Back to Journals » Psoriasis: Targets and Therapy » Volume 12
Therapeutic Inertia in the Management of Psoriasis: A Quantitative Survey Among Indian Dermatologists and Patients
Authors Rajagopalan M, Dogra S , Godse K, Kar BR, Kotla SK, Neema S, Saraswat A , Shah SD, Madnani N, Sardesai V, Sekhri R, Varma S, Arora S, Kawatra P
Received 24 May 2022
Accepted for publication 3 August 2022
Published 25 August 2022 Volume 2022:12 Pages 221—230
DOI https://doi.org/10.2147/PTT.S375173
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Uwe Wollina
Murlidhar Rajagopalan,1 Sunil Dogra,2 Kiran Godse,3 Bikash Ranjan Kar,4 Sai Krishna Kotla,5 Shekhar Neema,6 Abir Saraswat,7 Swapnil Deepak Shah,8 Nina Madnani,9,10 Vidyadhar Sardesai,11 Rajiv Sekhri,12 Sachin Varma,13 Sandeep Arora,14 Pallavi Kawatra15
1Department of Dermatology, Apollo Hospital, Chennai, India; 2Department of Dermatology Venereology & Leprology Postgraduate Institute of Medical Education & Research (PGIMER), Chandigarh, 160012, India; 3DY Patil University School of Medicine, Navi Mumbai, India; 4Department of Dermatology, IMS and SUM Hospital, Bhubaneshwar, Odisha, India; 5Department of Dermatology, Yashodha Hospital, Secunderabad, India; 6Department of Dermatology, Armed Forces Medical College, Pune, Maharashtra, India; 7Indushree Skin Clinic, Lucknow, India; 8Department of Dermatology, Ashwini Rural Medical College, Solapur, India; 9Hinduja Hospital, Mumbai, India; 10Sir. H. N. Reliance Hospital, Mumbai, India; 11Bharati Vidyapeeth Medical College, Pune, India; 12Fortis Hospital, Noida, India; 13Skinvita Clinic, Kolkata, West Bengal, India; 14Army College of Medical Sciences, New Delhi, India; 15Novartis, Mumbai, India
Correspondence: Murlidhar Rajagopalan, Department of Dermatology, Apollo Hospital, Chennai, India, Email [email protected]
Purpose: The primary objective of the study was to understand the therapeutic inertia in treatment and management of plaque psoriasis among dermatologists, along with determining the preferred treatment choices for management of plaque psoriasis; it also included the resulting treatment satisfaction among patients. The secondary objective was to identify the gaps in terms of knowledge and attitude among dermatologists and the expectations of patients.
Patients and Methods: A multicentre, cross-sectional quantitative survey was conducted among dermatologists and patients with moderate to severe plaque psoriasis across India. The interviews were conducted either face to face or via telephone between September and November 2020, using structured and validated questionnaires based on specific themes. The data obtained were statistically analysed, wherever applicable.
Results: Overall, 207 adult patients with moderate-to-severe plaque psoriasis and 303 dermatologists were interviewed. Post experiencing symptoms, 44% of the patients visited general physicians for treatment and there was an average 7.8-month delay by the patients to consult a dermatologist. Approximately one-fourth of patients used home remedies before seeking medical help. One-third of dermatologists used the Psoriasis Area and Severity Index (PASI) for assessing the disease severity. Majority of dermatologists preferred combination therapy for their patients. The lack of quick resolution and side effects were the major reasons for changing the treatment. Overall, only 35% of the patients complied to current treatment. Satisfaction with existing forms of therapies was highest for mild plaque psoriasis (62%) as confirmed by dermatologists, while 52% of the overall patients were satisfied with their therapy. Majority of the patients (64%) affirmed living with plaque psoriasis impacted their lives.
Conclusion: This first-of-its-kind survey in India highlighted the gaps in terms of the disease journey between dermatologists and patients. The survey emphasises the need for shared decision-making and may benefit dermatologists in suggestive modifications of the treatment algorithm and disease management in clinical settings.
