Back to Journals » Journal of Pain Research » Volume 12
Therapeutic Efficacy and the Impact of the “Dose” Effect of Acupuncture to Treat Sciatica: A Randomized Controlled Pilot Study
Authors Liu CH , Kung YY , Lin CL, Yang JL , Wu TP , Lin HC, Chang YK, Chang CM, Chen FP
Received 31 March 2019
Accepted for publication 29 November 2019
Published 31 December 2019 Volume 2019:12 Pages 3511—3520
DOI https://doi.org/10.2147/JPR.S210672
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Ching-Hsiung Liu,1,2 Yen-Ying Kung,2–4 Chun-Liang Lin,1 Jen-Lin Yang,2–4 Ta-Peng Wu,3 Hong-Chun Lin,3 Yang-Kai Chang,3 Ching-Mao Chang,2–4 Fang-Pey Chen2,3
1Department of Neurology, Lotung Poh-Ai Hospital, Ilan, Taiwan, Republic of China; 2Institute of Traditional Medicine, School of Medicine, National Yang-Ming University, Taipei, Taiwan, Republic of China; 3Center for Traditional Medicine, Taipei Veterans General Hospital, Taipei, Taiwan, Republic of China; 4Faculty of Medicine, School of Medicine, National Yang-Ming University, Taipei, Taiwan, Republic of China
Correspondence: Fang-Pey Chen
Institute of Traditional Medicine, School of Medicine, National Yang-Ming University, and Director, Center for Traditional Medicine, Taipei Veterans General Hospital, Number 155, Section 2, Linong Street, Taipei 112, Taiwan, Republic of China
Tel +8862-2875-7454
Fax +8862-2875-7452
Email [email protected]
Purpose: To investigate the required sample size for and feasibility of a full-scale randomized controlled trial examining the impact of the “dose” effect of acupuncture in treating sciatica.
Patients and methods: Fifty-seven patients with sciatica, aged 35–70 years, were recruited and screened. Thirty-one participants were randomly assigned to receive “low-dose” manual acupuncture (MAL) (n= 15) or “high-dose” manual acupuncture (MAH) (n=16). The acupuncture treatment was administered twice weekly for 4 weeks. The primary outcome was the visual analog scale (VAS) score at baseline and after 4 weeks of acupuncture treatment. Secondary outcomes included the Roland Disability Questionnaire for Sciatica (RDQS), the Sciatica Bothersomeness Index (SBI), and the World Health Organization Quality of Life in the Brief Edition (WHOQOL-BREF) scores at baseline and after 4 weeks of acupuncture treatment.
Results: Thirty patients completed the study. For all patients, acupuncture achieved significant improvement in the VAS (5.48±2.0, p<0.001), RDQS (3.18±2.83, p=0.004), and SBI (2.85±3.23, p=0.008) scores, but not in the WHOQOL-BREF scores. In the between-group analysis, the assessed scales showed no significant differences between the MAL and MAH groups. However, based on the level of chronicity, the MAH group demonstrated greater improvement in the outcomes and a significant benefit in the physical subscale of the WHOQOL-BREF (p<0.05).
Conclusion: Results of this pilot study indicate that acupuncture is safe and may effectively relieve symptoms and disability in patients with non-acute sciatica. MAL was as effective as MAH in treating sciatica. A subsequent trial with a larger sample size (estimated at n=96) is required to confirm whether patients with a high level of chronicity would benefit from MAH treatment.
Trial registration: NCT03489681.
Keywords: acupoints, alternative medicine, chronic pain, low back pain, analgesia, noninvasive treatment
Introduction
Sciatica is a common and bothersome medical problem. It typically presents as unilateral gluteal pain that may involve one leg in association with motor or sensory disturbances. Chronic sciatica may cause personal morbidity and negatively impact an individual’s quality of life (QOL).1,2 The prevalence of sciatica varies among studies, with incidences of 24–40% for different etiologies.3,4 The most common cause of sciatica is a herniated or bulging lumbar intervertebral disc.5 Other nondiscogenic causes that may contribute to sciatica include bony or muscular compression, vascular anomalies, and epidural adhesion.6 Owing to the diverse origins of sciatica, the most effective treatment for sciatica remains unknown. A recently published guideline (National Institute for Health and Care Excellence [NICE]7) for treating low back pain with or without sciatica suggests administering noninvasive treatments such as physical therapy, yoga, tai chi, or nonsteroidal anti-inflammatory drugs for first-line management of the condition.7 However, the NICE guidelines do not suggest patients with sciatica receive acupuncture treatment due to the relatively low-quality evidence from randomized controlled trials.
