Back to Journals » Vascular Health and Risk Management » Volume 19
Thromboembolism and Major Bleeding in Patients with Atrial Fibrillation and EHRA Type 2 Valvular Heart Disease: The Jordan Atrial Fibrillation (JoFib) Study
Authors Al-Najar M, Al-Nusair M , Alrabadi N, Alawaisheh I, Alawaisheh T , Jarrah M , Alzoubi KH , Njem S, Hamoudeh A
Received 31 August 2022
Accepted for publication 9 March 2023
Published 18 March 2023 Volume 2023:19 Pages 145—155
DOI https://doi.org/10.2147/VHRM.S387477
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Pietro Scicchitano
Mahasen Al-Najar,1 Mohammed Al-Nusair,2 Nasr Alrabadi,3 Ibrahim Alawaisheh,4 Tuqa Alawaisheh,4 Mohamad Jarrah,5 Karem H Alzoubi,6,7 Sumaya Njem,3 Ayman Hamoudeh8
1Department of Radiology, Faculty of Medicine, The University of Jordan, Amman, Jordan; 2Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan; 3Department of Pharmacology, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan; 4Faculty of Medicine, The University of Jordan, Amman, Jordan; 5Division of Cardiology, Department of Internal Medicine, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan; 6Department of Pharmacy Practice and Pharmacotherapeutics, University of Sharjah, Sharjah, United Arab Emirates; 7Department of Clinical Pharmacy, Faculty of Pharmacy, Jordan University of Science and Technology, Irbid, Jordan; 8Cardiology Department, Istishari Hospital, Amman, Jordan
Correspondence: Mohamad Jarrah; Nasr Alrabadi, Correspondence: Tel +962795994247, Email [email protected]; [email protected]
Aim: The risks of thromboembolism and major bleeding in atrial fibrillation (AF) patients were assessed according to the “Evaluated Heartvalves, Rheumatic or Artificial” (EHRA) classification. Additionally, the safety and efficacy of vitamin K antagonists (VKAs) and non-VKA oral anticoagulants (NOACs) were compared in AF patients with EHRA type 2 valvular heart disease (VHD) versus those with no VHD.
Methods: AF patients enrolled in the “Jordan Atrial Fibrillation (JoFib)” study were followed up for thromboembolic events and major bleeding at 30, 180, and 365 days. Patients in the EHRA type 2 VHD and non-VHD groups were sub-grouped to compare different OACs.
Results: 2020 AF patients were recruited. The thromboembolic risk was higher in EHRA type 2 VHD patients compared to non-VHD controls. Major bleeding also occurred at higher rates in EHRA type 2 patients. In addition, NOACs were more effective in preventing thromboembolic events than VKAs and non-anticoagulation in EHRA type 2 VHD patients. Furthermore, EHRA type 2 VHD patients taking rivaroxaban had significantly less thromboembolic risk than their non-anticoagulated counterparts. At the same time, apixaban and warfarin did not significantly lower the risk of thromboembolism compared to non-anticoagulation.
Conclusion: AF patients with EHRA type 2 VHD are at significant risk of thromboembolism and major bleeding. Furthermore, NOACs were more effective than VKAs in preventing thromboembolic events in this group of patients without conferring an added risk of major bleeding. Moreover, rivaroxaban appears to be particularly efficacious.