Keywords: therapeutic inertia, psoriasis, adherence, treatment expectations, treatment goals, diagnosis
Introduction
Psoriasis is a chronic inflammatory condition with genetic basis that affects the skin and joints, with various systemic associations.1 Recent evidence indicates that the global prevalence of psoriasis varies from 0.14% to 1.99%.2 According to global psoriasis atlas (GPA) data, an estimated 3.59 million people in India are affected by psoriasis,3 with prevalence ranging between 0.44% and 2.8%.4,5 Patients with psoriasis report symptoms such as itching, pain, and flaky skin.6 The overall quality of life (QoL) of patients with psoriasis is significantly impacted due to disease severity, gender, age, anatomical sites of lesion, and involvement of comorbidity;7–9 leading to multifaceted effects on patients life including social exclusion, discrimination, physical and psychological well-being, and loss of productivity.10–21
Patients with psoriasis are categorised as mild, moderate and severe based on the severity of disease and percentage of body surface affected.22 The treatment for psoriasis is generally a long-term therapy wherein patients with moderate-to-severe psoriasis need systemic treatment (such as methotrexate, acitretin & biologics), whereas for mild psoriasis, topical medications (such as corticosteroids and vitamin D3 analogues) and phototherapy are generally preferred. The long-term use of conventional systemic therapy is restricted due to poor tolerability and cumulative toxicity.23,24 Additionally, the global use of biologics has followed an increasing trend in the recent years.23,25–27 However, in the Indian context, the applicability is still restricted with the proposed ranking of biologics (available in India) in terms of efficacy being secukinumab, adalimumab/infliximab, and etanercept.28
In the real-world study by Armstrong et al, patients affirmed highest effectiveness with the use of biologics (73%), with up to a 55% adherence. However, median treatment duration and high side effects were the major causes for discontinuation of biologics.29 Various studies have established the effectiveness of different conventional therapies and biologics, and improved QoL of the patients.30–33
Enhanced patient communication by the dermatologists is required for the management of psoriasis to improve the overall QoL of the patients.34,35
Patients with psoriasis often do not achieve their target goal of skin clearance, attributed to the lack of initiation/intensification of treatment, which is also known as “therapeutic inertia”.36,37 A French survey reported the extent of therapeutic inertia to be 36% among dermatologists while treating psoriatic patients.38 Unlike poor therapeutic compliance, which is attributed to the attitude of the patient, therapeutic inertia is caused by the attitude of physician. It can lead to a negative impact on the patient’s QoL, treatment adherence and patients being likely to change their physician.39 The main cause for disconnect between patients and dermatologists is plausibly due to the objective approach taken by the dermatologist to determine disease severity compared to the subjective manner by which an individual experiences and monitors his/her disease symptoms.36 However, there is a lack of India-specific evidence to understand this concept and its impact in the management of psoriasis.
A quantitative survey was conducted with the primary objective to understand the therapeutic inertia in treatment and management of plaque psoriasis among dermatologists, along with determining the preferred treatment choices for management of plaque psoriasis; it also included the resulting treatment satisfaction among patients. The secondary objective was to identify the gaps in terms of knowledge and attitude among dermatologists and the expectations of patients. The research question with respect to the dermatologists included mapping the patient journey, evaluating the need for treatment and treatment algorithm, factors influencing choice of therapy, barriers for aggressive treatment, and the current unmet needs. Similarly, the research questions for patients were pertaining to the patient experience, impact on personal, professional, and social lives, expectations from treatment, current level of satisfaction and need gaps, and patient’s role in treatment decision.
Materials and Methods
Survey Design
A multicentre non-interventional, cross-sectional, quantitative survey was conducted among patients with plaque psoriasis and dermatologists; the recruitment was performed based on the screener questions. A sample size of 303 dermatologists was estimated for the study across geographical zones (North, East, West, South), biologics usership (user, non-user), practice setting (private [n=250] vs public [n=53]), experience (3–50 years) and patient load (average of 250 patients per month, with at least 50 psoriasis patients) with confidence interval and margin of error to get a statistically valid sample. Similarly, a sample size of 207 patients was estimated across geographical zones, biologic usership (user, non-user), gender (male, female), duration of disease (1–5 years, 6–10 years, >10 years), type of hospital setting (public [42], private [165]), age (18–25, 26–40, >40 years), severity of disease (moderate and severe), Psoriasis Area and Severity Index (PASI) score (≥10) and Body Surface Area (BSA) (≥3%). The dermatologist recruitments were undertaken from September to November 2020, while patient recruitments were done from September to October 2020. To eliminate biases, the dermatologist samples were homogeneously distributed across geographies along with relevant expertise and patient load, while patient samples were distributed across gender and age.
Methodology
The survey was conducted in accordance with Royal Pune Independent Ethics Committee, this is an Independent Ethics Committee-approved protocol registered with the following id: ECR/45/Indt/MH/2013/RR-19. All pertinent guidelines of ICH E6 (R2) Guideline for Good Clinical Practice, ICMR Guidelines (2017) and other regulatory guidelines applicable for such survey programmes have been adhered to. The interviews were conducted by representatives from the contract research organisation IQVIA, using a mix of face-to-face interviews using Computer-Assisted Personal Interviews technique and telephonic methodology due to COVID-19 pandemic. Prior to participation in the survey, participants were given information about the survey and consent forms that were duly obtained.
