Back to Journals » International Journal of General Medicine » Volume 15
The Widowhood Effect on Mortality in Older Patients with Hip Fracture
Authors Zhu Z, Wang Z, Wu Y, Chen X, Liu H, Zhang J, Liu M, Liu Y
Received 3 August 2022
Accepted for publication 27 September 2022
Published 7 October 2022 Volume 2022:15 Pages 7693—7700
DOI https://doi.org/10.2147/IJGM.S384862
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Zhonglun Zhu,1,* Zhicong Wang,1,2,* Yuxuan Wu,1,* Xi Chen,1 Hailong Liu,1 Jianjun Zhang,1 Mozhen Liu,2 Yuehong Liu1
1Department of Orthopedics, People’s Hospital of Deyang City, Deyang, People’s Republic of China; 2Department of Orthopedics, The First Affiliated Hospital of Dalian Medical University, Dalian, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yuehong Liu, Department of Orthopedics, People’s Hospital of Deyang City, Deyang, People’s Republic of China, Email [email protected]
Objective: Widowed people have increased mortality than married people of the same age, a phenomenon known as the widowhood effect. This study aimed to investigate whether this effect exists in older patients with hip fracture.
Methods: Using our own hip fracture database, a total of 1101 hip fracture patients were consecutively included from January 2014 to December 2021. Marital status was stratified as married (n = 793) and widowed (n = 308). Patients survival status was obtained from medical records or telephone follow-ups, and the outcomes were all-cause mortality at 30 days, 1 year and at latest follow-up. Univariate and multivariate Cox proportional hazard models were used to assess the association between marital status and mortality, and subgroup analyses according to sex were also conducted.
Results: Compared with married patients, widowed patients were more likely to be older, female and intertrochanteric fracture, and were less likely to be urban area, smoking, drinking, and surgical treatment (P < 0.05). After a median follow-up of 37.1 months, the 30-day mortality was 4.3% (n = 47), 1-year mortality was 19.3% (n = 178), and total mortality was 34.2% (n = 376). Multivariate Cox analysis showed that widowed marital status remained an independent risk factor for 1-year mortality (HR = 1.437, 95% CI: 1.054– 1.959, P = 0.022), and total mortality (HR = 1.296, 95% CI: 1.038– 1.618, P = 0.022), whereas this association was not found in 30-day mortality (HR = 1.200, 95% CI: 0.607– 2.376, P = 0.599). Moreover, subgroup analyses also found that the widowhood effect on mortality was present in both male and female.
Conclusion: Widowed marital status seems to be an independent risk factor for long-term mortality in older patients with hip fracture.
Keywords: widowhood, mortality, hip fracture, older adults
Introduction
With an increasingly ageing society, spousal loss or widowhood has become a common phenomenon.1 In UK, more than 2 million older adults over 65 years were widowed, with an incidence of 23.4% in 2020.2 In China, the number of the widowed older adults was estimated to be 47.7 million, which accounted for 26.9% of the older population.3
Widowhood is one of the most stressful life events that negatively influences the mental health of the older people, including loneliness,4 anxiety,5 depression6 and cognition.7 As a result, widowed people have poorer physical health and higher mortality than married people of the same age, a phenomenon known as the widowhood effect.8–10 A meta-analysis of 15 prospective cohort studies involving more than 2.2 million people reported a 12.0% higher risk of mortality in widowed versus married persons.11 To date, this effect has been confirmed in the general population,8–10,12–14 as well as patients with cardiovascular disease,15 stroke16 and cancer.17 Although China has a large number of widowed people, most of these prior studies were conducted in Western countries.4 Given the differences in culture, dietary habits and lifestyles between Western countries and China, it is still unclear whether the widowhood effect exists in Chinese population, although this effect has been confirmed in Asian populations.18
Hip fracture is a common injury among older adults, resulting in substantial excess short- and long-term mortality.19 Most recently, two network meta-analyses including over 100 randomized controlled trails have showed that the 1-year mortality rates were as high as 23.5% and 20.2% in patients with intracapsular and extracapsular hip fracture, respectively.20,21 This increased mortality risk persisted for more than two decades after hip fracture.22 Due to the advanced age of hip fracture patients, the prevalence of widowhood is relatively high, such as 46.2% in Sweden,23 43.1% in USA,24 42.6% in Denmark,25 and 39.2% in Norway.26 For this reason, we hypothesized that widowed marital status might be associated with increased mortality of older patients with hip fracture. To date, only a few studies have examined the association between widowhood and mortality in hip fracture patients.23,24,27,28 Despite this, half of them showed this relationship,27,28 while the other half did not.23,24 Therefore, using the data from our own hip fracture database,29 we aimed to investigate the effect of widowhood on all-cause mortality in older patients with hip fracture.