Keywords: thromboembolism, bleeding, atrial fibrillation, EHRA type 2 valvular heart disease, Jordan
Introduction
Atrial fibrillation (AF) is a well-established risk factor for thromboembolism and an essential indication for oral anticoagulation (OAC),1,2 conferring a severe risk of bleeding.3 Valvular heart disease (VHD) is independently associated with AF.1 It is an independent cause of mortality and morbidity associated with thromboembolic and bleeding events, irrespective of underlying cardiac rhythm.4,5 AF patients have historically been dichotomized as “valvular” AF or “nonvalvular” AF. However, clinical definitions of these terms have been conflicting, causing confusion among researchers and practitioners.6,7 As an antidote to this uncertainty, a new functional classification of AF patients with VHD, based on OAC therapy, was proposed: the “Evaluated Heartvalves, Rheumatic or Artificial” (EHRA) classification, which categorized patients as 1) EHRA type 1 VHD, corresponding to AF patients with “VHD needing therapy with a vitamin K antagonist (VKA)”, which include mitral stenosis (moderate to severe, of rheumatic origin) and mechanical prosthetic valve replacement; and 2) EHRA type 2 VHD, which refers to AF patients with “VHD needing therapy with a VKA or a non-VKA oral anticoagulant (NOAC)”, which generally include any other VHD, bioprosthetic valve replacement, valve repair or transcatheter aortic valve implantation (TAVI).8
Thromboembolic risk in AF patients with concurrent mitral stenosis or mechanical prosthetic valve (EHRA type 1 VHD) is well established, prompting guidelines to recommend anticoagulation with VKAs. In contrast, thromboembolic risk in the heterogeneous EHRA type 2 VHD group is not as certain, and guidelines recommend anticoagulation by the CHA2DS2VASc score.8 Recent studies have indicated an increased risk of thromboembolism and major bleeding in AF patients with EHRA type 2 VHD compared to AF patients with no documented VHD. However, this may be explained by the greater number of risk factors and comorbidities in the former group, reflected by a higher CHA2DS2VASc score.9,10
Several studies have compared the safety and effectiveness of NOACs and VKAs in managing AF patients with EHRA type 2 VHD. They have generally demonstrated comparable outcomes regarding thromboembolism and major bleeding, with some suggesting a more favorable profile of NOACs, not to mention the added benefits of fewer side effects, more rapid pharmacokinetic effects, and less monitoring.11–16 Furthermore, recent guidelines have recommended using NOACs over warfarin in AF patients without moderate-severe mitral stenosis or a mechanical heart valve, including those with EHRA type 2 VHD.17
In this study, the risk of thromboembolism and major bleeding according to the new EHRA valve classification was assessed in a Jordanian population of AF patients from the national multicenter AF registry. In addition, the risks of thromboembolism and major bleeding were compared between patients taking VKAs and patients taking NOACs within an EHRA type 2 VHD subpopulation and within a subpopulation of patients with no documented VHD.
Methods
Study Population and Design
This study included patients enrolled in the “Jordan Atrial Fibrillation (JoFib)” study, a national multicenter observational registry of AF patients sequentially recruited from 18 hospitals and 11 outpatient cardiology clinics throughout Jordan. Inclusion criteria were diagnosis of AF confirmed by 12-lead electrocardiogram (EKG), rhythm strip lasting ≥30 seconds, ≥1 episode of AF on an ambulatory EKG monitor, or a past diagnosis by a treating cardiologist. Patients were assessed for the primary outcomes of thromboembolism, defined as ischemic stroke (thrombotic or embolic stroke) or systemic embolism, and major bleeding, defined as intracranial hemorrhage, bleeding requiring hospitalization, bleeding leading to a drop in hemoglobin concentration greater than 2g/dL or bleeding requiring blood transfusion, at 1, 6 and 12 months of follow-up.18 Patients who refused to sign the study consent form without sufficient data or records for the whole period were excluded.
Using specialist face-to-face interviews and laboratory records, data were collected at the entry visit and included clinical and demographic profiles, laboratory findings, transthoracic echocardiographic features, and data on OAC use and other medications. The follow-up data were collected using face-to-face interviews, laboratory records, and phone calls when appropriate. CHA2DS2VASc and HAS-BLED scores were calculated for each patient at baseline.
The study population of AF patients was divided into three groups based on EHRA VHD classification as follows: 1) EHRA type 1 VHD, defined as a diagnosis/procedural code of moderate-to-severe mitral stenosis or metallic prosthetic valve; 2) EHRA type 2 VHD, defined as any other VHD, including a diagnosis/procedural code of aortic stenosis or regurgitation, mitral regurgitation, TAVI or other valve diseases/procedures (tricuspid regurgitation/stenosis, pulmonic regurgitation/stenosis, bioprosthetic valve replacement); and 3) Non-VHD controls, defined as AF patients with no diagnosis/procedural code of any VHD nor prosthetic heart valve or valve repair. Patients diagnosed with EHRA type 1 VHD and type 2 VHD were classified as EHRA type 1 VHD.
Statistical Analysis
Comparisons between groups were made using chi-square tests to compare categorical variables, described as percentages, and one-way ANOVA tests for continuous variables described using means and standard deviations (SD).