Acupuncture has been proposed as a treatment resulting in better outcomes8 for many muscular and neurological diseases such as fibromyalgia, migraines, chronic pain syndrome, and acute stroke.9–13 Acupuncture maneuvers may elicit a sensation of “de qi” (ie, dull pain, soreness or needling sensation) to achieve analgesia: neural signals are transferred through the peripheral nociceptive pathway, leading to a central neuromodulatory effect.14,15
Nevertheless, there are several debates surrounding acupuncture treatment because there is inadequate evidence to promote its routine use.7,12 Some clinical trials and meta-analyses have recently contributed more evidence regarding acupuncture treatment for sciatica.16–18 He et al, in their study of post-partum sciatica, revealed that up to 98% of patients in the treatment group recovered, compared with 24% in the non-acupuncture control group.16 Zhang et al showed electroacupuncture had greater short- and long-term benefits for chronic discogenic sciatica than medium-frequency electrotherapy.17 Qiu et al also demonstrated that acupuncture may stimulate the sciatic nerve trunk and effectively relieve pain in patients with discogenic sciatica.18 Moreover, acupuncture may reduce sciatica pain intensity, increase the pain threshold,19 enhance the effects of drug, and improve outcomes.20,21 The benefits of acupuncture in treating sciatica are well known; however, the possible dose-related response has not been sufficiently explored.22,23
Considering that acupuncture is more effective in treating sciatica than traditional treatments; we investigated the dose effect of acupuncture and observed the impact of pain chronicity. We hypothesized that, if acupuncture therapy is effective for pain relief in chronic sciatica, the number of acupoints (ie, dosage) may have a crucial role in pain relief. We also investigated the efficacy of acupuncture in treating sciatica and the impact of pain duration on treatment outcome.
Patients and Methods
Study Design
This randomized, prospective study enrolled consecutive patients who fulfilled the inclusion criteria. The study was approved by the institutional review board of the Taipei Veterans General Hospital (Taipei, Taiwan) in accordance with the Helsinki Declaration. All patients provided written informed consent. The trial is registered in the US National Institutes of Health trials registry at http://clinicaltrials.gov (registration No. NCT03489681).
The study comprised two parallel arms: (1) the “low-dose” manual acupuncture (MAL) treatment group, which involved six acupoints, and (2) the “high-dose” manual acupuncture (MAH) treatment group, which involved 18 acupoints. All patients received 4 weeks of treatment, twice weekly, for a total of eight sessions of acupuncture treatment. All patients were surveyed using behavioral scales at baseline and 4 weeks after initiating acupuncture treatment.
Patients
Outpatients who met the inclusion criteria were recruited for this study. The selection criteria were: 35–70 years of age, low back or gluteal pain that radiated to one leg, and pain lasting at least 2 weeks. To meet the inclusion/diagnosis criteria, participants had to fulfill least two of the following items: (1) radicular pain in the L4, L5, or S1 dermatome; (2) physical examination results consistent with radicular pain, motor or sensory neurological findings, or decreased reflex in the L4, L5, or S1 spinal nerve roots; (3) positive results on a straight-leg-raise test; (4) increased leg pain upon coughing, sneezing, or straining; and (5) magnetic resonance imaging demonstrating a unilateral disc herniation impinging on the L4, L5, or S1 nerve roots. The exclusion criteria were: history of or suspected serious spinal pathology (eg, cauda equina syndrome or spinal fracture); pregnant or breastfeeding; scheduled or being considered for spinal surgery or interventional procedures for sciatica during the 8-week treatment period; comorbid systemic malignancy, bleeding tendency, rheumatic arthritis, or other known autoimmune diseases; focal neurological deficits with progressive or disabling symptoms; acupuncture treatment within the previous month; contraindications for acupuncture or magnetic resonance imaging; visual analogue scale (VAS) score <3 for sciatica; and low back pain without sciatica.