Methods
Study Design and Patients
This was a single-center, observational study that was conducted using our own hip fracture database, which focused on the prognosis of hip fracture patients.29 Briefly, a total of 1240 hip fracture patients aged ≥ 60 years have been consecutively entered into the database from January 2014 to December 2021. At admission, all patient were asked about their marital status, which was classified into four categories: married, unmarried, widowed, and divorced. In this study, patients who were unmarried, divorced, or lost to follow-up were excluded from the analyses. The patient selection flowchart is shown in Figure 1. This retrospective study was approved by the Institutional Ethics Committee of People’s Hospital of Deyang City (Review No. 2022-04-040-K01), and was conducted according to the Declaration of Helsinki. Written informed consent was obtained from all participants at admission, and oral informed consent was completed during telephone follow-up.
 |
Figure 1 A flow diagram of the selection process. |
Data Collection
As described previously,29 data were extracted from the clinical database, including age, sex, residence address, smoking and drinking history, Charlson comorbidity index (CCI), hip fracture type, and surgery treatment. Specifically, age was categorized by 10-year age groups as 60–69, 70–79 and ≥ 80 years. Residence was classified as urban or rural areas according to the patients’ addresses. On the basis of the smoking and drinking history, smoking and drinking status was defined as either current (yes) or not current (no). CCI is widely used for comorbidity assessment, and has been validated as a predictor of mortality in hip fracture patients.30 Based on a prior study, CCI was categorized as none (CCI = 0), low (CCI = 1), or high (CCI ≥ 2).26 Hip fracture type was confirmed by X-ray and/or computed tomography, and classified as femoral neck fracture or intertrochanteric fracture. Most of patients were surgically treated with percutaneous cannulated screw fixation, intramedullary nail fixation, or hip replacement (yes), and the remaining patients were classified as undergoing nonoperative management (no).
Follow-Up and Outcome
After discharge, all surviving patients were followed up annually by telephone interviews. The follow-up contents included survival status, cause of death and time of death. For patients who died in hospital, we obtained the death information from their hospital medical records. Survival time was defined as the time from hospital admission to death or last follow-up (January 31, 2022), whichever occurred first. The outcomes of interest were all-cause mortality at 30 days, 1 year and at latest follow-up. To ensure follow-up of at least 1 year, only patients between January 2014 and December 2020 were included in the 1-year mortality analysis.
Statistical Analysis
Continuous variable (age) was first assessed by the Shapiro–Wilk normality test, and reported as mean ± standard deviation (SD), and categorical variables were reported as numbers (percentages). Differences between groups were compared with Student’s t-test or chi-square test, as appropriate. Survival analysis was performed using Kaplan-Meier survival curve and the Log rank test. Cox proportional hazard regression models were used to identify the factors associated with 30-day, 1-year and total mortality. Model 1 was unadjusted (crude model), model 2 was adjusted for significant variables (P < 0.10) in model 1, and model 3 was further adjusted for all variables (fully adjusted model). The hazard ratio (HR) and 95% confidence interval (CI) were calculated. The proportional hazard assumption was assessed with Schoenfeld residuals. Previous meta-analysis indicated that the widowhood effect on mortality was significant for men but not for women,11 therefore, subgroup analyses according to sex were made. All analyses were conducted using JMP Pro software (version 16.0.0; SAS Institute Inc., Cary, NC, USA), and P < 0.05 was considered statistically significant.
Results
Patient Characteristics
Ultimately, 1101 patients were included in the final analysis, and patient characteristics are presented in Table 1. Among these patients, more than half were older than 80 years (53.7%), and almost two thirds were female (66.4%), and the majority lived in an urban area (60.9%). A total of 16.0% of patients were current smokers, 10.4% were drinkers, 21.3% had a high comorbidity level, 52.0% were intertrochanteric fracture, and 72.4% underwent surgical treatment. In terms of the marital status, 72.0% were married, and 28.0% were widowed. Compared with married patients, widowed patients were more likely to be older, female and intertrochanteric fracture, and were less likely to be urban area, smoking, drinking, and surgical treatment (P < 0.05).