Using cox proportional hazards models, time-to-event analysis was applied to describe the association between EHRA classification and the risk of thromboembolism and major bleeding. Time at risk was measured from the entry visit date until an event of thromboembolism or major bleeding, death, change in anticoagulation status (starting anticoagulation therapy, discontinuing anticoagulation, switching from one medication to another, or changing dose), emigration, end of follow-up or end of the study, whichever occurred first. Data on the time at which failure and censoring events had occurred were accurate to the day of follow-up except for the change in anticoagulation status, which was expressed as having occurred during 0–30 days of follow-up, 31–180 days of follow-up, or 181–365 days of follow-up. Since the number of patients that experienced a change in anticoagulation status was relatively small, we estimated that the change occurred at 15, 105, or 272 days, respectively. Time at risk was measured separately for each event of interest (thromboembolism or major bleeding); thus, patients were followed until the event of interest (or a censoring event, eg, death) and were allowed to experience a thromboembolic event before the bleeding event, and vice versa. The proportional hazards assumption was tested by running a cox regression analysis with time-dependent variables. The results were expressed as hazard ratios (HR) and 95% confidence intervals (CI).
Subgroup analysis was performed on EHRA type 2 and non-VHD patients according to OAC therapy to describe the association between OAC class and thromboembolic and major bleeding risk within AF patients with EHRA type 2 VHD and AF patients with no VHD. Two sets of analyses were performed for each group: one comparing NOACs and VKAs, and a second comparing individual drugs. Time-to-event analysis was performed as described above. Subgroup analysis was not performed for EHRA type 1 patients because most of these patients were taking Warfarin, and too few patients were taking NOACs or were non-anticoagulated for a reliable risk estimate to be obtainable. A p-value <0.005 was considered statistically significant. IBM SPSS Statistics for Windows, version 26 (IBM Corp., Armonk, NY, USA) was used for statistical analysis.
Ethical Considerations
All relevant study documentation and amendments were approved by the institutional review board of Jordan University of Science and Technology and registered at the ClinicalTrials.gov with reference number: NCT03917992. Written informed consents were obtained from all study participants.
Results
A total of 2020 patients with AF were included in this study. Of them, 170 (8.4%) had EHRA type 1 VHD defined as moderate-to-severe mitral stenosis of rheumatic origin (66, 3.3%) or mechanical prosthetic valve (104, 5.1%); 339 (16.8%) had EHRA type 2 VHD defined as any other VHD including moderate-to-severe mitral regurgitation, moderate-to-severe aortic regurgitation, moderate-to-severe tricuspid regurgitation, and TAVI; and 1511 (74.8%) had no VHD. Descriptive statistics for these patients are provided in Table 1. Notably, AF patients with EHRA type 2 VHD were older and had higher mean CHA2DS2VASc and HAS-BLED scores than patients with EHRA type 1 VHD or no VHD. On the other hand, EHRA type 1 patients were more commonly female and more likely to have permanent AF than other patients.
 |
Table 1 Characteristics of AF Patients According to EHRA Classification |
Regarding medical therapy, EHRA type 1 patients were more frequently prescribed anticoagulants (96.5%) and beta-blockers (84.7%), while type 2 patients more commonly received angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers (43.7%) and diuretics (53.7%).
Thromboembolism
Of the 2020 patients enrolled in the JoFib registry, 74 patients had no follow-up data and were excluded from time-to-event analyses. There were 77 thromboembolic events in total. The rate of thromboembolic events for AF patients was significantly higher (1.954, 95% CI: 1.19–3.22, p=0.008) in EHRA type 2 than in non-VHD controls (p=0.007 for overall Log rank test; p=0.023 for type 2 vs 1, p=0.216 for type 1 vs non-VHD controls (Figure S1, Supplementary files). After adjustment for age, sex, anticoagulation, antiplatelet therapy, and comorbid diseases (heart failure, hypertension, diabetes, previous thromboembolic event, and coronary artery disease), a statistically significant difference between the three groups persisted with EHRA type 2 predisposing to thromboembolism (Figure 1). Multivariable analysis also identified increasing age, history of thromboembolism, and diabetes as independent predictors of future thromboembolism. Interestingly, when adjusted for anticoagulation at baseline and CHA2DS2VASc score, AF patients with EHRA type 2 VHD remain at a statistically significant higher risk of thromboembolism than non-VHD AF controls (1.755 (95% CI: 1.066–2.890, p=0.027). Increasing the CHA2DS2VASc score was also identified as an independent risk factor for thromboembolic events.