Randomization Procedures
Patients were randomized using permuted blocks of four with stratification. The generated code was sealed in an envelope until informed consent was obtained. Patients were randomly allocated to the MAL group or the MAH group. The research assistant opened the sealed envelope before the patient’s first acupuncture treatment in the study.
Intervention
Experienced acupuncturists (n = 2) were allocated to alternatively administer treatment to patients in the MAL and MAH groups. Patients in the MAL group received treatment on six acupoints, as follows: Shenshu (BL 23), Huantiao (GB 30), Weizhong (BL 40), Yanglingquan (GB 34), Kunlun (BL 60), and Xuanzhong (GB 39). Patients in the MAH group received 18 acupoints as follows: Shenshu (BL 23), Dachangshu (BL 25), Xiaochangshu (BL 27), Huantiao (GB 30), Yinmen (BL 37), Zhibian (BL 54), Chengfu (BL 36), Fengshi (GB 31), Weizhong (BL 40), Zusanli (ST 36) Yanglingquan (GB 34), Yinlingquan (SP 9), Feiyang (BL 58), Sanyinjiao (SP 6), Xuanzhong (GB 39), Kunlun (BL 60), Taixi (KI 3), and Shenmai (BL 62). Acupoint selection was based on previous treatment experience and traditional Chinese medicine (TCM) theory, all selected points were practically effective for treatment.24 We also took into consideration sciatica dermatomes when choosing acupoints.
Sterile disposable 0.3 mm × 40 mm or 0.35 mm × 50 mm (diameter × length) stainless steel needles (Ching Ming Medical Device Co, Taipei, Taiwan, ROC) were used. Needles were used only once and were generally inserted to a depth of 5–30 mm, depending on the acupoint. Insertion was followed by manual stimulation to elicit the “de qi” sensation. Needles were retained in position for 20–30 mins.
Outcome Measures
The primary outcome was the 10-cm VAS score for sciatica, which was measured at baseline and week 4. The patients rated their average leg pain over the previous 24 hrs from 0 (ie, “no leg pain”) to 10 (ie, “worst pain imaginable”).25,26
There were several secondary outcomes. The Roland Disability Questionnaire for Sciatica (RDQS) score,1,27 measured at baseline and week 4, was used to assess functional disability; the scores ranged from 0 (ie, “no disability”) to 24 (ie, “most disability”) with higher values indicating worse outcomes. The Sciatica Bothersomeness Index (SBI) was used to rate leg pain and other bothersome symptoms such as paresthesia and weakness, with scores ranging from 0 (ie, “not bothersome”) to 24 (ie, “extremely bothersome”); higher symptom scores were associated with higher emotional distress and lower physical function.28,29 The World Health Organization Quality of Life in the Brief Edition (WHOQOL-BREF) was scored at baseline and at week 4 to evaluate medical outcomes and QOL. Higher scores indicated a better QOL. The WHOQOL-BREF had four subscales: (1) physical domain (score range, 4–20); (2) psychological domain (score range, 4–20); (3) social domain (score range, 4–20); and (4) environmental domain (score range, 4–20). The total score ranged from 8 to 80 points, with higher values indicating better outcomes.30
During the acupuncture treatment period, the investigative team monitored safety. The physicians and nursing team recorded patients’ vital signs and monitored them for any discomfort. The participants recorded unexpected events that occurred during treatment.
Statistical Analysis
Data are presented as the mean ± standard deviation (SD). We used the Shapiro–Wilk test to determine whether the data exhibited a normal distribution. We used the χ2 test to determine whether the nominal variables were comparable. Between-group differences were assessed using the independent t-test or the nonparametric Mann–Whitney U-test, based on the normality test findings. The primary and secondary outcome results were analyzed using univariate analysis of variance (ANOVA). We also applied repeated-measures ANOVA to examine changes over time in the primary and secondary outcomes. To assess the improvement rate, we used the independent t-test to compare changes in scores from baseline to 4 weeks after acupuncture treatment. IBM SPSS software v20.0 (Armonk, New York, USA) was used for all statistical analyses. A value of p<0.05 was considered statistically significant, and p<0.1 represented a statistical tendency toward a significant difference.