Data Collection and Analysis
A structured questionnaire was designed and validated by a 13-member panel of dermatology experts to collect information from dermatologists and patients. Post approval of the questionnaire, 30-minute online interviews were performed. The dermatologist’s questionnaire included the following themes: patient load and patient types, mapping the patient journey, evaluating the need for treatment, determining the treatment algorithm and therapy of choice, understanding treatment protocol and goals, understanding healthcare professionals’ experience with injectables, treatment satisfaction and patient follow-up. The patient questionnaire included the following parts: understanding patient experience with the condition; determining impact of the condition on private, professional, and social life; understanding patient reactions, awareness, and goals; understanding treatment journey and drivers for treatment decision. All questionnaires were scrutinised, 30% of them were backchecked, followed by data processing of all questionnaires.
Statistical Analysis
The data were analysed using descriptive analysis, correlation analysis, regression analysis, subgroups analysis (including different zones, gender and public versus private sectors), wherever applicable and is included in the manuscript. Quantum statistical cross-tabulation package was used to run the data tables. The t-test at 95% confidence level was used for significant testing. The independent sample t-test compared differences in continuous measurement from the two groups, and chi-square test was used to assess independence among the two variables. The level of statistical significance was set at p<0.05.
Results
Dermatologist Demographics and Practice Dynamics
A total of 303 dermatologists with a mean experience of 18.8 years were interviewed. Overall, 82.5% (n=250) and 17.4% (n=53) dermatologists were practicing in a private setup and public practice, respectively (Supplementary Table 1).
Dermatologists stated that 47% of the patients received prior treatment and 27% of the patients opted for alternative therapies before consultation. Dermatologists reported that highest proportion of patients get diagnosed at mild stage (46%), followed by severe plaque psoriasis (27%). Approximately one-third of dermatologists used PASI and BSA as the tools to assess disease severity.
Patient Demographics
A total of 207 patients with moderate-to-severe plaque psoriasis were interviewed. Majority of the patients were from metro cities (62.7%, n=129) who visited a private practice setup (79.7%, n=165). Overall, 61.3% (n=127) patients were in the age group of 18–40 years with majority being male patients (60.3%, n=125) (Supplementary Table 2).
Symptoms to Diagnosis
The top three symptoms recalled by the patients at the time of diagnosis were itching (77%; n=159), cracked and dry skin (71%, n=147) and rash (65%, n=135). However, dermatologists recalled patients reporting flaky skin (77%, n=234), cracked and dry skin (76%, n=230) and itching (69%, n=209) (Figure 1).
 |
Figure 1 Overall distribution of the symptoms experienced at the initial diagnosis. More than one option can be selected by the respondents. |
Time Lapse to Seek Medical Help from the Diagnosis
A total 47% (n=97) of the patients reported to have a time-lapse of 1–3 months between experiencing symptoms and seeking medical help with an overall time-lapse of 3.6 months. Female patients reported lesser time-lapse (2.6 months) compared to male patients (4 months).
Nearly 54% of the patients (n=111) reported visiting dermatologists as the initial point of care with a higher number of female patients (66%, n=51) compared to male patients (50%, n=64) (Supplementary Figure 1).
Overall, 26% (n=54) and 14% (n=29) of the patients tried home remedies and alternative therapy, respectively, after experiencing the disease symptoms. Patients >40 years of age exhibited a high preference to try home remedies (36%) compared to young patients (18–25 years) (19%).
Considering the time taken by the referral pathway to be under the care of a dermatologist, there was a time-lapse of 7.8 months. The top two factors considered by the patients before seeking specialist consultation were advice/recommendations from family/friend (64%; n=132) and impact on QoL and daily activities (40%; n=89).
Diagnosis Consultation
Overall length of consultation recalled by the dermatologists was around 22 minutes, whereas the time recalled by the patients was around 29 minutes. Dermatologists in public setup spent lesser time on consultation (18.3 minutes) compared to private setup (23.5 minutes). Both patients and dermatologists acknowledged spending majority of time in counselling, followed by discussion of treatment options (Table 1).