 |
Figure 1 Thromboembolism survival curve, adjusted, in AF patients according to EHRA VHD classification; 1946 patients, and 77 events. |
Major Bleeding
A total of 49 major bleeding events occurred during the 12 months of follow-up. The risk of major bleeding in AF patients was significantly higher (2.207, 95% CI: 1.17–4.18, p=0.015) among those classified under EHRA type 2 VHD than those with no VHD (p=0.034 for the overall Log Rank test, p=0.800 for type 1 vs non-VHD, p=0.137 for type 1 vs type 2 (Figure S2, Supplementary files). After adjustment for age, sex, anticoagulation, antiplatelet use, baseline INR >3, and comorbidities including hypertension, chronic kidney disease, and previous stroke, no significant difference in major bleeding risk was observed between the three groups (Figure 2). In addition, increasing age, baseline INR >3 and increasing HAS-BLED score were identified as independent risk factors for major bleeding.
 |
Figure 2 Major bleeding survival curve, adjusted, in AF patients according to EHRA VHD classification; 1946 patients and 46 events. |
OAC Sub-Analysis
Descriptive statistics regarding OAC in AF patients are provided in Table 2. Briefly, EHRA type 1 patients were more frequently anticoagulated (96.5%) than other groups. Warfarin was the most used anticoagulant in EHRA type 1 patients (87.1%). At the same time, NOACs were more commonly used in EHRA type 2 and non-VHD patients (48.4% and 51.6%, respectively), with Rivaroxaban being the most common NOAC (26.0% and 25.1%, respectively).
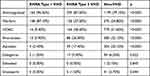 |
Table 2 OAC in AF Patients According to EHRA Classification |
Subgroup analysis according to OAC was performed separately in EHRA type 2 VHD patients and non-VHD patients. Two sets of analyses were conducted in each group. In the first, three subgroups of patients were compared (patients taking NOACs, patients taking warfarin, and non-anticoagulated patients). In the second subgroup analysis, we sought to compare individual anticoagulant drugs. Six anticoagulants were identified in the population of AF patients, warfarin, rivaroxaban, apixaban, dabigatran, edoxaban, and enoxaparin. Patients taking dabigatran and edoxaban were not present in numbers sufficient to obtain a reliable risk estimate and thus were excluded from the second subgroup analysis. Since enoxaparin, low-molecular-weight heparin, is administered subcutaneously, it is, by definition, not an OAC; therefore, patients taking enoxaparin were excluded from all OAC subgroup analyses. Finally, four subgroups were compared in the second analysis (patients taking warfarin, patients taking rivaroxaban, patients taking apixaban, and non-anticoagulated patients). Of the 1946 AF patients with follow-up data, 41 took subcutaneous enoxaparin and were excluded from OAC subgroup analyses.
AF patients with EHRA type 2 VHD taking NOACs were at a significantly lower risk of thromboembolism compared to non-anticoagulated patients and those taking warfarin (0.213 (95% CI: 0.06–0.74), p=0.015; 0.314, 95% CI: 0.11–0.89, p=0.030, respectively (Figure S3, Supplementary files). This persisted after adjustment for age, sex, antiplatelet therapy, and comorbidities (hypertension, diabetes, previous thromboembolic event, coronary artery disease, and heart failure (Figure 3). There was no significant difference in major bleeding risk between patients on NOACs, warfarin and non-anticoagulated patients (Figure 4). In AF patients with no VHD, no statistically significant difference was found between the NOACs, warfarin, and non-anticoagulated groups regarding thromboembolic or major bleeding risk (Figures S4 and S5, Supplementary files).
 |
Figure 3 Thromboembolism survival curve, adjusted, in AF patients with EHRA type 2 VHD according to OAC; 325 patients, and 22 events. |
 |
Figure 4 Major bleeding survival curve in AF patients with EHRA type 2 VHD according to OAC; 325 patients, and 14 events comparison among patients on NOACs, warfarin, and non-anticoagulated patients. |
Among AF patients with EHRA type 2 VHD, rivaroxaban therapy was associated with significantly less risk of thromboembolism compared to non-anticoagulated patients (0.15 (95% CI: 0.029–0.775), p=0.024), while warfarin and apixaban were not associated with a statistically significant risk reduction (Figure 5). No statistically significant risk of major bleeding was found in any of the three OAC subgroups (Figure S6, Supplementary files). In non-VHD patients, neither rivaroxaban, apixaban, or warfarin was significantly protective or predictive of thromboembolism or major bleeding (Figures S7 and S8, Supplementary files).