Results
Participants
From December 2017 to January 2019, 280 patients were assessed for eligibility. Of these, 57 patients were screened (22 men, 35 women). Twenty-six patients (11 men, 15 women) were excluded for the following reasons: declined to participate (n=8); had low back pain only (n=5); had major cardiovascular disease (n=1); VAS score <3 (n=4); acupuncture treatment within the preceding month (n=2); immunocompromised status (n=1); acute sciatica (n=3); fear of acupuncture (n=1), and history of lumbosacral operation (n=1). Of the remaining 31 patients, 16 were allocated to the MAH group, and 15 to the MAL group (Figure 1). After one dropout, 30 participants were included in the study (11 men and 19 women).
Baseline Characteristics
The average age of all recruited participants was 58.73±12.14 years. The average sciatica pain duration was 25.67±23.67 months. The average baseline VAS, SBI, RDQS, and WHOQOL-BREF scores were 6.09±1.73, 13.33±5.12, 10.60±4.64, and 53.97±8.27, respectively (Table S1). The effectiveness of acupuncture treatment did not seem to differ between the sexes (Table S2). The mean age was 63.20±8.20 years in the MAH group and 54.27±14.97 years in the MAL group (p=0.042). Sex, lateralization of sciatica, and pain duration did not differ significantly between the two groups. The intergroup baseline scores were not significantly different (Table 1).
 |
Table 1 Clinical Characteristics at Baseline and During the Treatment Phase in the Different Dose Groups |
VAS Score
Based on the within-group analysis of changes from the baseline values in each group, the VAS scores for the MAL and MAH groups were significantly reduced after 4 weeks of acupuncture treatment (from 5.90±1.74 to 3.94±2.51, p<0.05 [MAL]; from 6.29±1.76 to 4.00±1.95, p <0.005 [MAH]). On combining the two groups, the VAS score changed from 6.09±1.73 at baseline to 3.97±2.21 after initiating acupuncture treatment (p=0.000; Table 1). However, there were no significant differences between the VAS scores of the MAH and MAL groups at 4 weeks (Table1).
Other Outcomes
The SBI and RDQS scores for all participants were significantly different after acupuncture treatment (p<0.05; Table S1). Only the MAL group had a significant improvement in SBI and RDQS scores (p<0.05; Table 1 and Figure 2). WHOQOL-BREF scores did not differ significantly within either group.
Sample-Size Calculation
The SD values of the primary end point (VAS) were used to calculate the sample size for a future definitive trial using G*Power V.3.1.9.2 (Heinrich-Heine University of Dusseldorf, Düsseldorf, Germany). The change in VAS score between baseline and 4 weeks was selected as the most suitable primary outcome for sample-size calculation. The mean square of the residual of the VAS scores of all patients after baseline VAS score adjustment was estimated to be 2.52, which was converted to an SD of 1.66. Assuming this degree of variance, 42 patients per group would be required to detect an effect size of 0.55 at a 5% significance level with 80% power. To allow for an 18% loss to follow-up (based on our results), a full-scale study would require 96 patients in total.
Acupuncture Effect on the Chronicity of Pain
Subgroup analysis was used to assess the patients completed the study, based on pain duration: the nonchronic pain (NCr) group patients (n= 14) had a pain duration of ≤12 months; the chronic pain (Cr) group patients (n= 16) had a pain duration of >12 months. Nearly all outcome measure scales were “severe” before acupuncture in the Cr group when compared with those of the NCr group (Table 2). There were significant differences in the scores of the WHOQOL-BREF and its subscales (Figure 3A and B). After acupuncture treatment, the between-group difference (ie, NCr vs Cr) showed a decreasing trend (Table 3 and Figure 3C). With regard to the effect of dose on chronicity, the physical subscale of the WHOQOL-BREF significantly improved in the Cr group after MAH (Figure 3D).