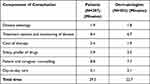 |
Table 1 Distribution of Time Spent in Various Components of Counselling |
Treatment Recommendation and Expectation
Highest disconnect in terms of treatment expectation between patients and dermatologists' perception of patient expectations were observed for side effects profile (29%), complete cure of the disease (27%) and probability of the condition spreading to other parts of body (27%) (Figure 2). Although >50% of the patients expected clear skin and quick resolution, only 19% of the patients were aware of biologics as a treatment option.
 |
Figure 2 Treatment expectations by patients and dermatologists' perspective of patient expectations. |
Overall, 21% (n=63) and 18% (n=54) dermatologists suggested oral and topical therapy, respectively, for moderate plaque psoriasis. Among the current therapies for severe plaque psoriasis, although 49% (n=148) dermatologists gave injectables/biologics in combination with oral therapies with immunosuppressants, topical therapy along with oral therapies with DMARDs/immunosuppressants were recommended by 22% (n=66) dermatologists for severe plaque psoriasis.
Treatment Acceptance, Compliance, and Follow-Up
There was a disconnect between dermatologists (51% [n=154]) and patients (76% [n=157]) in terms of the recommended treatment at the first visit. The west zone had the least resistance (55%) while the east zone had the highest resistance to initiate the therapy (48%). On average, dermatologists reported a 5.5-month window to shift from first- to second-line therapy and an 8.7-month window to shift from second- to third-line therapy. Overall, onset of comorbidities (69%) and no improvement in condition (66%) were the primary reasons to shift the line of therapy.
The fear of side effects (42%; n=87) followed by preference of home remedies and alternative therapies (33%; n=68) were the main reasons for the patients to deny therapy. However, the dermatologists reported need for second opinion (56%; n=169) and home remedies or alternative therapies (54%; n=163) to be the prime reasons for non-acceptance of therapy. Approximately only one third of the patients reported compliance to the current therapy. A total of 56% and 53% dermatologists considered high cost of therapy and low or no immediate relief as the primary reasons for non-compliance.
Frequency of follow-up was 24 days, with an average of 17 minutes of the consultation time. Loss to follow-up was reported in 28% of the patients with moderate plaque psoriasis and 25% of the patients with severe plaque psoriasis.
Treatment Satisfaction
As per the dermatologists, satisfaction to existing therapies were highest in patients with mild plaque psoriasis (62%) and lowest for those with severe plaque psoriasis (5%). Biologics users seemed more satisfied (67%) than non-users (57%). Nearly 52% of the patients were satisfied with the current therapy, with maximum satisfaction reported by biologics users (72%) and 57% confirming on skin clearance results.
Impact on the QoL of Patients
Majority of the patients (64%) affirmed living with plaque psoriasis impacted their lives. Around 31% of the patients reported reduced work productivity, 28% faced unemployment at any stage and 27% could not attend work social events and were allocated tasks requiring lesser social interactions. Overall, 32 working days were lost with 1.6 non-productive hours per working day. Similarly, on a personal front, 27% reported social stigma and 23% of the patients felt being left out socially.
Current Need Gaps
The current need gaps for the dermatologists include treatment satisfaction (reduces significantly as the severity increases), patient compliance (low compliance for biologics attributable to low compliance to high cost, no immediate relief), attitude towards management and improvement areas in management (affordable therapy [25%] and more aggressive therapies required in the initial stages [22%] highlighting the inertia in the treatment). Majority of the dermatologists (64%) opined that they played prominent role in identification, treatment and prevention or treatment of other comorbidities related to psoriasis.
Only one-fourth patients received any kind of support services; hence, they perceived a high need for value-added services. Owing to lack of knowledge and awareness, true compliance was observed only in around 30% of the patients. Other need gaps of the patients included lack of definitive cure (42%), longer remission period (41%), and more time required by dermatologists to listen to patient needs and emotions (38%).
Discussion
Current evidence indicates that undertreatment and dissatisfaction with the treatment are common concerns observed in patients with psoriasis. In a global survey, nearly 25% and 10% of the patients were suffering from mild and severe psoriasis, respectively; 10% of the patients with severe psoriasis were not receiving any treatment, while nearly 50% were dissatisfied with the current treatment.40 This was in corroboration with the current findings. With respect to the difference in patient journey between genders in India, the medical expertsunanimously hypothesised that the cultural and social pressures on Indian women maydrive them to seek dermatologists earlier in their journey.
