, Drichoutis AC, Nayga RM. Time preferences and health behaviour: a review. Agricultural and Food Economics. 2013;1(1):17. | ||
O’Donoghue T, Rabin M. Present bias: Lessons learned and to be learned. Am Econ Rev. 2015;105(5):273–279. | ||
Becker MH. The health belief model and sick role behavior. Health Educ Monogr. 1974;2(4):409–419. | ||
Schwarzer R, Lippke S, Luszczynska A. Mechanisms of health behavior change in persons with chronic illness or disability: the Health Action Process Approach (HAPA). Rehabil Psychol. 2011;56(3):161–170. | ||
Schwarzer R, Luszczynska A. How to overcome health-compromising behaviors: The health action process approach. Eur Psychol. 2008;13(2):141–151. | ||
Sloan FA, Padrón NA, Preferences PAC. Beliefs, and Self-Management of Diabetes. Health Serv Res. 2009;44(3):1068–1087. | ||
Emoto N, Okajima F, Sugihara H, Goto R. Behavioral economics survey of patients with type 1 and type 2 diabetes. Patient Prefer Adherence. 2015;9:649–658. | ||
van der Pol M, Hennessy D, Manns B. The role of time and risk preferences in adherence to physician advice on health behavior change. The European Journal of Health Economics. 2017;18(3):373–386. | ||
Shuval K, Stoklosa M, Pachucki MC, Yaroch AL, Drope J, Harding M. Economic preferences and fast food consumption in US adults: Insights from behavioral economics. Prev Med. 2016;93:204–210. | ||
Broadbent E, Donkin L, Stroh JC. Illness and treatment perceptions are associated with adherence to medications, diet, and exercise in diabetic patients. Diabetes Care. 2011;34(2):338–340. | ||
Wu SF, Courtney M, Edwards H, Mcdowell J, Shortridge-Baggett LM, Chang PJ. Self-efficacy, outcome expectations and self-care behaviour in people with type 2 diabetes in Taiwan. J Clin Nurs. 2007;16(11C):250–257. | ||
Williams KE, Bond MJ. The roles of self-efficacy, outcome expectancies and social support in the self-care behaviours of diabetics. Psychol Health Med. 2002;7(2):127–141. | ||
Gibson B, Yingling L, Bednarchuk A, Janamatti A, Oakley-Girvan I, Allen N. An Interactive Simulation to Change Outcome Expectancies and Intentions in Adults With Type 2 Diabetes: Within-Subjects Experiment. JMIR Diabetes. 2018;3(1):e2. | ||
Grossman M. On the Concept of Health Capital and the Demand for Health. J Polit Econ. 1972;80(2):223–255. | ||
McGuire A, Henderson J, Mooney G. The Economics of Health Care: An Introductory Text. New York, NY: Routledge & Keagan Paul; 1988. | ||
Arnold-Wörner N, Holle R, Rathmann W, Mielck A. The importance of specialist treatment, treatment satisfaction and diabetes education for the compliance of subjects with type 2 diabetes – results from a population-based survey. Exp Clin Endocrinol Diabetes. 2008;116(2):123–128. | ||
Chapman GB, Elstein AS. Valuing the future: temporal discounting of health and money. Med Decis Making. 1995;15(4):373–386. | ||
Cutler DM, Glaeser E. What explains differences in smoking, drinking, and other health-related behaviors? Am Econ Rev. 2005;95(2):238–242. | ||
RStudio Team. RStudio: integrated Development for R [computer program]. Boston, MA: RStudio, Inc.; 2015. | ||
Takagi D, Kondo N, Takada M, Hashimoto H. Educational attainment, time preference, and health-related behaviors: A mediation analysis from the J-SHINE survey. Soc Sci Med. 2016;153:116–122. | ||
Sen AP, Sewell TB, Riley EB, et al. Financial incentives for home-based health monitoring: a randomized controlled trial. J Gen Intern Med. 2014;29(5):770–777. | ||
Gopalan A, Paramanund J, Shaw PA, et al. Randomised controlled trial of alternative messages to increase enrolment in a healthy food programme among individuals with diabetes. BMJ Open. 2016;6(11):e012009. | ||
Dai H, Mao D, Volpp KG, et al. The effect of interactive reminders on medication adherence: A randomized trial. Prev Med. 2017;103:98–102. | ||
Kessler JB, Troxel AB, Asch DA, et al. Partners and Alerts in Medication Adherence: A Randomized Clinical Trial. J Gen Intern Med. 2018:1–7. |
Supplementary materials
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.