 |
Table 1 Patient Characteristics Stratified by Marital Status |
All-Cause Mortality
After a median follow-up of 37.1 months, 376 patients died from any cause. Overall, the 30-day mortality was 4.3% (n = 47), 1-year mortality was 19.3% (n = 178), and total mortality was 34.2%. Compared with married patients, widowed patients suffered higher 1-year mortality (24.6% vs 17.2%, P = 0.010), and total mortality (41.2% vs 31.4%, P = 0.002), but the difference in mortality at 30 days did not reach statistical significance (4.2% vs 4.3%, P = 0.961). Kaplan-Meier survival curve also showed that widowed patients had significantly worse survival than married patients (log-rank χ2 = 11.220, P < 0.001, Figure 2).
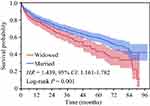 |
Figure 2 Kaplan-Meier survival curve for all-cause mortality stratified by marital status. |
Risk Factors Associated with Mortality
As shown in Table 2, univariate Cox regression analysis revealed that marital status, age, sex, CCI score and surgery were associated with 1-year mortality (Model 1). After adjusting for these variables, widowed marital status remained an independent risk factor for 1-year mortality (HR = 1.477, 95% CI: 1.085–2.010, P = 0.013; Model 2). Further adjustment for all variables did not change the result (HR = 1.437, 95% CI: 1.054–1.959, P = 0.022; Model 3). Meanwhile, age, sex, CCI score and surgery were significantly associated with 1-year mortality (P < 0.05). Consistent with this finding, subgroup analysis also showed that the widowhood effect on 1-year mortality was present in both male (HR = 1.328, 95% CI: 1.013–1.741, P = 0.040) and female (HR = 1.728, 95% CI: 1.179–2.532, P = 0.005).
 |
Table 2 Cox Regression Analysis for the Risk Factors Associated with 1-Year All-Cause Mortality |
The association between widowed marital status and mortality was slightly attenuated with the duration of follow-up, but remained independently associated with total mortality in Model 2 (HR = 1.256, 95% CI: 1.012–1.558, P = 0.039) and Model 3 (HR = 1.296, 95% CI: 1.038–1.618, P = 0.022; Table 3). Moreover, age, CCI score and surgery were significantly associated with total mortality (P < 0.05). Also, the widowhood effect on total mortality for male (HR = 1.282 95% CI: 1.004–1.636, P = 0.046) and female (HR = 1.409, 95% CI: 1.086–1.829, P = 0.010) was observed in a subgroup analysis.
 |
Table 3 Cox Regression Analysis for the Risk Factors Associated with Total All-Cause Mortality |
However, univariate and multivariate Cox regression analysis revealed that there was no association between widowed marital status and 30-day mortality (P = 0.949 in Model 1, P = 0.685 in Model 2, P = 0.599 in Model 3; Supplementary Table 1).
Discussion
Widowhood is a common phenomenon in older adults, and has been identified as a risk factor for fall.31 Many of these falls lead to fractures, a recent analysis of up to 1.7 million individuals found that widows and widowers had a 1.34-fold and 1.32-fold higher risk of hip fracture than married persons.32 Other studies also showed an increased risk of hip fracture after spousal loss.25,33 In turn, hip fracture patients tend to be older, thereby, the incidence of widowhood is expected to be high. In this study, the prevalence of widowhood was 28.0%. Although this was much higher than a survey conducted in China (6.6%),27 it was still lower than that in Western countries.23–26
As is well known, hip fracture is associated with substantial excess mortality.19 We found that the 30-day, 1-year and total all-cause mortality rates were 4.3%, 19.3% and 34.2%, respectively. Due to the high mortality, we were able to explore the association between widowed marital status and mortality based on a relatively small sample size. The results showed that widowed patients suffered higher 1-year mortality and total mortality. Further adjustment for all variables, widowed marital status remained an independent risk factor for 1-year mortality (HR = 1.437, 95% CI: 1.054–1.959), and total mortality (HR = 1.296, 95% CI: 1.038–1.618). Furthermore, subgroup analyses also found that the widowhood effect on mortality was present in both male and female. In line with our findings, Zeng et al27 analyzed 210,450 patients from a large national database, and reported that hip fracture patients who were widowed exhibited higher mortality than married patients after hip arthroplasty (HR = 1.3, 95% CI: 1.0–1.7). Zhou et al28 also reported that the 1-year mortality rate was significantly higher in unmarried hip fracture patients than in married patients (30.8% vs 13.9%). When compared with married hip fracture patients, another study found that widowed patients were more likely to undergo a preoperative transthoracic echocardiogram, and had a longer time to surgery. For this reason, the authors suggested that the use of preoperative noninvasive cardiac testing may lead to delays in surgery, thereby contributing to worse outcomes in hip fracture patients.24 On the other hand, widowed hip fracture patients had a lower persistence on antiosteoporosis drugs.34 This might be another reason for the high mortality in widowed patients. However, there was also study that found no obvious differences between widowed and married hip fracture patients with regard to medical complications, hip complications and mortality, but the associations were close to statistical significance.23