Additionally, a multinational survey involving patient population with an average PASI score of 6.4 concluded that patients with physical and psychological comorbidities, along with visibly affected body areas and itch, had lower QoL, and augmented work impairment.41 Similar results were reported in German and Taiwanese clinical settings where restricted QoL had the greatest effect on daily activities and occupational scales.42,43 Likewise for an Indian setting, a study with 56.2% male patients reported restriction in daily activities in 90.6% of the patients, followed by work impairment in 84.4% of the patients. The overall QoL was hampered in 70% of the patients.44
Psoriasis causes a huge impact on the psychosocial well-being of the patients despite therapeutic interventions. It might exacerbate in the form of psychological comorbidities, social and occupational impairment, and interpersonal conflicts, ultimately culminating into clinical implications causing deteriorated QoL.45,46 Another important aspect is that psoriasis not only affects the QoL of patients but also that of the cohabitants (87.8%) who experience impaired QoL and higher levels of anxiety and depression.47
The survey highlights the fact that the use of terms such as scaling in a research survey may lead to a disconnect between a dermatologist and a patient due to the difference in linguistic interpretation. A web-based population survey reported high disease burden, with more than 90% of the patients complaining itching, redness, flaking, and scales along with musculoskeletal symptoms in 63% of the patients. Patients and dermatologists also had different perceptions related to disease severity, treatment goals, and treatment satisfaction.21
A major finding with respect to treatment was that only 19% of the patients with moderate-to-severe psoriasis were aware of biologics; however, Indian dermatologists were found to recommend topical and oral therapies for moderate cases, while combination therapies (not qualified in results section) were reserved for the severe cases.48 A prospective observational study established that a combinatorial approach with topical and systemic therapy is more efficacious with significant improvement in QoL compared with topical alone.24 However, biologics are not used optimally by the Indian dermatologists owing to cost, fear of adverse effects, lack of awareness, and a perception of inadequacy.49 Nonetheless, the global use of biologics in the past decade has significantly changed the treatment algorithm for psoriasis, thereby greatly affecting the treatment choices in a clinical setting.50 Majority of the patients lack awareness and appreciable knowledge about possibility of attaining substantial improvement or elimination of their most troublesome symptoms.36 Patients are often not satisfied with their treatment regimen but are hesitant in communicating this to their dermatologist, thereby arising the need for involving patients in shared decision making throughout their journey.51
An intriguing point to note was a stark difference observed between the perception of patients and dermatologists towards management of psoriasis acting as a barrier to optimum care. This calls for measures to intensify treatment awareness among the patients and improve the counselling time and techniques. It was studied that the awareness related to the QoL of patients amongst the dermatologists could significantly improve the overall patient journey and imbibe a positive outcome within the patients.52 Moreover, psychological counselling and social awareness are the need of the hour to overcome the hurdle of stigmatisation encountered by patients.53 Therefore, a holistic approach encompassing both pharmacological intervention and psychological measures is indispensable for the management of psoriasis.
The present survey comprehensively captured the issue of therapeutic inertia in an Indian scenario and the need to escalate therapy in moderate-to-severe plaque psoriasis patients. However, we do acknowledge certain limitations of the survey. There was scarcity of data in the public domain from Indian perspective, which was a major challenge. The study is a regional representation with limited sample size and patient access was provided by the dermatologists from their pool of patients. Furthermore, emotional aspects that are paramount in determining the therapy and its impact on relationships were not covered. Despite the limitations, this is the first-of-its-kind survey and the value it is adding in Indian context is being looked upon.
The novelty of the study lies in the fact that there is paucity of data in the Indian context to estimate and identify “Therapeutic Inertia” in plaque psoriasis. Hence, it is important to know the barriers for physicians to recommend aggressive therapies, and the gaps between expectation and treatment.
The survey provides a first-hand information on therapeutic inertia in an Indian population and might form a base to conduct future follow-up studies on a broader scale with more profound results. Further, if feasible, the role of patient advocacy groups should be established in such studies. Although the management of psoriasis is contingent on multiple factors such monitoring burden and therapy cost, nevertheless the finding from the study can access the therapeutic inertia over broader effective care paradigm. Due considerations on economic burden of the disease, HEOR (Health Economics & Outcomes Research) tools, and patient-related outcomes are the pressing needs for patient empowerment throughout the treatment journey.
Conclusion
The survey expressed a gap between Indian dermatologists and patients in terms of symptoms presentation, consultation, and treatment expectation. Cumulatively, the emotional and psychological needs of the patients were far from addressed in India. From a dermatologist’s perspective, the key need gaps to be covered in the region are counselling skills, which can contribute to better treatment and compliance. Although cost is an important factor in decision-making, it is imperative to share all the options with the patients to ensure a shared decision-making between the dermatologist and the patient.
Data Sharing Statement
The data that support the findings of this study are available on request from the corresponding author.
Acknowledgments
We would like to acknowledge Rubina Farooqui, Akshay Halepaty and Anusharth Mulay from IQVIA Primary intelligence team for their help in conducting the survey, and Mrigna Malhotra, Bushra Nabi and Yukti Singh from IQVIA, India for their medical writing and editing support. We would like to acknowledge Dr Akshay Desai, Franchise Medical Head, Novartis Healthcare Pvt Ltd India for his editorial support.The medical writing and editorial support were funded by Novartis Healthcare Pvt Ltd.