Discussion
In this study, AF patients categorized according to the EHRA VHD classification were shown to be associated with different risk profiles. Specifically, patients with EHRA type 2 VHD were at higher risk of thromboembolism and major bleeding than AF patients with no VHD. Interestingly, thromboembolic risk persisted after adjusting for possible confounders. Whether such findings are due to random chance, reflect a potential risk inherent in the physiology of the valvular diseases, or can be explained by unidentified confounding factors, remains unknown. Notably, the EHRA type 2 VHD group had a significantly higher mean CHA2DS2VASc score, which may help explain this finding even after adjustment. Of note, these findings contrast with previous studies, where the greater thromboembolic risk associated with EHRA type 2 VHD status was no longer significant following adjustment for possible confounding risk factors, which was explained by the older age and larger number of comorbidities in the EHRA type 2 VHD group, reflected by a greater CHA2DS2VASc score.9,10 On the other hand, the risk of major bleeding in EHRA type 2 patients became nonsignificant following adjustment, which could be explained by the higher HAS-BLED score and the number of patients taking OACs in this group. This was unlike what was observed by Bisson et al, who described a persistent, significantly increased risk of major bleeding in patients with EHRA type 2 VHD. However, they also observed higher mean HAS-BLED scores and/or OAC and postulated that these would be possible explanations.9 Moreover, EHRA type 1 patients had a nonsignificantly lower risk of thromboembolism than non-VHD patients, which may be due to a higher percentage of anticoagulated patients in the former group, reaching 96.5%. This, however, is in line with the findings described by Bisson et al.9
The risk of thromboembolism and major bleeding in patients with EHRA type 2 VHD and patients without VHD were separately analyzed according to OAC therapy. In EHRA type 2 patients, an independent significantly lower risk of thromboembolism was detected in patients taking NOACs compared to those taking VKAs or no OAC. This corresponds with what was reported in previously published meta-analyses.11–13 Specifically, compared to nonanticoagulated patients, rivaroxaban was found to be more effective in preventing thromboembolic events than apixaban or warfarin. In a retrospective analysis of the large randomized trial Rivaroxaban Once Daily Oral Direct Factor Xa Inhibition Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation (ROCKET AF) that compared warfarin and rivaroxaban in “nonvalvular” AF patients, which included EHRA type 2 VHD and non-VHD patients, Breithardt et al found a similar efficacy for preventing thromboembolic events of rivaroxaban and warfarin in AF patients with EHRA type 2 VHD.19 On the other hand, recent studies comparing NOACs and warfarin have found no significant difference in thromboembolic risk among AF patients with EHRA type 2 VHD.15,16 Melgaard et al even found a greater risk of thromboembolism in AF patients with aortic stenosis treated with NOACs than those treated with warfarin.14 Our study observed no significant difference in thromboembolic risk between non-VHD patients taking NOACs, warfarin, or no OAC. Interestingly, the thromboembolic risk was higher in both anticoagulated groups, which may be due to a significantly higher mean CHA2DS2VASc score in these two groups compared to the nonanticoagulated group.
This study found no significant differences in major bleeding risk among EHRA type 2 patients or non-VHD patients, anticoagulated with NOACs or warfarin or not anticoagulated. This is comparable to what was described in other recent studies.11,12,15,16 Conversely, Melgaard et al reported a significantly lower risk of major bleeding in aortic stenosis patients with AF and EHRA type 2 VHD treated with NOACs than warfarin.14 Interestingly, Malik et al demonstrated an increased risk of intracranial hemorrhage and major bleeding in AF patients with EHRA type 2 VHD taking rivaroxaban compared to other NOACs. They also identified a reduced risk with edoxaban.12 Our study found no significant difference in major bleeding between rivaroxaban, apixaban, and warfarin in patients with EHRA type 2 VHD or no VHD.