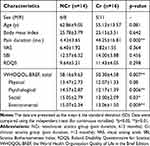 |
Table 2 Clinical Characteristics at Baseline in Groups with Differing Chronicity |
 |
Table 3 Clinical Outcomes After Acupuncture in Groups with Differing Chronicity |
Adverse Events
No serious adverse events occurred. One patient in the MAL group felt transient dizziness during acupuncture.
Discussion
The present study aimed to investigate the effectiveness of acupuncture therapy on chronic sciatica, the dose effect of acupuncture, and the influence of pain chronicity on acupuncture treatment outcome. First, we observed whether acupuncture was effective in patients with sciatica who received MAL or MAH. Second, we found that the efficacy of acupuncture treatment on sciatica was not lesser in the MAL group than in the MAH group. Third, the analysis of sciatica pain chronicity revealed that patients who had sciatica for more than 12 months had inferior scores for pain or disability than patients who had sciatica for less than 1 year. Fourth, we demonstrated that acupuncture may ameliorate differences between groups with different levels of pain chronicity, and we further specified that MAH may enhance physical activity in patients with a relatively longer pain duration.
The results of this study indicated that, in patients with chronic sciatica, acupuncture therapy was effective for pain relief, reduced disability, and alleviated annoyance due to sciatica. Our results are in line with those of recent clinical trials and meta-analyses.16,19,20,31 In our previous review of common acupoints for treating sciatica,24 the acupoints selected were primarily in the bladder (BL) and gallbladder (GB) meridians, as well as the Governing Vessels and Kidney (KI) meridians, which, based on TCM theory, may nourish the patient’s qi. Our acupoint selection for treating sciatica was based on TCM theory and took into account a concept in contemporary medicine: the dermatome. Sciatica primarily involves the L4 and L5 to S1 dermatomes.2,32 The BL and GB meridians are mostly distributed in the L4, L5, and S1 dermatomes, and the KI, stomach (ST) and spleen (SP) meridians are generally distributed in the L4 and S1 dermatomes. Recent research reveals that acupuncture stimulation in the sciatic nerve trunk is more effective in relieving pain compared with simple routine acupuncture.18 Our strategy for choosing acupoints seems to reflect the efficacy of acupuncture treatment for sciatica.
The concept of acupuncture “dose” is varied and generally includes needling depth, intensity, “de qi” sensation, and treatment frequency.33–35 The Delphi Consensus on the assessment of the quality of acupuncture declared that treatment components such as the number of needles, type of stimulation, retention time, and number of treatments all contribute to the “dose” of acupuncture.36 In the current study, we used number of needles (ie, acupoints) applied to the ipsilateral meridians in the same dermatomes of the sciatic nerve to characterize the dosage of acupuncture and found that MAL was as efficient as MAH after 8 sessions of acupuncture treatment, which is line with a previous study on the “dose” of acupuncture for treating a painful cervical myofascial syndrome.37 Similar dose-finding studies reveal that changing in modes of stimulation such as whether to apply manual stimulation and the frequency of manipulation did not result in significant differences in the treatment of fibromyalgia or menstrual pain, respectively.33,38 However, a meta-analysis on treating primary dysmenorrhea with acupuncture showed that needle location, number of needles used, and frequency of treatment may have dose–response relationships with menstrual pain outcomes.23 A contradictory dose–response relationship can be attributed to the variable aspect of the “dose” of acupuncture, which involves both the physiological effects of needling and a patient’s perception.35
Chronic pain involves multidimensional aspects such as biological, psychological, and social facets that determine a patient’s experience of pain.39 The chronicity of pain may be associated with clinicians’ inability to manage pain effectively.40 Our study did not reveal a difference in treating sciatica in the MAL group or MAH group; nevertheless, we tried to specify further whether the dose–response relationship may be correlated with the chronicity of pain.
Our results demonstrated that the Cr group had significantly lower scores on the WHOQOL-BREF and its physical, social, and environmental subscales than the NCr group. Acupuncture may enhance QOL in multifaceted ways and narrow the gap between groups of individuals with different levels of chronicity. With regard to the dose–response effect, the MAH group demonstrated a significant improvement in the physical subscale of WHOQOL-BREF when compared with the MAL group.