A part of the study has been presented earlier: Mauiderm Poster (patient findings), EADV Spring symposium Poster (dermatologist’s perspective), IFPA Posters: Zonal and gender trends, EADV Spring Symposium Poster: Biologic usage specific trends.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research has been funded by Novartis Healthcare Pvt Ltd.
Disclosure
Dr Pallavi Kawatra is an employee of Novartis Healthcare Pvt Ltd, India. Dr Murlidhar Rajagopalan reports personal fees from Novartis, during the conduct of the study; is a speaker and advisor for Novartis,Sanofi, Janssen, Pfizer, Sun Pharma, Gracewell, Dr Reddy's Labs, Eli Lilly, Zydus Cadila, Merck Sharpe and Dohme and has received honoraria for lectures. The authors report no other conflicts of interest in this work.
References
1. Griffiths CEM, Armstrong AW, Gudjonsson JE, Barker JN. Psoriasis. Lancet. 2021;397(10281):1301–1315. doi:10.1016/S0140-6736(20)32549-6
2. Parisi R, Iskandar IYK, Kontopantelis E, Augustin M, Griffiths CEM, Ashcroft DM. National, regional, and worldwide epidemiology of psoriasis: systematic analysis and modelling study. BMJ. 2020;369:m1590. doi:10.1136/bmj.m1590
3. Prevalence data. Available from: https://www.globalpsoriasisatlas.org/en/statistics/prevalence-data.
4. Dogra S, Yadav S. Psoriasis in India: prevalence and pattern. Indian J Dermatol Venereol Leprol. 2010;76(6):595–601. doi:10.4103/0378-6323.72443
5. Raychaudhuri SP, Rein G, Farber EM. Neuropathogenesis and neuropharmacology of psoriasis. Int J Dermatol. 1995;34(10):685–693. doi:10.1111/j.1365-4362.1995.tb04653.x
6. Dubertret L, Mrowietz U, Ranki A, et al. European patient perspectives on the impact of psoriasis: the EUROPSO patient membership survey. Br J Dermatol. 2006;155(4):729–736. doi:10.1111/j.1365-2133.2006.07405.x
7. Singh SM, Narang T, Dogra S, Verma AK, Gupta S, Handa S. An analysis of dermatological quality-of-life scores in relation to psychiatric morbidity in psoriasis. Indian Dermatol Online J. 2016;7(3):208–209. doi:10.4103/2229-5178.182371
8. Zachariae H, Zachariae R, Blomqvist K, et al. Quality of life and prevalence of arthritis reported by 5795 members of the Nordic Psoriasis Associations. Data from the Nordic Quality of Life Study. Acta Derm Venereol. 2002;82(2):108–113. doi:10.1080/00015550252948130
9. Suganya Sekar SJD. A clinico-epidemiological study of psoriasis patients with moderate to severe plaque type in tertiary care centre in South India. Int J Res Dermatol. 2021;7(1):1–6.
10. World Health Organization. Global report on psoriasis. World Health Organization; 2016.
11. Fujii R, Mould J, Tang B, et al. PSY46 burden of disease in patients with diagnosed psoriasis in Brazil: results From 2011 National Health and Wellness Survey (NHWS). Value Health. 2012;15(4):A107. doi:10.1016/j.jval.2012.03.580
12. Stern RS, Nijsten T, Feldman SR, Margolis DJ, Rolstad T. Psoriasis is common, carries a substantial burden even when not extensive, and is associated with widespread treatment dissatisfaction. J Investig Dermatol Symp Proc. 2004;9(2):136–139. doi:10.1046/j.1087-0024.2003.09102.x
13. de Korte J, Sprangers MA, Mombers FM, Bos JD. Quality of life in patients with psoriasis: a systematic literature review. J Investig Dermatol Symp Proc. 2004;9(2):140–147. doi:10.1046/j.1087-0024.2003.09110.x
14. Sampogna F, Tabolli S, Abeni D. Living with psoriasis: prevalence of shame, anger, worry, and problems in daily activities and social life. Acta Derm Venereol. 2012;92(3):299–303. doi:10.2340/00015555-1273
15. Nyunt WWT, Low WY, Ismail R, Sockalingam S, Min AKK. Determinants of health-related quality of life in psoriasis patients in Malaysia. Asia Pac J Public Health. 2015;27(2):NP662–NP673. doi:10.1177/1010539513492561
16. Kimball AB, Gieler U, Linder D, Sampogna F, Warren RB, Augustin M. Psoriasis: is the impairment to a patient’s life cumulative? J Eur Acad Dermatol Venereol. 2010;24(9):989–1004. doi:10.1111/j.1468-3083.2010.03705.x
17. Weiss SC, Kimball AB, Liewehr DJ, Blauvelt A, Turner ML, Emanuel EJ. Quantifying the harmful effect of psoriasis on health-related quality of life. J Am Acad Dermatol. 2002;47(4):512–518. doi:10.1067/mjd.2002.122755
18. Moradi M, Rencz F, Brodszky V, Moradi A, Balogh O, Gulácsi L. Health status and quality of life in patients with psoriasis: an Iranian cross-sectional survey. Arch Iran Med. 2015;18(3):153–159.