In general, it appears that NOACs could be a safe and effective alternative to VKAs in the management of AF patients with EHRA type 2 VHD. Considering the added benefits of more rapid pharmacokinetic effects and less requirement for monitoring, it may be the better choice. Accordingly, recent guidelines have recommended it over VKAs in this population of AF patients and those with no VHD.17
In comparison to the current study, a recent study was conducted in Turkey showed the most common comorbid diseases with atrial fibrillation were chronic kidney disease (69%) and hypertension (65.5%). This study demonstrated that most of the non-valvular atrial fibrillation patients are in the high-risk group.20 This was considered the reason for switching from warfarin to new oral anticoagulant therapies.20
Limitations
This study was based on registry data and is liable to limitations intrinsic to retrospective observational analyses. The study population was not ethnically diverse, and our results may not be generalizable to other populations. However, our results were comparable with those of studies conducted on different ethnic populations. The registry data used in this study did not contain data on VHD severity, which may influence thromboembolic risk. Thus, we could not investigate the effect of VHD severity on thromboembolic and major bleeding risks. We can only estimate the risk of ischemic stroke with some uncertainty, as our definition of ischemic stroke included patients with unspecified stroke, as most strokes are ischemic in origin. In addition, some patients may have suffered fatal strokes and never made it to the hospital. Data regarding risk factors for thromboembolism and major bleeding were collected at the entry visit. Similarly, CHA2DS2VASc and HAS-BLED scores were calculated at baseline. However, the dynamic population of AF patients, many of whom are elderly and with multiple comorbidities, may acquire risk factors with time, giving them new scores. Still, a change in anticoagulation status is likely to reflect a change in risk status. Since we censored patients who experienced a change in anticoagulation, we likely censored patients who developed new risk factors, such as fluctuations in drug concentration and response, as no monitoring was strictly conducted for those patients. However, our estimation of when a change in anticoagulation status occurred is not as accurate as other failure or censoring events, which were accurate to the follow-up day. In contrast, the change in anticoagulation status was described as either between 0 and 30 days of follow-up, 31 to 180 days of follow-up, or 181 to 365 days of follow-up. Yet, since the number of patients who experienced a change in anticoagulation status was relatively small, we believe our estimation of the date of anticoagulation status change (15, 105, or 272 days of follow-up) to be reasonable. Finally, numerous variables were to be considered, and we may have overlooked confounding factors affecting the value of multivariable statistical analysis.
Conclusion
Current observations suggest that AF patients with EHRA type 2 VHD are at significant risk of thromboembolism and major bleeding. Furthermore, NOACs were found to be more effective than VKAs in preventing thromboembolic events in this group of patients without conferring an added risk of major bleeding. Moreover, rivaroxaban appears to be particularly efficacious. Therefore, NOACs, particularly rivaroxaban, can potentially replace VKAs as a preferable choice of therapy in this group of patients. Further studies are needed to establish such a practice.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author (MA) upon reasonable request. No individual deidentified participant data will be shared.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021;42(5):373–498. doi:10.1093/eurheartj/ehaa612
2. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22(8):983–988. doi:10.1161/01.str.22.8.983
3. Chao T-F, Lip GYH, Lin Y-J, et al. Incident risk factors and major bleeding in patients with atrial fibrillation treated with oral anticoagulants: a comparison of baseline, follow-up and delta HAS-BLED scores with an approach focused on modifiable bleeding risk factors. Thromb Haemost. 2018;118(04):768–777. doi:10.1055/s-0038-1636534