Moreover, age, sex, CCI score and surgery were found to be significantly associated with mortality in hip fracture patients, which have been previously reported.35 However, most of these factors were inherent or unmodifiable. After spousal loss, widows and widowers often disengage from or restrict their social networks, leading to social isolation. Widowed elderly individuals who have children were found to be more likely to show higher level of satisfaction with life.3 A result from a nationwide cohort study showed that having children was associated with a longer survival after hip fracture. The authors suggested that adult children may support their ageing parents with hip fracture, thereby potentially increasing survival chances.36 In China, older patients with hip fracture are mainly cared for by their adult children in the acute phase after injury. This may be an explanation for no association between widowed marital status and 30-day mortality. In another study, hip fracture patients who lived alone had a higher mortality than those living with a partner.37 These results implied that continuous support by their families may be an important strategy for reducing mortality for the widowed hip fracture patients. Indeed, family caregivers have been confirmed to be an essential component of recovery after hip fracture by providing emotional and physical support.38
However, several limitations should be acknowledged. First, like many other studies in this field,15 marital status was assessed at the time of inclusion, thus change in marital status, such as the duration of widowhood and remarriage during the follow-up was not accounted for. Yet, the prevalence of remarriage was extremely low (1.9%) among Chinese old population.4 Second, some important socioeconomic variables that could not be obtained from our database which may have influenced the results, such as education, income and occupation. As mentioned by Blanner et al,8 it was not possible to meaningfully adjust for educational level or latest employment status due to the age range of the study population. Also, a recent study showed that income and education did not have a significant effect on medical complications, hip complications and mortality after hip fracture surgery.23 Third, the small sample size in this study might limit the statistical power of the analysis. Four, 110 patients (8.9%) were lost to follow-up, although no difference was observed between follow-up and lost to follow-up patients in patient characteristics (Supplementary Table 2). Finally, all patients were retrospectively identified from our institutional database, hence selection bias inevitably existed. To overcome these limitations, more prospective studies with large sample sizes are needed to confirm our findings.
Conclusions
Widowed marital status seems to be an independent risk factor for long-term mortality in older patients with hip fracture. Given the high prevalence of widowhood, it is necessary to pay more attention to its negative impacts on older patients with hip fracture, including high risks of subsequent hip fracture,25,32,33 complications,23 and mortality.27,28 This also implies that social and familiar support, especially their adult children, may be important to improve prognosis.3,36
Data Sharing Statement
The data used during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This retrospective study was approved by the Institutional Ethics Committee of People’s Hospital of Deyang City (Review No. 2022-04-040-K01), and was conducted according to the Declaration of Helsinki. Written informed consent was obtained from all participants at admission, and oral informed consent was completed during telephone follow-up.
Acknowledgments
We would like to thank several nurses from the Department of Orthopedics in People’s Hospital of Deyang City, for the help with the data inspection.
Funding
This study was supported by Sichuan Science and Technology Program (2020YFS0520), and Scientific Research Project of Sichuan Medical Association (S21029).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Hsiao YH, Lee MC, Yeh CJ, Tai CJ, Lee SS. Social participation and survival in widowed persons: results of the Taiwan Longitudinal Study on aging. Int J Environ Res Public Health. 2021;18:10974. doi:10.3390/ijerph182010974
2. Hill D. Population estimates by marital status and living arrangements, England; 2021. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesbymaritalstatusandlivingarrangementsengland.