In the previous research, the stage of chronicity was an important attribution of psychological vulnerability for pain-related disability,41 and higher stages of chronicity require a multidisciplinary treatment strategy to provide a benefit.42 In our study, MAH involved more acupoints/meridians (ie, BL, GB, ST, and SP) than MAL (ie, BL and GB). This factor may ensure that individuals receiving MAH achieve a greater multilevel therapeutic benefit from peripheral nociception to the central analgesic effect of the brain.43
This study demonstrates a dose–response relationship of acupuncture for treating sciatica and presents a relationship between MAH and the stage of chronicity. A potential implication of our results is that, in treating chronic pain, acupuncturists may choose different dosages (ex, six vs. 18 acupoints) according to the pain chronicity of the patients.
However, there are some limitations to our study. Acupuncture in clinical trials cannot be conducted with a double-blind design, and using sham needles has a placebo effect.44,45 In the current study, we did not assign a placebo group because of ethical reasons and because we wanted to observe the dose-response in real-world acupuncture practice. Moreover, our study did not has blinded observers to measure treatment outcomes because pain or disability for sciatica is relative to each patient, and the questionnaire could be filled out only by the patients. Furthermore, as the study involved a relatively small sample size, further research with a larger sample size is needed to investigate the impact of acupuncture “dose” on the level of pain chronicity in multidimensional aspects of pain perception.
Conclusion
Results of this prospective, randomized, controlled, pilot study suggests that acupuncture is safe and effective for relieving symptoms and disability in patients with non-acute/chronic sciatica. MAL is as effective as MAH in treating chronic sciatica. MAH treatment seems superior to MAL treatment for sciatica patients with a higher stage of chronicity. However, more extensive case-control studies with larger sample sizes are needed to confirm with better certainty a dose–response relationship and the impact on chronicity.
Abbreviations
MAL, “low-dose” manual acupuncture; MAH, “high-dose” manual acupuncture; VAS, visual analog scale; RDQS, Roland Disability Questionnaire for Sciatica; SBI, Sciatica Bothersomeness Index; WHOQOL-BREF, World Health Organization Quality of Life in the Brief Edition; QOL, quality of life; NICE, National Institute for Health and Care Excellence; TCM, traditional Chinese medicine; SD, standard deviation; ANOVA, analysis of variance.
Data Sharing Statement
Data will not be shared for the research is still in progress.
Acknowledgments
This work was supported by the Taipei Veterans General Hospital (Taipei, Taiwan; grant No. V107C-058) and in part by the Lotung Poh-Ai Hospital (Ilan, Taiwan) and the Lo-Hsu Foundation grant (grant No. 10605-E235). This work was particularly supported by the “Development and Construction Plan” of the School of Medicine (107F-M01-07M32) at National Yang-Ming University.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kim M, Guilfoyle MR, Seeley HM, Laing RJ. A modified Roland-Morris disability scale for the assessment of sciatica. Acta Neurochir. 2010;152(9):
2. Stirling ER, Patel MS, Sell PJ. Sciatica. Br J Hosp Med. 2016;77(11):C180–C183. doi:10.12968/hmed.2016.77.11.C180
3. Korovessis P, Repantis T, Zacharatos S, Baikousis A. Low back pain and sciatica prevalence and intensity reported in a Mediterranean country: ordinal logistic regression analysis. Orthopedics. 2012;35(12):e1775–e1784. doi:10.3928/01477447-20121120-24
4. Konstantinou K, Dunn KM. Sciatica: review of epidemiological studies and prevalence estimates. Spine. 2008;33(22):2464–2472. doi:10.1097/BRS.0b013e318183a4a2
5. Davis D, Vasudevan A. Sciatica. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from http://www.ncbi.nlm.nih.gov/books/NBK507908/
6. Stafford MA, Peng P, Hill DA. Sciatica: a review of history, epidemiology, pathogenesis, and the role of epidural steroid injection in management. Br J Anaesth. 2007;99(4):461–473. doi:10.1093/bja/aem238
7. Bernstein IA, Malik Q, Carville S, Ward S. Low back pain and sciatica: summary of NICE guidance. BMJ. 2017;356:i6748. doi:10.1136/bmj.i6748
8. Birch S, Lee MS, Alraek T, Kim TH. Overview of treatment guidelines and clinical practical guidelines that recommend the use of acupuncture: a bibliometric analysis. J Altern Complement Med. 2018;24(8):752–769. doi:10.1089/acm.2018.0092