19. Russo PA, Ilchef R, Cooper AJ. Psychiatric morbidity in psoriasis: a review. Australas J Dermatol. 2004;45(3):
20. Tang MM, Chang CC, Chan LC, Heng A. Quality of life and cost of illness in patients with psoriasis in Malaysia: a multicenter study. Int J Dermatol. 2013;52(3):314–322. doi:10.1111/j.1365-4632.2011.05340.x
21. Lebwohl M, Langley RG, Paul C, et al. Evolution of patient perceptions of psoriatic disease: results from the Understanding Psoriatic Disease Leveraging Insights for Treatment (UPLIFT) survey. Dermatol Ther. 2022;12(1):61–78. doi:10.1007/s13555-021-00635-4
22. Mrowietz U, Kragballe K, Reich K, et al. Definition of treatment goals for moderate to severe psoriasis: a European consensus. Arch Dermatol Res. 2011;303(1):1–10. doi:10.1007/s00403-010-1080-1
23. Gisondi P, Del Giglio M, Girolomoni G. Treatment approaches to moderate to severe psoriasis. Int J Mol Sci. 2017;18(11):2427. doi:10.3390/ijms18112427
24. Karamata VV, Gandhi AM, Patel PP, Sutaria A, Desai MK. A study of the use of drugs in patients suffering from psoriasis and their impact on quality of life. Indian J Pharmacol. 2017;49(1):84–88. doi:10.4103/ijp.IJP_166_16
25. Rendon A, Schäkel K. Psoriasis pathogenesis and treatment. Int J Mol Sci. 2019;20(6):1475. doi:10.3390/ijms20061475
26. Balogh EA, Bashyam AM, Ghamrawi RI, Feldman SR. Emerging systemic drugs in the treatment of plaque psoriasis. Expert Opin Emerg Drugs. 2020;25(2):89–100. doi:10.1080/14728214.2020.1745773
27. Kim WB, Jerome D, Yeung J. Diagnosis and management of psoriasis. Can Fam Physician. 2017;63(4):278–285.
28. Rajagopalan M, Chatterjee M, De A, et al. Systemic management of psoriasis patients in Indian scenario: an expert consensus. Indian Dermatol Online J. 2021;12(5):674–682. doi:10.4103/idoj.IDOJ_113_21
29. Armstrong AW, Foster SA, Comer BS, et al. Real-world health outcomes in adults with moderate-to-severe psoriasis in the United States: a population study using electronic health records to examine patient-perceived treatment effectiveness, medication use, and healthcare resource utilization. BMC Dermatol. 2018;18(1):4. doi:10.1186/s12895-018-0072-2
30. Ghislain P-D, Lambert J, Hoai X-L-L, et al. Real-life effectiveness of apremilast for the treatment of psoriasis in Belgium: results from the observational OTELO study. Adv Ther. 2022;39(2):1068–1080. doi:10.1007/s12325-021-01981-7
31. Gupta AK, Pandey SS, Pandey BL. Effectiveness of conventional drug therapy of plaque psoriasis in the context of consensus guidelines: a prospective observational study in 150 patients. Ann Dermatol. 2013;25(2):156–162. doi:10.5021/ad.2013.25.2.156
32. Sator P. Safety and tolerability of Adalimumab for the treatment of psoriasis: a review summarizing 15 years of real-life experience. Ther Adv Chronic Dis. 2018;9(8):147–158. doi:10.1177/2040622318772705
33. Rajagopalan M, Dogra S, Saraswat A, Varma S, Banodkar P. The use of apremilast in psoriasis: an Indian perspective on real-world scenarios. Psoriasis. 2021;11:109–122. doi:10.2147/PTT.S320810
34. Augustin M, Krüger K, Radtke MA, Schwippl I, Reich K. Disease severity, quality of life and health care in plaque-type psoriasis: a multicenter cross-sectional study in Germany. Dermatology. 2008;216(4):366–372. doi:10.1159/000119415
35. Krueger G, Koo J, Lebwohl M, Menter A, Stern RS, Rolstad T. The impact of psoriasis on quality of life: results of a 1998 National Psoriasis Foundation patient-membership survey. Arch Dermatol. 2001;137(3):280–284.