3. Yang C, Sun X, Duan W. Widowhood and life satisfaction among Chinese elderly adults: the influences of lifestyles and number of children. Front Public Health. 2021;9:754681. doi:10.3389/fpubh.2021.754681
4. Yang F, Gu D. Widowhood, widowhood duration, and loneliness among older adults in China. Soc Sci Med. 2021;283:114179. doi:10.1016/j.socscimed.2021.114179
5. Blanner Kristiansen C, Kjær JN, Hjorth P, Andersen K, Prina AM. Prevalence of common mental disorders in widowhood: a systematic review and meta-analysis. J Affect Disord. 2019;245:1016–1023. doi:10.1016/j.jad.2018.11.088
6. Jadhav A, Weir D. Widowhood and depression in a cross-national perspective: evidence from the United States, Europe, Korea, and China. J Gerontol B Psychol Sci Soc Sci. 2018;73:e143–e153. doi:10.1093/geronb/gbx021
7. Wu-Chung EL, Leal SL, Denny BT, Cheng SL, Fagundes CP. Spousal caregiving, widowhood, and cognition: a systematic review and a biopsychosocial framework for understanding the relationship between interpersonal losses and dementia risk in older adulthood. Neurosci Biobehav Rev. 2022;134:104487. doi:10.1016/j.neubiorev.2021.12.010
8. Blanner C, Mejldal A, Prina AM, Munk-Jørgensen P, Ersbøll AK, Andersen K. Widowhood and mortality: a Danish nationwide register-based cohort study. Epidemiol Psychiatr Sci. 2020;29:e149. doi:10.1017/S2045796020000591
9. Caputo J, Li P, Kühn M, Brønnum-Hansen H, Oksuzyan A. Immigration background and the widowhood effect on mortality. J Gerontol B Psychol Sci Soc Sci. 2021;76:2155–2168. doi:10.1093/geronb/gbab090
10. Manvelian A, Sbarra DA. Marital status, close relationships, and all-cause mortality: results from a 10-year study of nationally representative older adults. Psychosom Med. 2020;82:384–392. doi:10.1097/PSY.0000000000000798
11. Moon JR, Kondo N, Glymour MM, Subramanian SV. Widowhood and mortality: a meta-analysis. PLoS One. 2011;6:e23465. doi:10.1371/journal.pone.0023465
12. Liu H, Umberson D, Xu M. Widowhood and mortality: gender, race/ethnicity, and the role of economic resources. Ann Epidemiol. 2020;45:69–75.e61. doi:10.1016/j.annepidem.2020.02.006
13. Ytterstad E, Brenn T. Mortality after the death of a spouse in Norway. Epidemiology. 2015;26:289–294. doi:10.1097/EDE.0000000000000266
14. Moon JR, Glymour MM, Vable AM, Liu SY, Subramanian SV. Short- and long-term associations between widowhood and mortality in the United States: longitudinal analyses. J Public Health. 2014;36:382–389. doi:10.1093/pubmed/fdt101
15. Schultz WM, Hayek SS, Samman Tahhan A, et al. Marital status and outcomes in patients with cardiovascular disease. J Am Heart Assoc. 2017;6:e005890. doi:10.1161/JAHA.117.005890
16. Dupre ME, Lopes RD. Marital history and survival after stroke. J Am Heart Assoc. 2016;5:e004647. doi:10.1161/JAHA.116.004647
17. Huang L, Peng S, Sun C, et al. Impact of marital status on survival in patients with stage 1A NSCLC. Aging. 2022;14:770–779. doi:10.18632/aging.203838
18. Leung CY, Huang HL, Abe SK, et al. Association of marital status with total and cause-specific mortality in Asia. JAMA Netw Open. 2022;5:e2214181. doi:10.1001/jamanetworkopen.2022.14181
19. Katsoulis M, Benetou V, Karapetyan T, et al. Excess mortality after Hip fracture in elderly persons from Europe and the USA: the CHANCES project. J Intern Med. 2017;281:300–310. doi:10.1111/joim.12586
20. Lewis SR, Macey R, Stokes J, Cook JA, Eardley WG, Griffin XL. Surgical interventions for treating intracapsular Hip fractures in older adults: a network meta-analysis. Cochrane Database Syst Rev. 2022;2:Cd013404. doi:10.1002/14651858.CD013404.pub2
21. Lewis SR, Macey R, Lewis J, et al. Surgical interventions for treating extracapsular Hip fractures in older adults: a network meta-analysis. Cochrane Database Syst Rev. 2022;2:Cd013405. doi:10.1002/14651858.CD013405.pub2