9. Deare JC, Zheng Z, Xue CC, et al. Acupuncture for treating fibromyalgia. Cochrane Database Syst Rev. 2013;5:Cd007070.
10. Yang Y, Que Q, Ye X, Zheng G. Verum versus sham manual acupuncture for migraine: a systematic review of randomised controlled trials. Acupunct Med. 2016;34(2):76–83. doi:10.1136/acupmed-2015-010903
11. Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172(19):1444–1453. doi:10.1001/archinternmed.2012.3654
12. Yang A, Wu HM, Tang JL, Xu L, Yang M, Liu GJ. Acupuncture for stroke rehabilitation. Cochrane Database Syst Rev. 2016;8:Cd004131.
13. Liu CH, Hsieh YT, Tseng HP, et al. Acupuncture for a first episode of acute ischaemic stroke: an observer-blinded randomised controlled pilot study. Acupunct Med. 2016;34(5):349–355. doi:10.1136/acupmed-2015-010825
14. Omura Y. Patho-physiology of acupuncture treatment: effects of acupuncture on cardiovascular and nervous systems. Acupuncture Electrother Res. 1975;1(1–2):51–141.
15. Cao X. Scientific bases of acupuncture analgesia. Acupuncture Electrother Res. 2002;27(1):1–14. doi:10.3727/036012902816026103
16. He BS, Li Y, Gui T. Preliminary clinical evaluation of acupuncture therapy in patients with postpartum sciatica. J Midwifery Womens Health. 2018;63(2):214–220. doi:10.1111/jmwh.12681
17. Zhang X, Wang Y, Wang Z, Wang C, Ding W, Liu Z. A randomized clinical trial comparing the effectiveness of electroacupuncture versus medium-frequency electrotherapy for discogenic sciatica. Evid Based Complement Alternat Med. 2017;2017:9502718. doi:10.1155/2017/9502718
18. Qiu L, Hu XL, Zhao XY, et al. A randomized controlled clinical trial of treatment of lumbar disc herniation-induced sciatica by acupuncture stimulation of sciatic nerve trunk. Zhen Ci Yan Jiu. 2016;41(5):447–450.
19. Fernandez M, Ferreira PH. Acupuncture for sciatica and a comparison with Western medicine (PEDro synthesis). Br J Sports Med. 2017;51(6):539–540. doi:10.1136/bjsports-2016-096203
20. Qin Z, Liu X, Wu J, Zhai Y, Liu Z. Effectiveness of acupuncture for treating sciatica: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2015;2015:425108. doi:10.1155/2015/425108
21. Ji M, Wang X, Chen M, Shen Y, Zhang X, Yang J. The efficacy of acupuncture for the treatment of sciatica: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2015;2015:192808. doi:10.1155/2015/192808
22. Zhao L, Chen J, Liu C-Z, et al. A review of acupoint specificity research in China: status quo and prospects. Evid Based Complement Alternat Med. 2012;2012:16. doi:10.1155/2012/543943
23. Armour M, Smith CA. Treating primary dysmenorrhoea with acupuncture: a narrative review of the relationship between acupuncture ‘dose’ and menstrual pain outcomes. Acupunct Med. 2016;34(6):416–424. doi:10.1136/acupmed-2016-011110
24. Liu C-H, Chen F-P. Therapeutic approach of acupuncture for sciatica: a brief review. Neuropsychiatry. 2017;7(2):149–155. doi:10.4172/Neuropsychiatry.1000191
25. Huskisson EC. Measurement of pain. Lancet. 1974;2(7889):1127–1131. doi:10.1016/S0140-6736(74)90884-8
26. Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: what is moderate pain in millimetres? Pain. 1997;72(1–2):95–97. doi:10.1016/S0304-3959(97)00005-5
27. Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8(2):141–144. doi:10.1097/00007632-198303000-00004