36. Strober BE, van der Walt JM, Armstrong AW, et al. Clinical goals and barriers to effective psoriasis care. Dermatol Ther (Heidelb). 2019;9(1):5–18. doi:10.1007/s13555-018-0279-5
37. Phillips LS, Branch JWT, Cook CB, et al. Clinical inertia. American College of Physicians; 2001.
38. Halioua B, Corgibet F, Maghia R, et al. Therapeutic inertia in the management of moderate-to-severe plaque psoriasis. J Eur Acad Dermatol Venereol. 2020;34(1):e30–e32. doi:10.1111/jdv.15882
39. Halioua B. Therapeutic inertia in psoriasis management. Available from: https://www.psoriasiscouncil.org/2019_eadv_congress_report.htm#Therapeutic%20inertia%20in%20psoriasis%20management.
40. Armstrong AW, Robertson AD, Wu J, Schupp C, Lebwohl MG. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: findings from the National Psoriasis Foundation surveys, 2003–2011. JAMA Dermatol. 2013;149(10):1180–1185. doi:10.1001/jamadermatol.2013.5264
41. Griffiths CEM, Jo SJ, Naldi L, et al. A multidimensional assessment of the burden of psoriasis: results from a multinational dermatologist and patient survey. Br J Dermatol. 2018;179(1):173–181. doi:10.1111/bjd.16332
42. Langenbruch A, Radtke MA, Jacobi A, et al. Quality of psoriasis care in Germany: results of the national health care study “PsoHealth3”. Arch Dermatol Res. 2016;308(6):401–408. doi:10.1007/s00403-016-1651-x
43. Yang H-J, Yang K-C. Impact of psoriasis on quality of life in Taiwan. Dermatologica Sin. 2015;33(3):146–150. doi:10.1016/j.dsi.2015.02.001
44. Manjula VD, Sreekiran S, Saril PS, Sreekanth MP. A study of psoriasis and quality of life in a tertiary care teaching hospital of kottayam, Kerala. Indian J Dermatol. 2011;56(4):403–406. doi:10.4103/0019-5154.84767
45. Kolli SS, Amin SD, Pona A, Cline A, Feldman SR. Psychosocial impact of psoriasis: a review for dermatology residents. Cutis. 2018;102(5S):21–25.
46. Bhosle MJ, Kulkarni A, Feldman SR, Balkrishnan R. Quality of life in patients with psoriasis. Health Qual Life Outcomes. 2006;4(1):35. doi:10.1186/1477-7525-4-35
47. Martínez-García E, Arias-Santiago S, Valenzuela-Salas I, Garrido-Colmenero C, García-Mellado V, Buendía-Eisman A. Quality of life in persons living with psoriasis patients. J Am Acad Dermatol. 2014;71(2):302–307. doi:10.1016/j.jaad.2014.03.039
48. Psoriasis clinical guideline. Available from: https://www.aad.org/member/clinical-quality/guidelines/psoriasis.
49. Neema S, Dabbas D, Radhakrishnan S, Yadav AK. Pattern of use of biologics in psoriasis among Indian dermatologists – a cross sectional survey. 2021:1–4Indian J Dermatol Venereol Leprol. doi:10.25259/IJDVL_1006_19
50. Kamiya K, Oiso N, Kawada A, Ohtsuki M. Epidemiological survey of the psoriasis patients in the Japanese Society for Psoriasis Research from 2013 to 2018. J Dermatol. 2021;48(6):864–875. doi:10.1111/1346-8138.15803
51. Huang Y-H, Chiu T-M, Ho J-C, et al. Patient’s perception and importance of clear/almost clear skin in moderate-to-severe plaque psoriasis: results of clear about psoriasis survey in Taiwan. Dermatologica Sin. 2019;37(1):12–18. doi:10.4103/ds.ds_28_18
52. Darjani A, Heidarzadeh A, Golchai J, et al. Quality of life in psoriatic patients: a study using the short form-36. Int J Prev Med. 2014;5(9):1146–1152.
53. Jankowiak B, Kowalewska B, Krajewska-Kułak E, Khvorik DF. Stigmatization and quality of life in patients with psoriasis. Dermatol Ther. 2020;10(2):285–296. doi:10.1007/s13555-020-00363-1
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