4. Petty GW, Khandheria BK, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Predictors of cerebrovascular events and death among patients with valvular heart disease. Stroke. 2000;31(11):2628–2635. doi:10.1161/01.STR.31.11.2628
5. Melgaard L, Jensen M, Overvad TF, Larsen TB, Lip GYH, Nielsen PB. Thromboembolic and bleeding outcomes in patients with atrial fibrillation and valvular heart disease: a descriptive nationwide cohort study. Int J Clin Pract. 2020;74(10):e13589. doi:10.1111/ijcp.13589
6. Potpara TS, Lip GYH, Larsen TB, et al. Stroke prevention strategies in atrial fibrillation and heart valve abnormalities: perceptions of ‘valvular’ atrial fibrillation: results of the European heart rhythm association survey. EP Eur. 2016;18(10):1593–1598. doi:10.1093/europace/euw302
7. Molteni M, Polo Friz H, Primitz L, Marano G, Boracchi P, Cimminiello C. The definition of valvular and non-valvular atrial fibrillation: results of a physicians’ survey. EP Eur. 2014;16(12):1720–1725. doi:10.1093/europace/euu178
8. Lip GYH, Collet JP, Caterina R, et al. Antithrombotic therapy in atrial fibrillation associated with valvular heart disease: a joint consensus document from the European Heart Rhythm Association (EHRA) and European society of cardiology working group on thrombosis, endorsed by the ESC working. EP Eur. 2017;19(11):1757–1758. doi:10.1093/europace/eux240
9. Bisson A, Bodin A, Clementy N, et al. Stroke, thromboembolism and bleeding in patients with atrial fibrillation according to the EHRA valvular heart disease classification. Int J Cardiol. 2018;260:93–98. doi:10.1016/j.ijcard.2018.03.017
10. Philippart R, Brunet-Bernard A, Clementy N, et al. Prognostic value of CHA2DS2-VASc score in patients with ‘non-valvular atrial fibrillation’ and valvular heart disease: the Loire valley atrial fibrillation project. Eur Heart J. 2015;36(28):1822–1830. doi:10.1093/eurheartj/ehv163
11. He Q, Sze C-Y, Shum T-Y, et al. Comparing clinical outcomes of NOACs with warfarin on atrial fibrillation with valvular heart diseases: a meta-analysis. BMC Cardiovasc Disord. 2019;19(1):113. doi:10.1186/s12872-019-1089-0
12. Malik AH, Yandrapalli S, Aronow WS, Panza JA, Cooper HA. Oral anticoagulants in atrial fibrillation with valvular heart disease and bioprosthetic heart valves. Heart. 2019;105(18):1432LP–1436 . doi:10.1136/heartjnl-2019-314767
13. de Souza Lima Bitar Y, Neto MG, Filho JAL, et al. Comparison of the new oral anticoagulants and warfarin in patients with atrial fibrillation and valvular heart disease: systematic review and meta-analysis. Drugs R D. 2019;19(2):373–498. doi:10.1007/s40268-019-0274-z
14. Melgaard L, Overvad TF, Jensen M, et al. Effectiveness and safety of NOAC versus warfarin in patients with atrial fibrillation and aortic stenosis. J Am Heart Assoc. 2021;10(23):e022628. doi:10.1161/JAHA.121.022628
15. Strange JE, Sindet-Pedersen C, Staerk L, et al. All-cause mortality, stroke, and bleeding in patients with atrial fibrillation and valvular heart disease. Eur Heart J Cardiovasc Pharmacother. 2021;7(FI1):f93–f100. doi:10.1093/ehjcvp/pvaa011
16. Li H-J, Lin S-Y, Lin F-J, Hung C-S, Wang -C-C. Effectiveness and safety of non-vitamin K antagonist oral anticoagulants in Asian patients with atrial fibrillation and valvular heart disease. Curr Med Res Opin. 2021;37(4):535–542. doi:10.1080/03007995.2021.1885365
17. January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American college of cardiology/American heart association task force on clinical practice guidelines and the heart R. J Am Coll Cardiol. 2019;74(1):104–132. doi:10.1016/j.jacc.2019.01.011
18. Schulman S, Kearon C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3(4):692–694. doi:10.1111/j.1538-7836.2005.01204.x
19. Breithardt G, Baumgartner H, Berkowitz SD, et al. Clinical characteristics and outcomes with rivaroxaban vs. warfarin in patients with non-valvular atrial fibrillation but underlying native mitral and aortic valve disease participating in the ROCKET AF trial. Eur Heart J. 2014;35(47):3377–3385. doi:10.1093/eurheartj/ehu305
20. Güzel T, Aktan A, Kılıç R, et al. Oral anticoagulant use and long-term follow-up results in patients with non-valvular atrial fibrillation in Turkey AFTER-2 study. Anatol J Cardiol. 2022;26(7):567–576. doi:10.5152/AnatolJCardiol.2022.1597
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