22. von Friesendorff M, McGuigan FE, Wizert A, et al. Hip fracture, mortality risk, and cause of death over two decades. Osteoporos Int. 2016;27:2945–2953. doi:10.1007/s00198-016-3616-5
23. Hansson S, Bülow E, Garland A, Kärrholm J, Rogmark C. More Hip complications after total Hip arthroplasty than after hemi-arthroplasty as Hip fracture treatment: analysis of 5815 matched pairs in the Swedish Hip Arthroplasty Register. Acta Orthop. 2020;91:133–138. doi:10.1080/17453674.2019.1690339
24. Sinvani L, Mendelson DA, Sharma A, et al. Preoperative noninvasive cardiac testing in older adults with Hip fracture: a multi-site study. J Am Geriatr Soc. 2020;68:1690–1697. doi:10.1111/jgs.16555
25. Hansen L, Judge A, Javaid MK, et al. Social inequality and fractures-secular trends in the Danish population: a case-control study. Osteoporos Int. 2018;29:2243–2250. doi:10.1007/s00198-018-4603-9
26. Riska BS, Forsén L, Omsland TK, Søgaard AJ, Meyer HE, Holvik K. Does the association of comorbidity with 1-year mortality after Hip fracture differ according to gender? The Norwegian Epidemiologic Osteoporosis Studies (NOREPOS). J Am Geriatr Soc. 2018;66:553–558. doi:10.1111/jgs.15207
27. Zeng C, Lane NE, Englund M, et al. In-hospital mortality after Hip arthroplasty in China: analysis of a large national database. Bone Joint J. 2019;101-B:1209–1217. doi:10.1302/0301-620X.101B10.BJJ-2018-1608.R1
28. Zhou J, Fu J, Zhao Q, Lin S, Zhu H. Effect of neutrophil-to-lymphocyte ratio on short-term prognosis of elderly patients with Hip fracture. Am J Transl Res. 2021;13:9122–9128.
29. Wang Z, Jiang W, Chen X, Yang L, Wang H, Liu Y. Systemic immune-inflammation index independently predicts poor survival of older adults with Hip fracture: a prospective cohort study. BMC Geriatr. 2021;21:155. doi:10.1186/s12877-021-02102-3
30. Varady NH, Gillinov SM, Yeung CM, Rudisill SS, Chen AF. The Charlson and Elixhauser scores outperform the American Society of Anesthesiologists score in assessing 1-year mortality risk after Hip fracture surgery. Clin Orthop Relat Res. 2021;479:1970–1979. doi:10.1097/CORR.0000000000001772
31. Kim T, Choi SD, Xiong S, Na K-S. Epidemiology of fall and its socioeconomic risk factors in community-dwelling Korean elderly. PLoS One. 2020;15:e0234787. doi:10.1371/journal.pone.0234787
32. Vala CH, Lorentzon M, Sundh V, et al. Increased risk for Hip fracture after death of a spouse-further support for bereavement frailty? Osteoporos Int. 2020;31:485–492. doi:10.1007/s00198-019-05242-w
33. Benetou V, Orfanos P, Feskanich D, et al. Education, marital status, and risk of Hip fractures in older men and women: the CHANCES project. Osteoporos Int. 2015;26:1733–1746. doi:10.1007/s00198-015-3054-9
34. Silverman SL, Siris E, Kendler DL, et al. Persistence at 12 months with denosumab in postmenopausal women with osteoporosis: interim results from a prospective observational study. Osteoporos Int. 2015;26:361–372. doi:10.1007/s00198-014-2871-6
35. Xu BY, Yan S, Low LL, Vasanwala FF, Low SG. Predictors of poor functional outcomes and mortality in patients with Hip fracture: a systematic review. BMC Musculoskelet Disord. 2019;20:568. doi:10.1186/s12891-019-2950-0
36. Meyer AC, Modig K. The role of having children for the incidence of and survival after Hip fracture - a nationwide cohort study. Bone. 2021;145:115873. doi:10.1016/j.bone.2021.115873
37. Dahl C, Holvik K, Meyer HE, et al. Increased mortality in Hip fracture patients living alone: a NOREPOS study. J Bone Miner Res. 2021;36:480–488. doi:10.1002/jbmr.4212
38. Ariza-Vega P, Castillo-Pérez H, Ortiz-Piña M, Ziden L, Palomino-Vidal J, Ashe MC. The journey of recovery: caregivers’ perspectives from a Hip fracture telerehabilitation clinical trial. Phys Ther. 2021;101:pzaa220. doi:10.1093/ptj/pzaa220
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