28. Grovle L, Haugen AJ, Keller A, Natvig B, Brox JI, Grotle M. The bothersomeness of sciatica: patients’ self-report of paresthesia, weakness and leg pain. Eur Spine J. 2010;19(2):263–269. doi:10.1007/s00586-009-1042-5
29. Grovle L, Haugen AJ, Natvig B, Brox JI, Grotle M. The prognosis of self-reported paresthesia and weakness in disc-related sciatica. Eur Spine J. 2013;22(11):2488–2495. doi:10.1007/s00586-013-2871-9
30. Yao G, Wu CH. Factorial invariance of the WHOQOL-BREF among disease groups. Qual Life Res. 2005;14(8):1881–1888. doi:10.1007/s11136-005-3867-7
31. Tang S, Mo Z, Zhang R. Acupuncture for lumbar disc herniation: a systematic review and meta-analysis. Acupunct Med. 2018;36(2):62–70. doi:10.1136/acupmed-2016-011332
32. Gore S, Nadkarni S. Sciatica: detection and confirmation by new method. Int J Spine Surg. 2014;8:15. doi:10.14444/1015
33. Harris RE, Tian X, Williams DA, et al. Treatment of fibromyalgia with formula acupuncture: investigation of needle placement, needle stimulation, and treatment frequency. J Altern Complement Med. 2005;11(4):663–671. doi:10.1089/acm.2005.11.663
34. Paterson C. Patients’ experiences of Western-style acupuncture: the influence of acupuncture ‘dose’, self-care strategies and integration. J Health Serv Res Policy. 2007;12 Suppl 1:
35. White A, Cummings M, Barlas P, et al. Defining an adequate dose of acupuncture using a neurophysiological approach – a narrative review of the literature. Acupunct Med. 2008;26(2):111–120. doi:10.1136/aim.26.2.111
36. Smith CA, Zaslawski CJ, Zheng Z, et al. Development of an instrument to assess the quality of acupuncture: results from a Delphi process. J Altern Complement Med. 2011;17(5):441–452. doi:10.1089/acm.2010.0457
37. Ceccherelli F, Marino E, Caliendo A, Dezzoni R, Roveri A, Gagliardi G. 3,5,11 needles: looking for the perfect number of needles – a randomized and controlled study. Acupunct Electrother Res. 2014;39(3–4):241–258. doi:10.3727/036012914X14109544776097
38. Armour M. The role of treatment timing and mode of stimulation in the treatment of primary dysmenorrhea with acupuncture: an exploratory randomised controlled trial. PLoS One. 2017;12:7. doi:10.1371/journal.pone.0180177
39. Rajapakse D, Liossi C, Howard RF. Presentation and management of chronic pain. Arch Dis Child. 2014;99(5):474. doi:10.1136/archdischild-2013-304207
40. Wang CK, Myunghae Hah J, Carroll I. Factors contributing to pain chronicity. Curr Pain Headache Rep. 2009;13(1):7–11. doi:10.1007/s11916-009-0003-3
41. Sullivan MJ, Sullivan ME, Adams HM. Stage of chronicity and cognitive correlates of pain-related disability. Cogn Behav Ther. 2002;31(3):111–118. doi:10.1080/165060702320337988
42. Buchner M, Neubauer E, Zahlten-Hinguranage A, Schiltenwolf M. The influence of the grade of chronicity on the outcome of multidisciplinary therapy for chronic low back pain. Spine. 2007;32(26):3060–3066. doi:10.1097/BRS.0b013e31815cde5a
43. Zhao ZQ. Neural mechanism underlying acupuncture analgesia. Prog Neurobiol. 2008;85(4):355–375. doi:10.1016/j.pneurobio.2008.05.004
44. Chae Y, Lee YS, Enck P. How placebo needles differ from placebo pills? Front Psychiatry. 2018;9:243. doi:10.3389/fpsyt.2018.00243
45. Vickers AJ, Vertosick EA, Lewith G, et al. Acupuncture for chronic pain: update of an individual patient data meta-analysis. J Pain. 2018;19(5):455–474. doi:10.1016/j.jpain.2017.11.005
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



